Abstract
Background and Objectives
Whether uric acid is a predictor of cardiovascular events remains controversial. We sought to evaluate the effects of the serum uric acid levels on major adverse cardiovascular events (MACEs) in the patients with coronary artery disease (CAD).
Subjects and Methods
The study population consisted of 660 consecutive patients with CAD, and they were followed up for a mean of 27 months (maximum: 62 months). The recorded MACEs included acute myocardial infarction (AMI), stroke, coronary artery bypass graft, percutaneous coronary intervention (PCI) due to de novo lesion during follow up, congestive heart failure (CHF) and sudden cardiac death.
Results
In the CAD patients with a uric acid level ≤3.88 mg/dL (the lowest quartile), as compared with those CAD patients with uric acid levels >5.74 mg/dL (the highest quartile), the MACE rate increased from 7.2% to 20.1%. On univariate Cox regression analysis, the highest uric acid quartile was a predictor of AMI, CHF and MACE. The absolute serum uric acid level was predictive of PCI, CHF and MACE. Multivariate Cox regression analysis showed that the independent predictors of MACE were presentation with acute coronary syndrome (HR 1.70, 95% CI: 1.04 to 2.78, p=0.033), multi-vessel disease (HR 2.43, 95% CI: 1.44 to 4.12, p=0.001), and the uric acid levels (HR 1.22, 95% CI: 1.05 to 1.43, p=0.010), and the highest uric acid quartile (HR 2.54, 95% CI: 1.58 to 4.10, p<0.001).
Elevated serum uric acid is an end product of purine metabolism, and this reflects increased xanthine oxidase activity. Serum uric acid has been shown to be correlated with endothelial dysfunction, cardiovascular disease and insulin resistance.1-4) It has been recently reported that serum uric acid is an independent predictor of mortality for patients with coronary artery disease(CAD) and morbidity, including acute myocardial infarction(AMI) or congestive heart failure(CHF). A causal role of serum uric acid in the development of CAD has not postulated and it was not related to death from cardiovascular disease or death from all causes, according to the Framingham heart study.5-8) It remains unclear whether serum uric acid is associated with major adverse cardiovascular outcomes(MACE) as well as mortality in patients with CAD.
To test the hypothesis that the uric acid level could predict cardiac morbidity and morality, we performed this study to evaluate the predictive value of serum uric acid on the subsequent MACEs such as death, AMI, stroke, CHF, percutaneous coronary intervention(PCI) and coronary artery bypass graft(CABG) surgery in 660 consecutive patients with CAD.
All the patients who were undergoing coronary angiography at the Konyang University Hospital were prospectively enrolled in a registry that includes baseline demographics and the clinical and angiographic characteristics. These patients visited the hospital once or twice per two months or they were contacted 6 and 12 months after the procedure and yearly thereafter by trained research technicians.
Following approval by the hospital ethics committee, the data base was searched for all the patients who had at least 30% luminal stenosis according to coronary angiography and they had their laboratory data available, including the serum uric acid levels within 2 weeks of performing their procedures, and the procedures were done between June 2000 and June 2001 at Konyang University Hospital in Daejeon, Korea. These dates were chosen as our practice remained relatively stable with regards to the adjunctive medical therapies(in particular clopidogrel) and stent types(bare metal) if they underwent PCI. For patients who underwent two procedures during the study period, only the first procedure was included. Baseline data on the patients was available from the database, including their clinical characteristics and the medication used. Hypertension was defined as a blood pressure ≥140/90 mmHg or the use of antihypertensive medications. Diabetes was defined as a fasting glucose level of ≥126 mg/dL, a nonfasting glucose level of ≥200 mg/dL, a reported history of diabetes or the current use of diabetes medication. AMI was defined as increased myocardial enzyme concentrations with typical chest pain that persisted >30 minutes or electrocardiographic changes(including ischemic ST-segemnt depression, ST-segment elevation or pathologic Q waves). CHF was diagnosed by the Framingham criteria. Those patients who refused authorization for medical records research were excluded, and an informed consent was obtained from all enrolled patients.
