Abstract
Background and Objectives
Heart failure is a progressive chronic disease with high morbidity and mortality. The aim of this study was to determine whether the N-terminal pro B-type natriuretic peptide (NT-proBNP) levels in the blood can predict readmission due to heart failure or cardiac death (cardiac event) following hospital discharge, and if these are a better predictive marker than a pre-discharge echocardiogram or other laboratory parameters in discharged patients with idiopathic dilated cardiomyopathy (DCM).
Subjects and Methods
The outcomes of 36 patients with idiopathic DCM, diagnosed on hospital admission, were retrospectively evaluated.
Results
During a mean follow-up period of 520 days, a 22.2% rate of cardiac events was observed. Evaluation of the NT-proBNPs showed the mid-term (mean 84th day after discharge) outpatient (OPD) NT-proBNP levels to be a strong predictor of cardiac events, with an area under the curve analysis of 0.90. The optimal mid-term OPD NT-proBNP cut-off level for predicting cardiac events was 1500 pg/mL, with a sensitivity and specificity of 80 and 92%, respectively; patients with levels above this threshold had a 22.9 hazard ratio for cardiac events compared to those with levels below this threshold.
Conclusion
The mid-term OPD plasma NT-proBNP levels were able to predict cardiac events in discharged patients with idiopathic DCM, regardless of the admission or pre-discharge NT-proBNP levels and other laboratory parameters. The measurement of OPD NT-proBNP at the mid term follow-up may be useful in outpatient therapeutic monitoring or for the development of prognostic guidelines in patients with idiopathic DCM.
Heart failure(HF) is a progressive chronic disease with high morbidity and mortality. Despite great advances in the medical management and survival following cardiac transplantation, the prognosis remains poor. HF is the single most frequent cause of hospitalization in the over 65 age group.1) The readmission rate for patients with HF within three to six months after hospital discharge has been reported to range from 17 to 55%, depending on the age and HF stage.2)3)
Clinical trials and registries have shown that the etiology of heart failure in 29-46% of cases is non-ischemic in origin; a majority of these cases have dilated cardiomyopathy(DCM), characterized by a progressive course of ventricular dilatation and systolic dysfunction.4)5)
Brain natriuretic peptide(BNP), a peptide hormone released primarily from the cardiac ventricles in response to myocyte stretch, is synthesized as an inactive prohormone that is split into an active hormone BNP(32 amino acids) and an inactive amino-terminal fragment, NT-proBNP(76 amino acids). BNP has been shown to induce vasodilation, diuresis and natriuresis, and inhibits the sympathetic nervous and renin-angiotensin-aldosterone systems.6)7)
The prognostic importance of BNP and NT-proBNP has been extensively studied in patients with heart failure, as well as those with acute coronary syndromes; they have been shown to be strong predictors of morbidity or mortality and in both.8-11)
Moreover, the pre-discharge BNP levels have been reported to be strong independent predictors of early readmission or death due to HF, and are more useful than clinical or echocardiographic parameters during acute care.12)
The aim of this study was to determine whether the N-terminal pro B-type natriuretic peptide(NT-proBNP) levels in the blood can predict hospital readmission due to heart failure or cardiac death after discharge, defined as cardiac events, and if these are better pre-dictive markers than a pre-discharge echocardiogram or other laboratory parameters in patients discharged with idiopathic dilated cardiomyopathy(DCM).
The outcomes of 36 patients with idiopathic DCM, diagnosed on admission to the Samsung Medical Center, between January 2003 and February 2006, were retrospectively evaluated. DCM was defined as cardiac enlargement and impaired systolic function of one or both ventricles, as based on echocardiography. In addition, idiopathic DCM was defined as DCM without identifiable etiology, such as ischemia, alcohol and Adriamycin. Ischemic DCM based on coronary angiography was excluded, as were alcoholic and adriamycin-induced DCM based on medical history.
Laboratory measurements, such as hemoglobin, sodium and creatinine, as well as echocardiographic examinations, were performed on admission, before discharge and at regular intervals during the follow-up period. The levels of NT-proBNP were measured at the time of admission, before discharge, and three to six months after discharge, and again at one year after discharge using an Elecsys proBNP reagent kit(Roche Diagnostic, Germany) on an Elecsys 2010 analyzer, before May 2004, or on a MODULAR ANALYTICS E170 (Roche Diagnostic, Germany) thereafter. The normal ranges for male and females <50 years of age were 0-88 and 0-153 pg/mL for males and females and 0-194 and 0-222 pg/mL for individuals older than 50, respectively.
