Abstract
Background and Objectives
Sirolimus-eluting stents (SESs) have a considerably lower optimal minimal stent area (MSA) threshold compared to bare metal stents (BMSs). In the SIRIUS IVUS sub study, the absolute optimal stent expansion (OSE) of SESs was described as ≥5.0 mm2. The purpose of this study was to evaluate the impact of the OSE on long-term outcomes following SES implantation using absolute IVUS criteria.
Subjects and Methods
The study included 157 patients (BMS: 57; SES; 100), who underwent 6-month follow-up angiography and 18-month clinical follow-up after bare metal stent or drug-eluting stent (DES) implantation. According to the absolute measurement IVUS criteria, patients were divided into two groups: OSE and non-OSE. The IVUS criteria for OSE were MSA ≥6.5 mm2 for BMS implantation and MSA ≥5.0 mm2 for SES implantation.
Results
Angiographic binary restenosis was higher in the non-OSE than the OSE group with BMS (33.3% vs. 11.4%; p<0.039), but the rates were similar between the two groups with SES (4.5% vs. 3.2%; p=1.00). With the BMS, the MACE rates were 5.7% and 30% in the OSE and non-OSE group, respectively (p=0.017). However, with the SES, the MACE rates were similar between the two groups (OSE group, 3.2% vs. non-OSE group, 4.5%, p=1.00).
Conclusion
After SES implantation, there were no significant differences in the late outcomes in relation to the achievement of absolute OSE. A variety of restenosis related factors should be considered for better outcomes after DES implantation. Therefore, the concept of OSE in the era of DESs might need to be revisited.
Despite the widespread clinical use of intra-coronary stents, angiographic information has potential limitations in providing an accurate assessment of the results of stent procedures. In contrast, intravascular ultrasound (IVUS) can visualize the echoreflective metallic struts, providing comprehensive insights into the vessel and stent geometry.1-4) A number of IVUS studies following coronary stenting have demonstrated the stents frequently under-expanded, despite an adequate angiographic appearance.5) IVUS observations have been the key to defining optimized stent deployment strategies, and have improved the outcomes and techniques of successful stenting.6)
Of these IVUS findings, the minimal stent area(MSA) has been reported as a consistent predictor of ISR and a poor clinical outcome following bare metal stent (BMS) implantation;7-9) therefore, the "bigger is better" theory is likely to be a superior strategy during BMS implantation. In addition, many studies have suggested several IVUS criteria for optimal stent expansion(OSE) using absolute(which was directly measured from the MSA) or relative MSA(the ratio of MSA and reference lumen area) as a predictor of restenosis; the absolute MSA has been reported to be a more reliable predictor of a good outcome.9) Drug-eluting stents(DESs) have recently been introduced into practice, and appear to be a promising approach for the treatment of target lesions.10)11) Because DES can dramatically reduce neointimal proliferation, OSE during DES implantation may have a less important role in determining an improved late outcome. There is little data on the direct relationship between MSA after DES implantation and the long-term angiographic and clinical outcomes. Therefore, the aim of this study was to evaluate and compare the impact of an optimal stent expansion (OSE), as assessed by IVUS, on the angiographic and clinical late outcomes with sirolimus-eluting stents(SESs) compared to BMSs.
From October 2001 until December 2004, 157 patients with 172 de novo coronary lesions who had undergone successful IVUS guided implantation of a single or 2 overlapping stent(s), were included. The BMS group was enrolled between October 2001 and September 2003, and SES group was enrolled between February 2003 and December 2004. All patients were requested to visit the outpatient clinic at 1, 6, 12 and 18 months after the procedure, and agreed to receive 6 to 9-month follow-up coronary angiography. The SES group consisted of 100 patients, with 107 native coronary lesions(73 men and 27 women; mean age: 57±10 years). As controls, 57 patients, with 65 native coronary lesions, who underwent a bare metal stent(BMS) implantation, were included( 37 men and 20 women; mean age: 57±9 years. The written informed consent was obtained from all patients.
