Abstract
Despite the excellent success of lowering low-density lipoprotein cholesterol (LDLc) cholesterol for treating coronary heart disease (CHD), a major part of the population still suffer from CHD. This fact is more prominent among the high risk patients who receive lipid lowering treatment with statins. This treatment is based on the prevailing view that LDL cholesterol (LDLc) is the only important risk factor for CHD. It is well known that HDL plays a crucial role for preventing CHD. Several epidemiologic studies and clinical trials have reported that high density lipoprotein cholesterol (HDLc) is an independent risk factor for CHD as well. A large scale meta-analysis of clinical trials clearly supports that increasing HDLc is equally important as decreasing LDLc, suggesting that physicians should pay attention to increasing HDLc as well as decreasing LDLc. Ongoing trials that are focused on this issue will test this hypothesis in the near future.
It is well known that a high cholesterol level is a major risk factor for coronary heart disease(CHD). Several epidemiologic studies such as the Multiple Risk Factor Intervention Trial(MR-FIT) showed that the plasma total cholesterol concentration is positively associated with the risk of cardiovascular mortality.1) Seven Countries Study has revealed that a high plasma cholesterol concentration was the universal risk factor for CHD, regardless of geography and race.2) It is also known that a high LDLc concentration in Koreans is significantly associated with an increased CHD risk.3) Many clinical trials have supported that lowering cholesterol is a crucially important therapeutic tool for preventing cardiovascular mortality and morbidity.
As a result of these studies, lowering cholesterol, and especially the low-density lipoprotein cholesterol(LDLc), is now widely accepted as an important tool for preventing CHD. Moreover, recent clinical trials such as the TNT and PROVE-IT trials have suggested that intensive LDLc lowering is better than conventional treatment.4)5) Nowadays, the paradigm of "the lower, the better" for high risk patients has become a mantra.
However, it was also known that intensive LDLc lowering is not a panacea for preventing CHD. A large scale meta analysis revealed that lowering cholesterol prevented CHD events by 26%, implicating that 74% of events were not avoided with lowering cholesterol.6-8) Consequently, the non LDLc such as HDLc and triglyceride have been revealed as another important risk factor, which runs counter to the previously accepted dogma.
In this article, the epidemiologic studies and clinical trials will be reviewed to show the importance of LDLc as an independent risk factor for CHD. Further, it will be discussed the light of the LDLc centric paradigm. Finally, several studies will be sited to support that HDLc is the another important risk factor for CHD and increasing the HDLc is as important a therapeutic tool as decreasing the LDLc.
A myriad of clinical trials have consistently showed that lowering LDLc reduces CHD mortality and morbidity. The Scandinavian Simvastatin Survival Study (4S) was the first to report that lowering LDLc in CHD patients who have a high plasma LDLc level reduced the recurrence of CHD and death.9) The West on Scotland Coronary Artery Disease Prevention Study (WOSCOPS) found that lowering LDLc in healthy men who have a high LDLc level was even helpful for preventing CHD in those people.10) The Cholesterol And Recurrent Event (CARE) and Long-term Intervention with Pravastatin in Ischaemic Disease (LIPID) studies revealed that for CHD patients with a moderate cholesterol level, treatment to lower lipid was also helpful for preventing recurrence of CHD.11)12) The Heart Protection Study(HPS) systematically showed that the benefit of lipid lowering treatment is the same regardless of the baseline LDLc level, suggesting that lipid loweriry treatment should be started for the entire range of LDLc levels, only if the patients have a substantial risk for CHD.13) HPS also confirmed that the benefit of lipid lowering treatment in women was the same as that of men. The Prospective Study of Pravastatin in the Elderly at Risk(PROSPER) study, which was performed on very old aged men and women, eloquently revealed that the benefit of lipid lowering treatment for the elderly was the same as it was for the middle aged.14) It also showed that the side effects of the lipid lowering agents, i.e., the statins, in the elderly were not so serious compared to those of the middle aged, which virtually unlocked the final barrier blocking the use of statin.