Follow up was achieved mainly through the data base and a chart review(574, 87.0%) and telephone calls(86, 13.0%) at 6 months and yearly after the procedure. The measured outcomes were cardiac death, AMI(defined by an increase in the cardiac biomarkers), CHF(new symptoms of CHF or increased symptoms of CHF that required treatment), PCI or CABG of de novo lesion, and stroke.
Continuous variables are summarized as means±SDs. Discrete variables are presented as group percentages. Kaplan-Meier estimates were used to describe the survival rates. For the time-to-event analyses, follow-up began at the date of discharge. One-way analysis of variance, Pearson's chi-squared tests and log-rank tests were used to test the significance of group differences.
Cox regression analysis was used to estimate the hazard ratios for the serum uric acid levels and the other clinical variables. Patients in the the lowest quartile were designated as the reference group. Statistical significance was accepted as p less than 0.05.
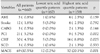
The study population consisted of 660 consecutive patients with angiographically proven CAD, and these patients had at least one serum uric acid measurement within 2 weeks of the procedure during the study period. The study population was divided into four groups according to the quartiles of the serum uric acid levels. The lowest quartile was a serum uric acid level ≤3.88 mg/dL(n=167, 25.3%), the second quartile was 3.88 mg/dL <serum uric acid ≤4.85 mg/dL(n=164, 24.8%), the third quartile was 4.85mg/dL <serum uric acid level ≤5.74 mg/dL(n=170, 25.8%), and the highest quartile was a serum uric acid level >5.74 mg/dL(n=159, 24.1%), respectively.
The median follow up was 27 months(range: -1 to 62 months).
Compared with the lowest quartile patients, the highest quartile patients had a higher proportion of male patients, a lower left ventricular ejection fraction, less smokers, lower levels of high-density and low-density lipoprotein cholesterol and a higher serum creatinine level. There were no significant differences in the mean age, body mass index, the diagnosis, the traditional atherosclerotic risk factors, treatment and the prescribed medications among each of the quartile groups.
At the end of the follow up period, there were 3 cardiac deaths, 5 AMIs, 3 CABGs, 21 PCIs, 30 CHFs and 12 strokes. In all, 69 patients experienced at least one MACE event(Table 2). There were 7 noncardiac deaths.
The MACE-free survival curves demonstrated a significant divergence of the highest uric acid quartile group from that of the third, second and the lowest quartiles (Fig. 1). The highest quartile group demonstrated a significant difference in AMI survival from that of the second and third quartile groups. The lowest quartile group required PCI least frequently. In terms of CHF, the quartile 4 showed a lower survival curve than did quartiles 1 and 2. However, there were no significant differences among each group in terms of cardiac death, stroke and CABG, including noncardiac death.
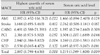
Univariate analysis revealed that MACE was associated with age, acute coronary syndrome(ACS) at presentation, multi-vessel disease, the uric acid level, the highest uric acid quartile and statin use(Table 3). The relevant baseline clinical and angiographic characteristics were included in a multivariable model. These characteristics included age, ACS, multi-vessel disease, the uric acid levels (or uric acid quartiles) and medications. Those variables showed a p of at least p<0.1 in Table 3. Patients on statin showed a higher incidence of MACE than those patients without statin, which was opposite to the already reported concept. We thought the reason for this was that the study subjects who were on statin had a higher incidence of ACS and multi-vessel disease(28.6% vs 17.5%, p=0.001, 39.3% vs 23.9%, p=0.000, respectively) than those subjects who were not on statin. However, the association between statin use and MACE did not show any significance after multivariate analysis.