Patients were eligible for inclusion if they had: 1) an acute coronary syndrome or stable angina, which required elective percutaneous transluminal coronary angioplasty and stent implantation, 2) de novo target lesions >70% the diameter stenosis, as assessed by quantitative coronary angiographic(QCA) analysis, 3) successful stent implantation resulting in a TIMI III flow, without a dissection, 4) IVUS performed for the assessment of stented segments, as well as the proximal and distal reference segments, 5) a 6 to 9 month follow-up coronary angiogram and a 18-month clinical follow-up and 6) to be above 18 years of age, with a negative pregnancy test, if the patient was female, and had to agree to sign an informed consent. Exclusion criteria included: 1) prior coronary intervention within 6 months, 2) intolerance or a contraindication to aspirin or clopidogrel, 3) advanced heart failure or an ejection fraction under 30%, 4) chronic renal insufficiency or hepatic dysfunction or 5) a major life threatening illness, such as cardiogenic shock.
Coronary angioplasty was performed using the Judkins method, via a femoral or radial approach. The patients were pretreated with aspirin and clopidogrel, and an intravenous bolus dose of weight adjusted heparin(100 U/kg) was given before the procedure. Predilation of the lesion was performed to facilitate stent passage across the lesion. After predilation, the stent size was determined using a digital cardiac imaging system or intravascular ultrasound. Multiple stent implantations were allowed at the discretion of the surgeon. In the DES group, only the sirolimus-eluting stent(Cypher, Cordis Corporation, a Johnson and Johnson Company, Miami Lakes, Florida) was used. However, in the BMS group, Bx Velocity (Cordis Corporation, a Johnson and Johnson Company, Ohio, USA) stents were used in 26 lesions(40.0%), Express( Boston Scientific Corp., Massachusetts, USA) stents in 23 lesions(35.4%) and Arthos (AMG, International GMBH, Raesfeld Erle, Germany) stents in 16 lesions (24.6%). All stents were inflated with a nominal to moderately high pressure using a stent delivery balloon. For the anti-thrombotic regimen, all patients received 100 mg aspirin and 75 mg clopidogrel daily(or cilostazol 100 mg twice daily, for those with an allergic response to clopidogrel) for at least 6 months after a SES implantation, and 1 month after a BMS implantation. The patients also received β-blockers, isosorbide dinitrate and statins at the discretion of the physician.
Data regarding the baseline clinical and angiographic characteristics, interventional procedures and clinical outcomes were obtained from a chart review. Follow-up angiography was performed at 6 to 9 month, with clinical follow-up performed 18 months following stent implantation in both the DES and BMS groups. Clinical follow-up was conducted by telephone contact or office visit. During the follow-up period, major adverse cardiovascular events(MACE), including cardiac death, non-fatal myocardial infarction and target lesion revascularization, were evaluated.
All IVUS studies were performed using a commercially available ultrasound system(Cardiovascular Imaging System/Boston Scientific Corp., San Jose, California). The coronary vessel was imaged using a 2.9 Fr or 3.2 Fr monorail imaging sheath, with a 30-MHz singleelement beveled transducer, rotating at 1,800 rpm. After an intracoronary administration of 200 µg of nitroglycerin, the imaging catheter was positioned at least 5 mm distal to the stent, and withdrawn with an automated pullback device, at 0.5 mm/sec, through the stent at more than 5 mm proximal to the stent. The IVUS images were recorded on a 0.5-in high-resolution s-VHS tape for off-line analysis. There were no procedural or postprocedural in-hospital complications related to the IVUS procedures.
Coronary angiography was performed according to the standard technique. All angiograms were analyzed by a computer-assisted system for a quantitative coronary angiographic analysis(Digital Cardiac Imaging System, Philips Inc, the Netherlands), according to the standard methodology, using end-diastolic frames and a contrast-filled guiding catheter for calibration. Angiographic restenosis was defined as a diameter stenosis ≥50% within the treated site on follow-up.