Two recent clinical trials, the Treating to New Targets (TNT) and Pravastatin or Atorvastatin Evaluation and Infection Therapy (PROVE-IT) studies, went further.4)5) These studies elegantly showed that intensive lipid lowering treatment is far better than conventional treatment for preventing cardiovascular mortality in high risk patients, thus igniting another frenzy of statin use, with everyone shouting "the lower, the better"!
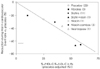
The Cholesterol Treatment Trial(CTT) study was recently published and it showed the linear relationship between cardiovascular risk reduction and the degree of lowering the LDLc level(Fig. 1), again confirming the mantra is valid indeed! "The lower the better!".15)
Not surprisingly, physicians around world have enthusiastically espoused lipid lowering treatment, and so lowering the LDLc in the patients with a substantial risk for CHD has become all the fashion.
In our zeal to lower lipid, our efforts to eradicate the development of CHD around the globe have not always been successful. A recent meta-analysis of 97 randomised controlled trials investigated different lipid lowering interventions in a total of almost 280,000 individuals. The results showed that only 26% of CHD could be avoided with treatment, leaving another 74% of the patients for whom CHD couldn't be avoided and they didn't benefit from treatment.6)7) There have been significant research findings for several decades that have poked large holes in the cholesterol dogma. Genest et al. reported that with using only the LDLc concentration, they could not completely discern between the CHD patients and the normal population. In their study, the LDLc distribution of both groups overlapped by 70%.16) Furthermore, the proportion of subjects with the highest occurrence of the LDLc concentration was similar in both groups(130 mg/dL of LDLc)(Fig. 2). The recently reported world-wide cross sectional study INTERHEART lends support for feeling righteously skeptical about the LDLc centric view. In this study, it was not the LDLc concentration, but the apoB/apoA1 ratio that was the foremost risk factor for CHD, followed by smoking and psychosocial stress.17)
These collective findings have given us a reason to be suspicious and surely reevaluate the cholesterol dogma.
Cholesterol is synthesized by all the organs in the human body, yet breaking down the cholesterol is performed in only one organ: the liver. Transporting cholesterol from the peripheral organs towards the liver requires a specific pathway designed to transfer cholesterol, that is, the HDL. By and large, one can surmise that a higher HDLc level would be better than a lower HDLc level.
According to the Framingham Heart study, men and women with higher HDLc levels suffered less CHD mortality and morbidity than those men and women with lower HDLc levels, and this was regardless of age and sex.18) The impact of the HDLc concentration on CHD has an interaction with the LDLc concentration. It is known that the population with the highest HDLc and lowest LDLc concentrations has the lowest risk for CHD mortality, whereas those people with the lowest HDLc and highest LDLc concentrations had the highest risk for this disease.
The impact of HDLc is universal, regardless of race. In the elaborately designed study performed on 95 Korean CHD patients and 216 healthy Koreans, Cho et al.19) showed that the patients with CHD had significantly lower HDLc concentrations than normal healthy people. In a large scale clinical study that performed carotid ultrasonography in 4,077 healthy Koreans over 27 months of a follow-up period, Cho et al.20) revealed that a low HDLc concentration was an independent risk factor for atherosclerotic stenosis of the carotid artery. In parallel, Bae et al.21) reported that a low HDLc concentration was significantly associated with increased carotid intima-media thickness, which is the important surrogate marker for CHD.
In addition to reverse cholesterol transport(RCT), HDL has several functions such as anti-inflammation, anti-oxidation, anti-thrombosis, anti-infection and vasodilatation. Yet in this article, only the HDL's RCT function will be discussed.
As previously mentioned, the liver is the only organ that can break down cholesterol. Three different states/types of HDL are needed for this purpose: lipid-poor apoA-1, nascent HDL and alpha-HDL.
