Abstract
Background and Objectives
Recent studies have shown that transradial coronary intervention (TRI) is feasible for percutaneous revascularization of chronic total occlusion (CTO). We investigated the feasibility and safety of using a 5-French catheter (5F) TRI for CTO and we compared it with that of using a 6F catheter TRI.
Subjects and Methods
One hundred fifteen patients (117 lesions) who underwent TRI for CTO (TIMI 0 or 1 for more than 2 months) were prospectively registered in this study from April 2002 to July 2004 (54 patients for the 5F and 61 patients for the 6F). The clinical, angiographic and procedural characteristics were evaluated and compared between the 2 groups.
Results
No major difference was noted for the clinical characteristics between the 2 groups. Coronary angiography showed a shorter occlusion length (5F: 8.8±7.6 mm, 6F: 14.7±12.7, p=0.008) and a higher incidence of the tapered type of entry morphology (5F: 74%, 6F: 56%, p=0.042) in the 5F group. A deep-seating technique was used more often in the 5F group (5F: 83%, 6F: 51%, p<0.001). The procedural success rate was similar between the 2 groups (5F: 82%, 6F: 86%, p<0.54). The most common cause of procedural failure for both groups was failure to pass the guidewire. The occlusion duration, lesion length and lesion angulation were the statistically significant predictors of procedural failure. No major procedural or local complication was noted. Minor hematoma occurred in 2 patients and no radial artery occlusion was noted.
With the current improvements of equipment and the increased experience of operators, coronary angioplasty has become an important treatment modality for coronary chronic total occlusion(CTO). Successful recanalization is associated with improvement of the left ventricular function, less mortality and the reduced necessity for performing bypass surgery.1)2)
Recent studies have indicated that transradial coronary intervention(TRI) is feasible for revascularizing CTO.3-5) The major advantages of TRI are reduced bleeding complications, a shorter duration of the hospital stay and the patients' improved comfort.6) A 5-French(5F) guiding catheter approach can further improve the procedure. However, use of a 5F guiding catheter may be limited by a lack of backup support, which may be the critical limitation when performing percutaneous coronary intervention(PCI) for treating CTO. We investigated the feasibility and safety of using a 5F catheter TRI for treating CTO and we compared this with a 6F catheter approach.
One hundred fifteen patients(117 lesions) who underwent TRI for CTO(a TIMI 0 or 1 for more than 2 months) were prospectively included in this study. Any bifurcation lesion requiring the kissing balloon technique was excluded from the study. Fifty-four patients were included in the 5F catheter group, and 63 patients were included in the 6F catheter group.
The prerequisites were a sufficient pulsating radial artery and the presence of an ulnar artery with an adequate palmar arch, as evidenced by the absence of digital ischemia according to the Allen test. Transradial angioplasties were performed with the arm and forearm extended, and with the wrist supine and secured next to the hip. The right radial artery was the preferred approach to keep the procedure simple and the radiation exposure as low as possible. The left radial approach was chosen for the patients with a pathological unilateral Allen test on the right or there was a failure of arterial puncture of the right radial artery, and the left radial approach was also employed for the patients who had undergone coronary bypass surgery with using the left mammary artery. After inducing local anesthesia with 2% lidocaine, the radial artery was cannulated with a 5F or 6F arterial sheath(Check-Flo Performer, Cook, Bloomington, IN). To prevent spasm, 600 µg of nitroglycerin was administered through the arterial sheath. During PCI, the activated coagulation time was kept above 300 seconds via intravenous injection of heparin. After the angioplasty had been performed, the sheath was removed immediately and hemostasis was achieved by applying a radial compressive dressing for 5 hours. The radial artery pulse and bleeding were frequently checked by an experienced nurse.
All the angioplasty procedures(balloon angioplasty and stent implantation) were performed with 5F or 6F guiding catheters(Brite Tip, Cordis, FL, USA). The selection of the guiding catheter's diameter was non-randomized and dependent on the operator's discretion, and a 5F guiding catheter was frequently selected for the low risk patient group. Extra-backup or an Amplatz curve was preferentially selected for a guiding catheter to achieve stronger backup support. A deep-seating technique was actively applied when the backup support of the guiding catheter was inadequate, and this typically occurred in calcified tortuous lesions. To improve the crossibility and to facilitate the exchange of a guidewire, we almost always routinely used a supportive infusion catheter with a guidewire. The initially selected guidewires were High Torque Intermediate(Guidant, USA) or hydrophilic coated guidewires, and these were readily changed to taperedtip stiff guidewires if there was resistance to the wire's progression. Once a guidewire had passed through the occlusion site, a 1.5 mm balloon wire was tried first in the tight fibrotic or calcified lesions. Stent implantation was performed only if the vessel diameter was larger than 2.5 mm.