Quantitative IVUS measurements were obtained within the stented segments and at reference segments 5 mm proximal and distal to the stent edge. The quantitative parameters consisted of: (1) the stent and reference lumen cross-sectional area(CSA), (2) the stent and reference external elastic membrane(EEM) CSAs, and (3) the percentage of plaque burden(%PB). The vessel CSA was measured by tracing the leading edge of the adventitia. The lumen area was measured by tracing the leading edge of the intima before stenting and of the stent after intervention. The percentage of plaque burden was calculated as(vessel CSA-lumen CSA)×100/vessel CSA. The post-intervention minimal stent area was determined as the smallest lumen CSA within the stent, using visual estimation. The CSA in the reference segments was measured at the site of the minimal plaque accumulation, within 5 mm proximal and distal to the lesion. To evaluate the efficacy of the IVUS criteria on the angiographic and late clinical outcomes, the absolute IVUS criteria were used, as recently described.12)13) It was considered that OSE had been achieved when the final MSA was ≥6.5 mm2 after a BMS implantation,12) and ≥5.0 mm2 after a SES implantation.13) All lesions were divided into two groups and then analyzed: when OSE had been achieved, the patients were enrolled into the OSE group, otherwise they were enrolled into the non-OSE group.
Statistical analyses were performed using the SPSS statistical software, version 11.0(SPSS, Inc., Chicago, Illinois). The Student t-test was used to compare the continuous variables, with Chi-squared or Fisher's exact tests used for the categorical variables. Continuous variables are presented as the mean±SD. A p<0.05 was considered statistically significant.
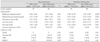
The baseline patient demographics and lesion characteristics are shown in Table 1. The baseline characteristics were similar between the BMS and SES groups. The incidence of diabetes, frequency of patients with multi-vessel disease, lesion complexity and target vessel site were also similar between the BMS and SES groups.
Quantitative angiographic and IVUS results are shown in Table 2. With a BMS, the reference vessel diameter, deployed stent diameter, post-intervention MLD and acute gain were greater in the OSE(MSA ≥6.5 mm2) than the non-OSE group(MSA <6.5 mm2). However, the pre-intervention MLD, lesion lengths, deployed stent lengths and balloon pressures were no different between the two groups. Adjunctive balloon inflation was performed in 8.6% of the OSE group and 13.3% of the non-OSE group(p=0.70). In the IVUS findings, the external elastic membrane(EEM) CSA and lumen CSA in the proximal and distal reference segments were larger in the OSE than the non-OSE group(p<0.001). The MSA was larger in the OSE than the non-OSE group(8.2±1.3 mm2 vs. 5.0±1.0 mm2; p<0.001). With the SES, the reference vessel diameter, deployed stent diameter, post-intervention MLD and acute gain were larger in the OSE(MSA ≥5.0 mm2) than the non-OSE group(MSA<5.0 mm2). The lesion length and deployed stent length were similar between the two groups. The balloon inflation pressure was higher in the OSE than the non-OSE group(16.0 atm vs. 15.1 atm, p=0.011). Adjunctive balloon inflation was performed in 18.0% of the OSE group and 19.3% of the non-OSE group (p=1.00). In the IVUS analysis, the EEM CSA, lumen CSA and MSA were larger in the OSE than the non-OSE group. The MSA was larger in the OSE than the non-OSE group(6.5±1.0 mm2 vs. 3.9±0.8 mm2; p<0.001).