On multivariable analysis, ACS(HR 1.7), multi-vessel disease(HR 2.9), the serum uric acid level(HR 1.2), and the highest uric acid quartile(HR 2.5) were all related to an increased risk of MACE(Table 4). The highest uric acid quartile was associated with an increased risk of AMI(HR 13.0) and CHF(HR 2.8), as well as any MACE(2.9). Serum uric acid was associated with an increased risk of PCI(HR 1.3) and CHF(HR 1.3), as well as any type of MACE(HR 1.2). A trend toward increased cardiac mortality(HR 1.7, p=0.081) was found(Table 5).
The main findings of this study are: i) Increased serum uric acid(highest quartile vs. lowest quartile) is associated with almost a 3-times increased MACE rate(7.2% vs. 20.1%, respectively). This is mainly due to CHF and not mortality; ii) the uric acid quartile is a predictor of AMI, CHF and MACE, and the absolute serum uric acid level is a predictor of PCI, CHF and MACE; iii) multivariate Cox regression analysis showed that the independent factors of MACE are ACS, multi-vessel disease, the uric acid levels and the highest uric acid quartile.
The important implication from our findings is that an increased serum uric acid level(>5.74 mg/dL) should be considered in the risk assessment for future MACEs in the patients with CAD. Such patients may require more aggressive secondary prevention measures.
Recent studies have suggested a role for serum uric acid as a predictor of mortality for patients with CAD, as well as an association between serum uric acid and other cardiovascular diseases.5)6)9)10) On the other hand, the Framingham heart study failed to disclose an association between serum uric acid and the development of CAD, death from cardiovascular disease or death from all causes.8) However, uric acid is known to be related to insulin resistance, endothelial dysfunction and the cardiovascular risk factors.2)3)9)11)12) Taken together, whether hyperuricemia is causally related to CAD has still not been clearly shown, although statistical adjustments suggest a strong independent correlation.5)6) Our study results did not show the role of uric acid as a predictor of mortality for patients with CAD, and this was unlike the previous studies.5)6) But it was similar to the Framingham heart study.8)
Serum uric acid and the uric acid quartiles were significantly correlated with CHF in our study, although they showed a significant, but weak association with the development of AMI or PCI, respectively. The increased serum uric acid level reflects increased xanthine oxidase activity that produces more oxygen free radicals.1)13) This increased oxidative stress may induce endothelial dysfunction of the small myocardial vessels, and then myocardial dysfunction.4) Oxidative stress-induced breakdown of nitric oxide can blunt the Frank-Starling response in the heart,14) and it may be a mechanism of decreased heart function via hyperuricemia. The predictive role of uric acid for the development of heart failure in patients with CAD was also evident in a recent study performed on patients with AMI.6)
Although there is still controversy about the association between serum uric acid and CAD,8)9)11) the present study demonstrates the highest uric acid quartile was associated with the development of AMI and the tendency for an increased need for PCI in the CAD patients in routine clinical practice, while serum uric acid was associated with the need for PCI and the tendency for an increased risk of cardiac death. These associations are related to the progression of the underlying CAD. Although the exact mechanisms of developing hyperuricemia and CAD are not fully understood and the value of therapies aimed at lowering uric acid levels is unproven, the associations of developing hyperuricemia and CAD with insulin resistance, endothelial dysfunction and increased oxidative stress are clear.2)3)9)11) The higher rates of AMI and the increased need for PCI, as related to serum uric acid in our study results, are exactly the same as that observed in hypertensive patients who had satisfactory control of their blood pressure.10)
There were a small number of cardiac deaths, which might possibility have excluded the association between mortality and serum uric acid in this study population. The other limitation was the possibility of a selection bias because the study population mainly consisted of referred patients from local clinics, and these patients underwent coronary angiography. However, our results demonstrated the clinical significance of serum uric acid in those patients.
In summary, this observational study demonstrates that the serum uric acid level, acute coronary syndrome and multi-vessel disease are associated with MACEs in patients with CAD. Cardiac patients with hyperuricemia may require more aggressive secondary prevention to prevent the development of future cardiac events.