Procedural success was defined as successful cannulation of the guiding catheter in the coronaries, the post-procedural residual stenosis was <50% and there was TIMI-3 antegrade flow with the absence of major complications(including death, Q-wave myocardial infarction, sustained coronary occlusion or the need for emergency coronary artery bypass surgery).
Vascular access site complications were defined as major if they were associated with a hemoglobin loss greater than 2 g/dL, the need for blood transfusions or vascular repair was done. Minor access site complications were defined as local hematoma >3 cm in diameter, or there was a loss of the radial pulse, suggesting radial occlusion or thrombosis. The duration of occlusion was estimated from the date of occurrence of the myocardial infarction in the area supplied by the occluded vessels, or the abrupt worsening of angina pectoris, or from the information obtained from a previous angiogram.
The angiographic morphology of the occlusion entry was classified as tapered if the occluded segment ended in a funnel-shaped form, or it was classified as abrupt when it did not take this form, or as none when it was impossible to locate the entry site.
The demographic, clinical, angiographic and procedural data was prospectively recorded on a prepared case record form. The coronary angiogram was assessed for lesion location, vessel tortuosity, lesion calcification, the occlusion entry morphology, bridging collaterals and the grade of retrograde collaterals, as based on the Retrop classification.7) Quantitative coronary analysis was also performed for the proximal and distal reference diameters of the vessel, the post-procedural residual stenosis, the lesion length and the occlusion length(these were measured after the passage of a balloon catheter in the success group or estimated by considering the contrast filling of the collaterals in the failure group).
The results are expressed as proportions or means±SDs. The differences in the categorical variables were analyzed by Fisher's exact test, whereas the differences in continuous variables were analyzed by Student's t test. P were less than 0.05 were considered statistically significant.
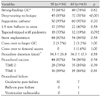
The baseline clinical characteristics of the patients are summarized in Table 1. No major differences were noted between the 2 groups with respect to the distribution of age and gender, the clinical diagnosis of the coronary risk factors, multivessel disease and the left ventricular function. Fifty patients(43%) were treated on a 1-day admission basis; PCI was done on the day of admission and the patients were discharge on the same day(5F: 26(48%), 6F: 24(39%), p=0.34).
The angiographic characteristics of the patients are shown in Table 2. The 5F catheter group was associated with a higher incidence of the tapered type of entry morphology(5F: 74%, 6F: 56%, p=0.04) and shorter occlusion length(5F: 8.8±7.6 mm, 6F: 14.7±12.7 mm, p=0.007). The lesion location, the severity of lesional tortuosity, the lesion calcification and the distribution of the antegrade and collateral flow were similar between the 2 groups. The estimated occlusion duration was also similar between the 2 groups(5F: 17.5‡23.6 months, 6F: 15.3‡18.6 months, p=0.61).
The procedural characteristics for both groups are shown in Table 3. Using a guiding catheter with strong back-up support such as an Amplatz or extra-backup curve was preferred for both the 5F and 6F groups(5F: 61%, 6F: 78%, p=0.82). The deep-seating technique was more frequently applied in the 5F group(5F: 83%, 6F: 51%, p<0.001).
Supportive infusion catheters(Excelsior®, Boston Scientific, MA, USA, or Prowler®, Cordis, FL, USA) were almost routinely used in both groups(5F: 93%, 6F: 97%, p=0.70) Tapered-tipped stiff guidewires(CrossIt 400®, Guidant, USA, or Conquest®, Asahi, Japan) were used in 33% of the 5F group and in 19% of the 6F group (p=0.092).
The crossover to larger guiding catheters or a femoral approach occurred for 2 lesions of the 5F group and for 3 lesions of the 6F group(p=1.0). The duration of the procedure, from starting the guiding catheter cannulation to the end of the procedure, was similar between the 2 groups(5F: 34.3±26.8 min, 6F: 36.7±17.3 min, p=0.58).
The overall procedural success rate was 84%, irrespective of the grade of the antegrade TIMI flow(TIMI 0: 82%, TIMI: 88%, p=0.43). The success rate was similar between the 5F and 6F groups(Table 3). The most frequent cause of procedural failure was the inability to cross the lesion with the guidewire(5F: 10 lesions, 6F: 7 lesions). Among the clinical and angiographic variables, the lesion angulation(>60°), an occlusion duration ≥6 months and a lesion length ≥10 mm were associated with a lower success rate(Table 4).