The angiographic and clinical follow-up results are listed in Table 3. With a BMS, there was a trend toward a larger reference vessel diameter and minimal lumen diameter in the OSE compared to the non-OSE group, but without statistical significance. The occurrence of late loss was similar between the two groups. The angiographic restenosis rate was lower in the OSE than the non-OSE group(11.4% vs. 33.3%; p=0.039). The incidences of death and nonfatal myocardial infarction were similar between the two groups. However, the target lesion revascularization was lower in the OSE than the non-OSE group(5.7% vs. 30.0%, p=0.017), which translated into a lower MACE rate in the OSE group (5.7% vs. 30.0%, p=0.017). With a SES, the reference vessel diameter was larger in the OSE than the non-OSE group(3.39±0.38 mm vs. 3.15±0.47 mm, p=0.005). The late loss was 0.31±0.55 mm in the OSE group and 0.38±0.70 mm in the non-OSE group(p=0.56). The minimal lumen diameter was larger in the OSE than the non-OSE group(2.92±0.46 mm vs. 2.55±0.68 mm, p=0.001). The angiographic restenosis rates were 3.2 and 4.5% in the OSE and non-OSE groups, respectively( p=1.00). During the 18 month clinical follow-up, there were no differences in the rates of MACE between the two groups. There was no evidence of acute or subacute thrombosis with a BMS or DES.
IVUS provides more vessel information for determining whether a stent is adequately deployed following implantation. In the BMS era, several studies have demonstrated that the MSA after coronary stenting was a consistent predictor of in-stent restenosis, and was also associated with poor clinical outcomes.7)8)14)15) Hoffmann et al.7) reported that ostial lesion location, IVUS preinterventional plaque burden and post-interventional final lumen dimensions were the most consistent predictors of angiographic in-stent restenosis in 291 patients with 382 lesions. The study by de Feyter et al.8) showed that MSA was inversely related to in-stent restenosis; whereas, the stent length was directly related to in-stent restenosis. In the final results of the CRUISE(Can Routine Ultrasound Influence Stent Expansion) study, a larger MSA was obtained by IVUS-guidance, with a lower target vessel revascularization rate observed in the IVUS-guided group compared to the angiographic guided group.14)
Various IVUS criteria for OSE, mainly the absolute or relative MSA, have been proposed and empirically used in the BMS era. One IVUS study reported that the relative MSA could predict a favorable outcome at follow-up.15) In their study, a MSA ≥55% of the average reference vessel area was associated with a higher probability of freedom from restenosis, independently from the vessel size, in 425 consecutive patients with 496 lesions. However, other IVUS studies have demonstrated that the absolute MSA might be a more reliable predictor for late outcomes.9)13) An IVUS sub study, from a large cohort multi-center trial, demonstrated that an MSA of 6.5 mm2 was the optimal threshold for minimizing target lesion revascularization.13) A similar finding was also supported by one investigating group,9) which suggesting that the absolute MSA (≥7.0 mm2) was the optimal threshold for the reduction of the 6-month angiographic restenosis of the seven IVUS criteria examined. In the current study, the absolute MSA(MSA of ≥6.5 mm2) most likely predicted both lower rates of angiographic restenosis and MACE with a BMS(11.4% vs. 33.3%, p=0.039 for and 5.7% vs. 30.0%, p=0.017, respectively). Based on these observations, a larger MSA may better predict late angiographic and clinical outcomes. Achieving the largest possible post-procedure lumen size could ensure a safety margin for an unexpectedly severe neointimal hyperplasia, which can occasionally follow conventional stenting. Therefore, high pressure stent delivery is required for optimal stent expansion with a BMS.16) However, the question of "How big is big enough?" still remains unsolved, particularly in the era of BMSs.