Figures and Tables
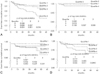 | Fig. 1Kaplan-Meier curve for event-free cumulative survival according to the quartiles of the serum uric acid levels. A: for all major adverse cardiovascular events. B: for acute myocardial infarction. C: for percutaneous coronary intervention. D: for congestive heart failure. See table 1 for the serum uric acid quartiles, and the figures on the X-axis represent months. |
Table 1
Demographics of study population

Data are expressed as mean±SD. BMI: body mass index, ACS: acute coronary syndrome, LVEF: left ventricular ejection fraction, H(L)DL: high (low) density lipoprotein, ACE: angiotensin converting enzyme. The number (percent) of patients and level of serum uric acid in each quartiles are; quartile 1=167 (25.3%), ≤3.88 mg/dL; quartile 2=164 (24.8%), >3.88 mg/dL and ≤4.85 mg/dL; quartile 3=170 (25.8%), >4.85 mg/dL and ≤5.74 mg/dL; quartile 4=159 (24.1%), >5.74 mg/dL
Table 3
Hazard ratio of clinical variables for major adverse cardiovascular events by univariate Cox regression analysis

Table 4
Independent factors of major adverse cardiovascular events by multivariate Cox regression analysis (p>0.10 to remove in table 3)

References
1. Hare JM, Johnson RJ. Uric acid predicts clinical outcomes in heart failure: insights regarding the role of xanthine oxidase and uric acid in disease pathophysiology. Circulation. 2003. 107:1951–1953.
2. Mercuro G, Vitale C, Cerquetani E, et al. Effect of hyperuricemia upon endothelial function in patients at increased cardiovascular risk. Am J Cardiol. 2004. 94:932–935.
3. Ward HJ. Uric acid as an independent risk factor in the treatment of hypertension. Lancet. 1998. 352:670–671.
4. Cicoira M, Zanolla L, Rossi A, et al. Elevated serum uric acid levels are associated with diastolic dysfunction in patients with dilated cardiomyopathy. Am Heart J. 2002. 143:1107–1111.
5. Bickel C, Rupprecht HJ, Blankenberg S, et al. Serum uric acid as an independent predictor of mortality in patients with angiographically proven coronary artery disease. Am J Cardiol. 2002. 89:12–17.
6. Kojima S, Sakamoto T, Ishihara M, et al. Prognostic usefulness of serum uric acid after acute myocardial infarction (the Japanese Acute Coronary Syndrome Study). Am J Cardiol. 2005. 96:489–495.
7. Anker SD, Doehner W, Rauchhaus M, et al. Uric acid and survival in chronic heart failure: validation and application in metabolic, functional, and hemodynamic staging. Circulation. 2003. 107:1991–1997.
8. Culleton BF, Larson MG, Kannel WB, Levy D. Serum uric acid and risk for cardiovascular disease and death. Ann Intern Med. 1999. 131:7–13.
9. Rich MW. Uric acid: is it a risk factor for cardiovascular disease? Am J Cardiol. 2000. 85:1018–1021.
10. Alderman MH, Cohen H, Madhavan S, Kivlighn S. Serum uric acid and cardiovascular events in successfully treated hypertensive patients. Hypertension. 1999. 34:144–150.
11. Moriarity JT, Folsom AR, Iribarren C, Nieto FJ, Rosamond WD. Serum uric acid and risk of coronary heart disease. Ann Epidemiol. 2000. 10:136–143.
12. Yoo TW, Sung KC, Kim YC, et al. The relationship of the hypertension, insulin resistance, and metabolic syndrome in the serum uric acid level. Korean Circ J. 2004. 34:874–882.
13. McCord JM. Oxygen-derived free radicals in postischemic tissue injury. N Engl J Med. 1985. 312:159–163.
14. Prendergast BD, Sagach VF, Shah AM. Basal release of nitric oxide augments the Frank-Starling response in the isolated heart. Circulation. 1997. 96:1320–1329.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download