No major complications such as cardiac tamponade or major hematoma were noted in the study group. No catheter-induced dissections were associated with the deep-seating technique. Coronary artery perforation was noted in 2 patients of the 6F group. These patients were treated with prolonged balloon inflation without further complications. Minor hematoma occurred in 2 patients of the 5F group(Table 5).
This study showed that transradial coronary intervention was feasible and safe with a high success rate and a low complication rate in a selected group of patients with chronic total occlusion. For selected lesions where there was a low risk of failure, a transradial approach with using a small guiding catheter(5F) was also feasible with high success rate that was similar to that with using a 6F catheter TRI.
The transradial approach has been the most popular procedure since Kiemeneij et al reported on similar procedural and clinical outcomes between the transradial, transfemoral and transbrachial accesses for PCIs.8) The advantages of the transradial approach are early ambulation after the procedure and a low local complication rate, and this results in a reduced hospital staff workload, a shorter hospital stay and possibly lower hospital costs.9)10)
Recanalizing CTO may be associated with improved myocardial ischemia, LV remodeling and better function, decreased late cardiac events and possibly with an improved long-term survival rate.1)2) Current improvements in the equipment and the increased operator experience have greatly contributed to the higher success rate of PCI for CTO. The transfemoral approach is the main access site for CTO intervention. The transradial approach is limited by having to use a smaller guiding catheter with less backup support and the inability to perform contralateral injection and several other useful techniques.
However, Saito et al.11) reported a high success rate for the transradial approach to CTO. The success rate was 67% in phase 1 and this improved to 81% in phase 2(from January to August 2001). During phase 2, the success rate was higher for the patients who were treated with transradial coronary intervention rather than with transfemoral coronary intervention(89% vs. 64%; p=0.008), which may indicate that CTO intervention is highly dependent on the experience and technique of the operators. Kelsey et al.12) reported that increased operator experience and improvement in the equipment were directly associated with a high success rate for the procedure. In our study, the overall success rate was 84% and it was similar between the 5F and 6F groups(5F: 82%, 6F: 86%, p=0.54), partly because we had recently accumulated experience with the 5F catheter transradial approach in our catheterization laboratory and the transradial approach for CTO was performed in the relatively low risk patients. The transradial approach was applied to 83.5% of the coronary interventions, among which the 5F approach comprised 48.7% of the transradial approaches during the most recent year.
Patient selection may be the most important factor for obtaining good results when performing CTO intervention. In our series, TIMI 1 flow was noted in 34% of the lesions, and a tapered entry morphology was noted in 64% of the lesions. The tapered entry morphology did not affect the success rate of our study, which compared well with the success rate of the previous studies. We think that the high success rates of performing CTO lesion PCI resulted from the recent improvements of the tapered tip strong guidewires(ex. CrossIt 400®, Guidant, USA, or Conquest®, Asahi, Japan). The occlusion length was 8.8 mm in the 5F group, whereas it was 14.7 mm in the 6F group. However, the success rate was 82% even for lesions with a TIMI flow grade of 0(n=77), and there was no statistical difference between the 5F and 6F groups (5F: 78%, 6F: 85%, p=0.39).
In this study, the feasibility and safety of 5F catheter transradial intervention was specifically tested for CTO intervention. 5F guiding catheters have been recently used in PCI procedures to reduce the local complication rate and patients' discomfort, and particularly for the transradial approach. A smaller guiding catheter is especially useful for patients with small radial arteries.13) Dahm et al reported a lower rate of vascular access complications after using a 5F catheter compared with a 6F catheter for TRI.14) Minor hematoma occurred in 1.1% of the 5F group and in 4.8% of the 6F group(p=0.07). A loss of the radial pulse that was caused by radial occlusion was noted in 1.1% of the 5F group and in 5.9% of the 6F group(p=0.05). In our study, however, the local complication rate was very low and it was not significantly different between the 5F and 6F groups.
A 5F guiding catheter may be associated with lower backup support, compared with a 6F catheter. However, the lack of backup support can be compensated for by aggressively applying the deep-throating technique and using a supportive infusion catheter and tapered-tipped stiff guidewires; this may explain the high success rate of the 5F group in this study.