In the era of DESs, it has been considered if the MSA may be an important predictor of late outcomes, because the drug can substantially inhibit neointimal proliferation.11)17) To date, there have been few reports on IVUS guidelines for optimal DES expansion. One previous study showed that angiographic restenosis increased when the MSA was <5 mm2 in patient treated with a SES.18) An IVUS sub study from the SIRIUS trial demonstrated that if the long-term stent patency was defined as an MSA of >4.0 mm2, then an MSA of ≥5.0 mm2 post-intervention would be the optimal IVUS threshold for long term SES patency in patients receiving a SES.12) In fact, interventional cardiologists are frequently faced with the problem of the MSA being <5.0 mm2 in patients who have small vessel disease or a large plaque burden and/or calcified plaque after a successful SES implantation. In the current study, the rates of angiographic restenosis and MACE were similar between the OSE and non-OSE groups for a SES (p=NS); therefore, the absolute MSA threshold for SES(≥5 mm2) may not be sufficient to predict favorable late outcomes. Furthermore, despite additional evaluation of different MSA cut-off values for OSE, no optimal MSA threshold could be suggested from this study in terms of favorable late outcomes for a SES. A plausible explanation of this result is that the smaller late loss with few MACE at follow-up with a SES may have overcome the safety margin for the biological response of a BMS. Therefore, OSE using the absolute MSA may be less important in late outcomes after DES implantation. However, it may be important for the longterm safety. Stent thrombosis still remains a major concern after DES implantation. Recent studies have reported that the angiographic incidence of stent thrombosis after DES implantation ranged between 0.37% to 1.27% by at least the 1 year follow-up.19)20) Using a multivariate analysis, the predictors for stent thrombosis were cessation of clopidogrel, renal failure, bifurcation lesions and instent restenosis.20)21) Stent under expansion is also associated with stent thrombosis.22)23) Therefore, obtaining an adequate stent dimension an not be disregarded, especially in relation to safety.
In the current study, no case of stent thrombosis was observed for up to 18 months after a SES implantation. It was speculated that all patients had taken at least two different anti-thrombotic medications for up to 12 months after the procedure; however, few clinical events were observed, regardless the OSE status. However, a small number of patients, with relatively short follow-up periods, may underestimate the true incidence of stent thrombosis after DES implantation. Larger numbers of patients, with longer follow-up, will be required to assess stent thrombosis.
The current study has several other limitations. A relatively large coronary vessel, with both BMS and DES, may favorable affect the late outcomes. Also, the reference vessel size in the non-OSE group was less than that in the OSE group, which may have influenced the restenosis gradient in these groups. In fact, patients with small vessel disease have been reported as having a higher rate of restenosis, as well as worse clinical outcomes.24)25) An IVUS study was not conducted at follow-up; therefore, no important IVUS findings, such as late incomplete stent apposition or stent under expansion at follow-up, can be provided. Also, the real neointimal proliferation could not be measured in this study. The BMS and SES groups were not simultaneously enrolled. Therefore, no direct comparison could be undertaken. With a SES, the balloon inflation pressure was higher in the OSE than the non-OSE group, which may have influenced the late outcomes. In the BMS group, the implanted stents were heterogeneous. Finally, the sites of MSA with both stents were determined by visual assessment. A larger randomized prospective study may be required to verify this result.
In conclusion, following SES implantation, the late outcomes did not differ significantly in relation to the achievement of absolute OSE. The outcomes after a DES implantation may be determined using a variety of other restenosis-related factors. Thus, the concept of an OSE might need to be revisited in the era of DESs.
Figures and Tables
Acknowledgments
This work was supported by a grant, No. RTI04-01-01, from the Regional Technology Innovation Program of the Ministry of Commerce, Industry and Energy(MOCIE).
References
1. Colombo A, Hall P, Nakamura S, et al. Intracoronary stenting without anticoagulation accomplished with intravascular ultrasound guidance. Circulation. 1995. 91:1676–1688.
2. Mudra H, Regar E, Klauss V, et al. Serial follow-up after optimized ultrasound-guided deployment of Palmaz-Schatz stents: in-stent neointimal proliferation without significant reference segment response. Circulation. 1997. 95:363–370.
3. von Birgelen C, Gil R, Ruygrok P, et al. Optimized expansion of the Wallstent compared with the Palmaz-Schatz stent: on-line observations with two- and three-dimensional intracoronary ultrasound after angiographic guidance. Am Heart J. 1996. 131:1067–1075.
4. Gorge G, Haude M, Ge J, et al. Intravascular ultrasound after low and high inflation pressure coronary artery stent implantation. J Am Coll Cardiol. 1995. 26:725–730.
5. Goldberg SL, Colombo A, Nakamura S, Almagor Y, Maiello L, Tobis JM. Benefit of intracoronary ultrasound in the deployment of Palmaz-Schatz stents. J Am Coll Cardiol. 1994. 24:996–1003.