All patients received the standard treatment with digoxin, diuretics(furosemide with or without spironolactone), angiotensin converting enzyme inhibitors or angiotensin II receptor blockers, as well as β-blockers. The mean follow-up period was 520±373 days; NT-proBNP was measured at mid-term(mean 84th day after discharge), at six to 12 months or after one year. The main study end-points were readmission due to heart failure or cardiac death. The causes of readmission or death were identified by medical record or a review of the death certificate.
The data were analyzed using SPSS 11.5 for Windows(SPSS Inc, Chicago, Illinois, USA). The baseline characteristics were compared between the cardiac event and event-free groups using Pearson's chi-squared and Mann-Whitney U tests where appropriate. Categorical variables are expressed as numbers(percentage), and continuous variables as the mean±SD. The percentage change in the NT-proBNP levels was defined as ["to"-"from"]×100/"from" NT-proBNP, and presented as a continuous variable. A multivariable Cox proportional hazard regression model was used to evaluate associations of the clinical variables, NT-proBNP levels and echocardiographic parameters with the incidence of cardiac events, with the findings expressed as a hazard ratio(HR) with a 95% confidence interval(CI). A receiver operating characteristics(ROC) curve was calculated to determine the cut-off value for NT-proBNP for predicting cardiac events. The cut-off value with optimal sensitivity and specificity, together with the area under the curve(AUC), were also identified. Survival curves were estimated according to the Kaplan-Meier method, and compared using a log-rank test. P<0.05 were considered significant.
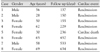
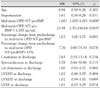
The baseline characteristics of the study patients according to cardiac events are summarized in Table 1. During the follow-up period of 520±373 days, cardiac events occurred in 8 patients(22.2%). The mean duration to a cardiac event from the time of discharge was 315±195 days. Readmission occurred in seven cases and cardiac death in a further one(Table 2). Among the variables, the mid-term(mean 84th day after discharge) outpatient(OPD) NT-proBNP level, percentage change from predischarge to mid-term OPD NT-proBNP and serum creatinine levels were significantly increased in the cardiac event group. Fig. 1 shows the ROC curve for the mid-term OPD NT-proBNP cut-off values and their association with cardiac events during follow-up. The mid-term OPD NT-proBNP level was a strong predictor of cardiac events, with an AUC of 0.90. The optimal mid-term OPD NT-proBNP cut-off level for predicting cardiac events during a mean follow-up period of 520 days was 1500 pg/mL, with a sensitivity and specificity of 80 and 92%, respectively.
In the univariate Cox regression analysis used to identify predictors of cardiac events after discharge(Table 3), neither the serum marker nor echocardiographic parameter at discharge was able to predict cardiac events. Among the NT-proBNPs, only the mid-term OPD NT-proBNP level was associated with cardiac events; the hazard ratio was above 23 when the cut-off value of the mid-term OPD NT-proBNP was 1,500 pg/mL.
From the multivariate Cox regression model, performed by the enter method, with all variables in the univariate analysis, the only independent predictor of cardiac events was a mid-term OPD NT-proBNP level ≥1,500 pg/mL(HR=22.9, 95% CI=2.46-221.10)(Table 4).
The event free survival rate was significantly higher in patients with a lower mid-term OPD NT-proBNP(<1,500 pg/mL) than in those with a higher mid-term OPD NT-proBNP level(≥1,500 pg/mL)(Fig. 2, Kaplan-Meier methods, p=0.0001 from the log-rank test).
The main finding of this study was that mid-term OPD plasma NT-proBNP levels at three months following hospital discharge were able to predict cardiac events, such as readmission due to heart failure or cardiac death, in patients diagnosed with idiopathic DCM on hospital admission. During the mean follow-up period of 520 days, eight cardiac events were observed; the mid-term(mean 84th day after discharge) OPD plasma NT-proBNP level was a strong independent predictor of cardiac events. The optimal cut-off value for the mid-term OPD NT-proBNP levels was 1,500 pg/mL, with a hazard ratio for cardiac events of 22.9.