In this study, lesion angulation, the occlusion length and the occlusion duration were associated with a success rate. Several research groups have reported that the duration of occlusion is predictive of procedural failure.15)16) The longer the duration of the occlusion, the more the lesion is organized with fibrous tissue and the lower the possibility of its recanalization. Kereiakes et al.17) have also shown that the length of occlusion, as judged by determining the extent of retrograde filling from collaterals, is inversely correlated with the procedural success.
The main reason for procedural failure in our study was failure to pass the guidewire(5F, 10 lesions; 6F, 7 lesions), the same as for the transfemoral approach.
The main advantage of the transradial approach is the low incidence of major vascular complications.6) We experienced no major vascular complications. Minor hematoma occurred in 2 patients of the 5F group, and difficult sheath removal was noted in 1 patient of the 6F group.
The limitation of this study is the small number of patients we studied in a non-randomized manner at a single center. The selection of the patients may be different from that of the previous studies, and the operator's experience and preference of procedure are the most important factors influencing the result, and this makes it difficult to generalize the results of this study. Nevertheless, we think this study successfully showed at least the feasibility and safety of using a 5F catheter transradial approach for complex lesion interventions such as chronic total occlusion.
Transradial coronary intervention for treating CTO was feasible and safe with a high success rate and a low complication rate. The 5F catheter transradial approach was also feasible and safe in our selected group of patients with chronic total occlusion, and this may contribute to decreased patient morbidity during percutaneous coronary intervention.
Figures and Tables
References
1. Suero JA, Marso SP, Jones PG, et al. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001. 38:409–414.
2. Noguchi T, Miyazaki S, Morii I, Daikoku S, Goto Y, Nonogi H. Percutaneous transluminal coronary angioplasty of chronic total occlusions: determinants of primary success and long-term clinical outcome. Catheter Cardiovasc Interv. 2000. 49:258–264.
3. Saito S, Tanaka S, Hiroe Y, et al. Angioplasty for chronic total occlusion by using tapered-tip guidewires. Catheter Cardiovasc Interv. 2003. 59:305–311.
4. Kim PH, Gwon HC, Kim YH, et al. The safety and feasibility in trans-radial coronary interventions for chronic total occlusion. Korean Circ J. 2004. 34:767–774.
5. Kim JY, Yoon JH, Jung HS, et al. The experience of transradial coronary intervention for chronic total occlusion. Korean Circ J. 2003. 33:805–812.
6. Kiemeneij F, Laarman GJ, de Melker E. Transradial artery coronary angioplasty. Am Heart J. 1995. 129:1–7.
7. Rentrop KP, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. 1985. 5:587–592.
8. Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches. J Am Coll Cardiol. 1997. 29:1269–1275.
9. Mann T, Cubeddu G, Bowen J, et al. Stenting in acute coronary syndromes: a comparison of radial versus femoral access sites. J Am Coll Cardiol. 1998. 32:572–576.
10. Mann JT, Cubeddu MG, Schneider JE, Arrowood M. Right radial access for PTCA: a prospective study demonstration reduced complications and hospital charges. J Invasive Cardiol. 1996. 8:40D–44D.
11. Saito S, Tanaka S, Hiroe Y, et al. Angioplasty for chronic total occlusion by using tapered-tip guidewires. Catheter Cardiovasc Interv. 2003. 59:305–311.
12. Kelsey SF, Mullin SM, Detre KM, et al. Effect of investigator experience on percutaneous transluminal coronary angioplasty. Am J Cardiol. 1984. 53:56C–64C.
13. Saito S, Ikei H, Hosokawa G, Tanaka S. Influence of the ratio between radial artery inner diameter and sheath outer diameter on radial artery flow after transradial coronary intervention. Cathet Cardiovasc Interv. 1999. 46:173–178.
14. Dahm JB, Vogelgesang D, Hummel A, Staudt A, Volzke H, Felix SB. A randomized trial of 5 vs. 6 French transradial percutaneous coronary interventions. Catheter Cardiovasc Interv. 2002. 57:172–176.
15. Holmes DR, Vlietstra RE, Reeder GS, et al. Angioplasty in total coronary occlusion. J Am Coll Cardiol. 1984. 3:845–849.
16. Melchior JP, Meier B, Urban P, et al. Percutaneous transluminal coronary angioplasty for chronic total occlusion. Am J Cardiol. 1987. 59:535–538.
17. Kereiakes DJ, Selmon MR, McAuley BJ, McAuley DB, Sheehan DJ, Simpson JB. Angioplasty in total coronary artery occlusion: experience in 76 consecutive patients. J Am Coll Cardiol. 1985. 6:526–533.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download