6. von Birgelen C, Erbel R. The stent is here to stay: a note on stenting, ultrasound imaging, and the prevention of restenosis. Eur Heart J. 2002. 23:595–597.
7. Hoffmann R, Mintz GS, Mehran R, et al. Intravascular ultrasound predictors of angiographic restenosis in lesions treated with Palmaz-Schatz stents. J Am Coll Cardiol. 1998. 31:43–49.
8. de Feyter PJ, Kay P, Disco C, Serruys PW. Reference chart derived from post-stent-implantation intravascular ultrasound predictors of 6-months expected restenosis on quantitative coronary angiography. Circulation. 1999. 100:1777–1783.
9. Hong MK, Lee CW, Kim JH, et al. Impact of various intravascular ultrasound criteria for stent optimization on the six-month angiographic restenosis. Catheter Cardiovasc Interv. 2002. 56:178–183.
10. Sousa JE, Costa MA, Abizaid AC, et al. Sustained suppression of neointimal proliferation by sirolimus-eluting stents: one-year angiographic and intravascular ultrasound follow-up. Circulation. 2001. 104:2007–2011.
11. Morice MC, Serruys PW, Sousa JE, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002. 346:1773–1780.
12. Morino Y, Honda Y, Okura H, et al. An optimal diagnostic threshold for minimal stent area to predict target lesion revascularization following stent implantation in native coronary lesions. Am J Cardiol. 2001. 88:301–303.
13. Sonoda S, Morino Y, Ako J, et al. Impact of final stent dimensions on long-term results following sirolimus-eluting stent implantation. J Am Coll Cardiol. 2004. 43:1959–1963.
14. Fitzgerald PJ, Oshima A, Hayase M, et al. Final results of the Can Routine Ultrasound Influence Stent Expansion (CRUISE) study. Circulation. 2000. 102:523–530.
15. Moussa I, Moses J, di Mario C, et al. Does the specific intravascular ultrasound criterion used to optimize stent expansion have an impact on the probability of stent restenosis? Am J Cardiol. 1999. 83:1012–1017.
16. Kim KY, Hur SH, Cho YW. Optimal stent expansion by nominal pressure balloon inflation: an intravascular ultrasound study. Korean Circ J. 2002. 32:666–673.
17. Moses JW, Leon MB, Popma JJ, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003. 349:1315–1323.
18. Takebayashi H, Kobayashi Y, Mintz GS, et al. Intravascular ultrasound assessment of lesions with targer vessel faiure after sirolimus-eluting stent implantation. Am J Cardiol. 2005. 95:498–502.
19. Ong AT, McFadden EP, Regar E, de Jaegere PP, van Domburg RT, Serruys PW. Late angiographic stent thrombosis (LAST) events with drug-eluting stents. J Am Coll Cardiol. 2005. 45:2088–2092.
20. Kuchulakanti PK, Chu WW, Torguson R, et al. Correlates and long-term outcomes of angiographically proven stent thrombosis with sirolimus- and paclitaxel-eluting stents. Circulation. 2006. 113:1108–1113.
21. Park DW, Park SW. Stent thrombosis in the era of the drug-eluting stent. Korean Circ J. 2005. 35:791–794.
22. Fujii K, Carlier SG, Mintz GS, et al. Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: an intravascular ultrasound study. J Am Coll Cardiol. 2005. 45:995–998.
23. Park SH, Hong GR, Seo HS, Tahk SJ. Stent thrombosis after successful drug-eluting stent implantation. Korean Circ J. 2005. 35:163–171.
24. Schunkert H, Harrell L, Palacios IF. Implications of small reference vessel diameter in patients undergoing percutaneous coronary revascularization. J Am Coll Cardiol. 1999. 34:40–48.
25. Popma JJ, Leon MB, Moses JW, et al. Quantitative assessment of angiographic restenosis after sirolimus-eluting stent implantation in native coronary arteries. Circulation. 2004. 110:3773–3780.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download