The first step of RCT is cholesterol efflux. Lipid-poor apoA-1 plays the role as an acceptor for cholesterol. With cholesterol efflux, the proteins are lipidated, converting them to nascent HDL, and these are the substrate of lecithin: cholesterol acyltransferase(LCAT). Esterification of cholesterol in the nascent HDL leads to formation of spherical alpha-HDL particles. These particles convert themselves to larger alpha-HDL particles by acquiring more cholesterol from many different sources. The second step of RCT is that cholesteryl ester transfer protein (CETP) exchanges the accumulated cholesterol ester of HDL for the triglyceride of VLDL. The last step is accomplished by the uptake of HDL in the liver via the SR-B1 receptor. As a final result, cholesterol from the peripheral organs is transferred to the liver via HDL.22)
There is considerable epidemiologic evidence that the LDLc and HDLc levels are comparably important as predictors of the risk of CHD.23) The Framingham Offspring study showed that a 1% difference in HDLc, for both sexes, or a 1% difference in the LDLc implies a 1% difference in the incidence of CHD.24) Indeed, the statin clinical trials clearly demonstrated that a 1% reduction in LDLc is associated with a 1% reduction in the CHD risk, and this is true over a wide range of LDLc concentration. 4)11) The insightful epidemiologic analysis by Gordon et al.25) found that a 1 mg/dL, or about 2-3%, greater HDLc level, is associated with an LDLc-independent 2-4% risk reduction for cardiovascular disease over a 7 to 10-year follow-up duration, and these findings were valid for 4 studies on 4 different populations. In an comprehensive and timely review article, Brown et al.26) dreamed up a plausible hypothesis after performing a meta-analysis on 23 clinical trials: both HDLc and LDLc are equally associated with a reduced risk of CHD. The hypothesis can be described in the formula:
Relative risk=(1+%ΔLDLc)×(1+%ΔHDLc),
where the '%' is given as a decimal value(i.e., 30% is 0.3) and an increase in the lipoprotein level is '+' and a decrease is '-'. For moderate changes in these lipoproteins (30-40%), the final term of this product(%ΔLDLc×%ΔHDLc) is so small(i.e., 0.3×0.3=0.09) as to be negligible and it can be omitted. Consequently, the formula can be described as:
Relative risk=1+%ΔLDLc-%ΔHDLc
The relative risk will be a positive number, ranging between 1(no benefit) or 0(complete benefit). For example, if one can decrease the LDLc by 40% and increase HDLc by 30%, then the relative risk will be 0.3(1-0.4-0.3), implicating that the relative risk reduction will be 70% in comparison with placebo(Fig. 3). The R square of this formula is reported to be about 0.95, meaning that nearly the complete CHD risk can be explained with only the variation of these lipoproteins. The final proof of this hypothesis awaits the completion of three ongoing clinical trials. In these trials, aggressive statin therapy is compared to the combination of statin therapy and an HDLc increasing agent such as niacin or fibrate.
A plethora of clinical trials have confirmed that intensive lipid lowering treatment results in a lower rate of CHD events than does moderate lipid lowering treatment, and the greatest benefits are related to the greatest reductions of the LDLc levels. But even with intensive lipid lowering, it is also known that only a quarter of the events can be avoided. It has been suggested that CHD patients additively benefit from increasing the HDLc as well as decreasing the LDLc. Several studies have firmly supported this hypothesis, and this hypothesis now awaits its final validation in the near future.
Figures and Tables
Fig. 1
Relation between the proportional reduction in the incidence of major coronary events and mean absolute low-density lipoprotein (LDL) cholesterol reduction at 1 year.15)

Fig. 2
LDL cholesterol distribution between coronary heart disease (CHD) patients and normal controls.16) LDLc: low-density lipoprotein cholesterol.

Fig. 3
Effect of various drug classes on trial primary clinical event rate.26) HDL: high-density lipoprotein, LDL: low-density lipoprotein.
References
1. Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded?: findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 1986. 256:2823–2828.
2. Keys A, Menotti A, Aravanis C, et al. The seven countries study: 2,289 deaths in 15 years. Prev Med. 1984. 13:141–154.
3. Hong SJ, Oh DJ, Kim EJ, et al. The comparison of seru lipid levels and risk factors according to the status of coronary atherosclerosis in Koreans. Korean Circ J. 2003. 33:465–474.
4. LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005. 352:1425–1435.
5. Cannon CP, Murphy SA, Braunwald E. Intensive lipid lowering with atorvastatin in coronary disease. N Engl J Med. 2005. 353:93–96.
6. Studer M, Briel M, Leimenstoll B, Glass TR, Bucher HC. Effect of different antilipidemic agents and diets on mortality: a systematic review. Arch Intern Med. 2005. 165:725–730.
7. Briel M, Studer M, Glass TR, Bucher HC. Effects of statins on stroke prevention in patients with and without coronary heart disease: a meta-analysis of randomized controlled trials. Am J Med. 2004. 117:596–606.
8. Bays HE. Extended-release niacin/lovastatin: the first combination product for dyslipidemia. Expert Rev Cardiovasc Ther. 2004. 2:485–501.
9. Scandinavian Simvastatin Survival Study (4S) Group. Randomised trial of cholesterol lowering in 4,444 patients with coronary heart disease. Lancet. 1994. 344:1383–1389.
10. West of Scotland Coronary Prevention Study Group. Influence of pravastatin and plasma lipids on clinical events in the West of Scotland Coronary Prevention Study (WOSCOPS). Circulation. 1998. 97:1440–1445.
11. Goldberg RB, Mellies MJ, Sacks FM, et al. Cardiovascular events and their reduction with pravastatin in diabetic and glucose-intolerant myocardial infarction survivors with average cholesterol levels: subgroup analyses in the cholesterol and recurrent events (CARE ) trial. Circulation. 1998. 98:2513–2519.
12. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998. 339:1349–1357.
13. Heart Protection Study Collaborators. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002. 360:7–22.
14. Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER ): a randomised controlled trial. Lancet. 2002. 360:1623–1630.
15. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005. 366:1267–1278.
16. Genest J Jr, McNamara JR, Ordovas JM, et al. Lipoprotein cholesterol, apolipoprotein A-I and B and lipoprotein (a) abnormalities in men with premature coronary artery disease. J Am Coll Cardiol. 1992. 19:792–802.
17. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (THE INTERHEART STUDY): case-control study. Lancet. 2004. 364:937–952.
18. Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. Am J Med. 1977. 62:707–714.
19. Cho EY, Bae SJ, Cho HK, et al. Association of cholesteryl ester transfer protein gene polymorphism with serum lipid concentration and coronary artery disease in Korean men. Korean Circ J. 2004. 34:565–573.
20. Cho DK, Kwon SU, Kim SW, et al. Risk factors and predictors for the progression of carotid atherosclerotic stenosis in Korean Adults. Korean Circ J. 2005. 35:834–840.
21. Bae JH, Seun KB, Jung HO, et al. Analysis of Korean carotid intima-media thickness in Korean healthy subjects and patients with risk factors: Korean Multi-Center Epidemiologic Study. Korean Circ J. 2005. 35:513–524.
22. Brewer HB Jr. High-density lipoproteins: a new potential therapeutic target for the prevention of cardiovascular disease. Arterioscler Thromb Vasc Biol. 2004. 24:387–391.
23. Assmann G, Cullen P, Schulte H. The Munster Heart Study (PROCAM ): results of follow-up at 8 years. Eur Heart J. 1998. 19:Suppl A. A2–A11.
24. Wilson PW, Anderson KM, Castelli WP. Twelve-year incidence of coronary heart disease in middle-aged adults during the era of hypertensive therapy. Am J Med. 1991. 90:11–16.
25. Gordon DJ, Probstfield JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease: four prospective American studies. Circulation. 1989. 79:8–15.
26. Brown BG, Stukovsky KH, Zhao XQ. Simultaneous low-density lipoprotein-C lowering and high-density lipoprotein-C elevation for optimum cardiovascular disease prevention with various drug classes, and their combinations: a meta-analysis of 23 randomized lipid trials. Curr Opin Lipidol. 2006. 17:631–636.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download