Many clinical and echocardiographic parameters associated with adverse outcomes in patients with heart failure have been identified, including physical examination(elevated jugular venous pressure, a third heart sound),13) laboratory findings(anemia, higher serum creatinine, lower cholesterol)14-16) and echocardiographic parameters(lower ejection fraction, increased LVEDD).17)18)
The prognostic importance of the BNP and NT-proBNP levels has been extensively studied in patients with heart failure, as well as those with acute coronary syndromes. Both markers have been shown to be strong predictors of morbidity and mortality.8-11) NT-proBNP has been reported to be a better marker than BNP for the detection and evaluation of chronic heart failure; this is because it is more stable and a better predictor of cardiac dysfunction.19)20) NT-proBNP has consistently been associated with increased risk for all-causes of mortality or hospitalization for heart failure in patients with severe congestive heart failure.21) A single measurement of the NT-proBNP level in patients with advanced CHF can help identify those at highest risk of death, and is also a better prognostic marker than the left ventricular ejection fraction.22) NT-proBNP is also known to be a strong predictor of the one-year mortality in hospitalized heart failure patients with both preserved and reduced systolic functions.23) Variations in the NT-proBNP levels have been noted to be related to cardiac events within six months of hospital discharge; NT-proBNP levels are also potentially useful in the evaluation of treatment efficacy as well as in planning the hospital discharge of patients with HF.24)
Many previous studies on the prediction of cardiac events enrolled patients with heart failure who had heterogeneous etiologies, including ischemic and non-ischemic heart disease; however, our study had a homogenous population with idiopathic DCM. In addition, our study differed from prior studies in the following ways:
First, about a quarter of the patients with recent-onset DCM improved spontaneously; survival was better among the patients with idiopathic DCM than those with ischemic cardiomyopathy.25)26) In previous studies, including ischemic and non-ischemic heart disease, depending on the age and HF stage, it has been reported that 17-55% of patients required readmission within three to six months after discharge;2)3) however, in this study, 10.8% of patients were readmitted within six months following hospital discharge. The results showed that the mid-term OPD plasma NT-proBNP levels may be useful for predicting hospital readmission or cardiac death six months after hospital discharge in idiopathic DCM patients. Therefore, more intensive medical therapy in DCM patients with mid-term OPD NT-proBNP levels greater than 1500 pg/mL, as based on serial measurements of the NT-proBNP levels, may improve patient outcomes.27)28) Second, while other studies have shown that the NT-proBNP levels on admission or pre-discharge, and variations between admission and discharge were related to readmission or death within six months following discharge,12)24) this study showed that neither variation during admission nor the pre-discharge NT-proBNP level were independent predictors of cardiac events. Third, according to several studies, the echocardiographic parameters may play an important role in predicting cardiac mortality in patients with DCM and congestive heart failure. In particular, the restrictive filling pattern, as characterized by a high peakearly diastolz mitral inflow velocity(E), a low peaklate diastolz mitral inflow velocity(A) wave, a high E/A ratio and a shortened E wave deceleration time, has been shown to be powerful predictor of increased mortality in patients with congestive heart failure and DCM;29)30) however, in this study, the echocardiographic parameters were unable to predict cardiac events.
The limitations of this study include the followings: 1) the study population was relatively small, 2) echocardiography and NT proBNP sampling was not performed on the same day; however, the time differences between the pre-discharge measurements were less than one week. Finally, our study was a single-center retrospective study; multicenter prospective studies will be needed to support our results.
In conclusion, the mid-term OPD plasma NT-proBNP levels following hospital discharge were able to predict cardiac events in patients diagnosed with idiopathic DCM on hospital admission, regardless of the admission or pre-discharge NT-proBNP levels and other laboratory and echocardiographic parameters. The optimal cut-off NT-proBNP level was found to be 1,500 pg/mL. Therefore, measurement of the mid-term OPD NT-proBNP level may be useful for outpatient therapeutic monitoring or in the development of prognostic guidelines in patients with idiopathic DCM.
Figures and Tables
Fig. 1
Receiver operating characteristic curve for the mid-term OPD N-terminal pro-B-type natriuretic peptide cut-off values and their association with cardiac events during follow-up. OPD: outpatient department.

Fig. 2
Kaplan-Meier curves according to the predefined mid-term OPD N-terminal pro-B-type natriuretic peptide cut-off (1,500 pg/mL) level. OPD: outpatient department.
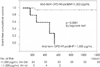
Table 1
Baseline characteristics of patients with idiopathic dilated cardiomyopathy according to cardiac events

NYHA: New York Heart Association, OPD: outpatient deporfmont, NT-proBNP: N-terminal pro-B-type natriuretic peptide, LA: left atrium, LVESD: left ventricular end-systolic dimension, LVEDD: left ventricular end-diastolic dimension, LVEF: left ventricular ejection fraction, ACEI: angiotensin converting enzyme inhibitor, ARB: angiotensin II receptor blocker. *: p<0.05 Cardiac event (-) vs. Cardiac event (+)
References
1. Braunwald E. Shattuck lecture: cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med. 1997. 337:1360–1369.
2. Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995. 333:1190–1195.
3. McDermott MM, Feinglass J, Lee PI, et al. Systolic function, readmission rates, and survival among consecutively hospitalized patients with congestive heart failure. Am Heart J. 1997. 134:728–736.
4. McMurray JJ, Stewart S. Epidemiology, aetiology, and prognosis of heart failure. Heart. 2000. 83:596–602.
5. Han SW, Ryu KH, Chae SC, et al. Multicenter analysis of clinical characteristics and prognostic factors of patients with congestive heart failure in Korea. Korean Circ J. 2005. 35:357–361.
6. Levin ER, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med. 1998. 339:321–328.
7. Hall C. Essential biochemistry and physiology of (NT-pro) BNP. Eur J Heart Fail. 2004. 6:257–260.
8. Tsutamoto T, Wada A, Maeda K, et al. Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation. 1997. 96:509–516.
9. Omland T, Persson A, Ng L, et al. N-terminal pro-B-type natriuretic peptide and long-term mortality in acute coronary syndromes. Circulation. 2002. 106:2913–2918.
10. Baek KK, Jeon ES, Rhee I, et al. N-terminal pro-B-type natriuretic peptide as a prognostic marker in acute coronary syndrome. Korean Circ J. 2004. 34:1070–1081.
11. Chung IH, Yoo BS, Ryu HY, et al. The relationship between the early follow-up BNP level and congestive status or prognosis in acute heart failure. Korean Circ J. 2006. 36:200–207.
12. Logeart D, Thabut G, Jourdain P, et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol. 2004. 43:635–641.
13. Drazner MH, Rame JE, Stevenson LW, Dries DL. Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med. 2001. 345:574–581.
14. Rauchhaus M, Clark AL, Doehner W, et al. The relationship between cholesterol and survival in patients with chronic heart failure. J Am Coll Cardiol. 2003. 42:1933–1940.
15. Forman DE, Butler J, Wang Y, et al. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004. 43:61–67.
16. Anand I, McMurray JJ, Whitmore J, et al. Anemia and its relationship to clinical outcome in heart failure. Circulation. 2004. 110:149–154.
17. Solomon SD, Anavekar N, Skali H, et al. Influence of ejection fraction on cardiovascular outcomes in a broad spectrum of heart failure patients. Circulation. 2005. 112:3738–3744.
18. Grayburn PA, Appleton CP, DeMaria AN, et al. Echocardiographic predictors of morbidity and mortality in patients with advanced heart failure. J Am Coll Cardiol. 2005. 45:1064–1071.
19. Yeo KT, Wu AH, Apple FS, et al. Multicenter evaluation of the Roche NT-proBNP assay and comparison to the Biosite Triage BNP assay. Clin Chim Acta. 2003. 338:107–115.
20. Seino Y, Ogawa A, Yamashita T, et al. Application of NT-proBNP and BNP measurements in cardiac care: a more discerning marker for the detection and evaluation of heart failure. Eur J Heart Fail. 2004. 6:295–300.
21. Hartmann F, Packer M, Coats AJ, et al. Prognostic impact of plasma N-terminal pro-brain natriuretic peptide in severe chronic congestive heart failure. Circulation. 2004. 110:1780–1786.
22. Gardner RS, Ozalp F, Murday AJ, Robb SD, McDonagh TA. N-terminal pro-brain natriuretic peptide: a new gold standard in predicting mortality in patients with advanced heart failure. Eur Heart J. 2003. 24:1735–1743.
23. Kirk V, Bay M, Parner J, et al. N-terminal proBNP and mortality in hospitalised patients with heart failure and preserved vs. reduced systolic function. Eur J Heart Fail. 2004. 6:335–341.
24. Bettencourt P, Azevedo A, Pimenta J, Frioes F, Ferreira S, Ferreira A. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation. 2004. 110:2168–2174.
25. Felker GM, Thompson RE, Hare JM, et al. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N Engl J Med. 2000. 342:1077–1084.
26. Wynne J, Braunwald E. Zipes DP, Libby P, Bonow RO, Braunwald E, editors. The cardiomyopathies. Braunwald's Heart Disease: a textbook of cardiovascular medicine. 2005. 7th ed. Philadelphia: Elsevier Saunders Company;1659–1696.
27. Troughton RW, Frampton CM, Yandle TG, Espiner EA, Nicholls MG, Richards AM. Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (N-BNP) concentrations. Lancet. 2000. 355:1126–1130.
28. Richards M, Troughton RW. NT-proBNP in heart failure: therapy decisions and monitoring. Eur J Heart Fail. 2004. 6:351–354.
29. Werner GS, Schaefer C, Dirks R, Figulla HR, Kreuzer H. Prognostic value of Doppler echocardiographic assessment of left ventricular filling in idiopathic dilated cardiomyopathy. Am J Cardiol. 1994. 73:792–798.
30. Pinamonti B, Zecchin M, di Lenarda A, Gregori D, Sinagra G, Camerini F. Persistence of restrictive left ventricular filling pattern in dilated cardiomyopathy: an ominous prognostic sign. J Am Coll Cardiol. 1997. 29:604–612.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download