Abstract
Background and Objectives
Percutaneous coronary intervention (PCI) of unprotected left main coronary artery (LMCA) stenosis is a promising approach during this era of drug-eluting stents. However, there is no available hemodynamic data on these type patients during the performance of LMCA stenting. The purpose of this study was to determine the risk factors affecting hemodynamic stability during LMCA stenting, and to evaluate whether hemodynamic support such as inotropics or intra-aortic balloon pump (IABP) is needed, based on the risk factors.
Subjects and Methods
From July 2003 to January 2006, we enrolled 92 study patients (Male=55) who had visited Yeungnam University Hospital, Keimyung University Dongsan Hospital and InJe University Baik Hospital in Busan and they were all were diagnosed with angiographically detected unprotected LMCA stenosis. Group 1 (n=69) included those patients who did not need hemodynamic support during PCI. Group 2 (n=23) included patients who needed hemodynamic support during PCI. All patients had stents deployed in the LMCA lesions without hemodynamic support; the clinical, angiographic and procedural outcomes were compared between the two groups after the procedure.
Results
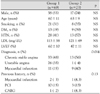
The baseline patient characteristics were not statistically different between the two groups. On univariate analysis, Group 2 had more patients diagnosed with acute myocardial infarction (AMI) than Group 1 (40% vs. 15%, respectively, p=0.014). Group 1 had a greater frequency of an increased left ventricular (LV) ejection fraction than Group 2 (60±10 vs. 47±11, respectively, p=0.01). Regarding the lesion location in the LMCA, Group 2 had relatively more lesions at bifurcated locations than Group 1 (44% vs. 78%, respectively, p=0.004). Group 2 required more complex techniques to repair lesions, such as kissing or crush stenting, than did Group 1 (19% vs. 48%, respectively, p=0.006). Multivariate logistic regression analysis showed that the presence of AMI (Odds Ratio (OR)=3.74, p=0.014), a complex stenting procedure such as kissing or crushing (OR=3.99, p=0.006), a bifurcated lesion (OR=4.58, p=0.004) and poor LV function (OR=9.95, p=0.0001) were independent risk factors for hemodynamic instability during LMCA stenting.
Several studies have reported on the safety and feasibility of stenting the left main coronary artery(LMCA).1-6) The use of drug-eluting stents(DES) has resulted in changing the approach to LMCA stenting, and it is now possible to expand the use of percutaneous coronary intervention(PCI) to include LMCA stenosis.7) In addition to the controversies related to the technical approaches for stent implantation, there is debate about the use of the prophylactic intra-aortic balloon pump(IABP) for LMCA stenting. Elective IABP may provide the optimal hemodynamic support during PCI for the at-risk patients.8) However, despite the potential importance, not much data is available on patients' hemodynamic status during LMCA stenting. Therefore, the purpose of this study was to determine the risk factors that affect hemodynamic stability during LMCA stenting, and to evaluate whether hemodynamic support like IABP is needed based on these risk factors.
From July 2003 to January 2006, 92 consecutive patients(Male n=55) presented to Yeungnam University Medical Center, Keimyung University Dongsan Hospital and Inje University Baik Hospital in Busan, and they underwent PCI for unprotected LMCA stenosis. All the PCI procedures were performed without routine backup hemodynamic support or keeping a prophylactic 4 French sheath in the left femoral artery. We excluded patients who had contraindications for antiplatelet or anticoagulation therapy and who could not provide informed consent for PCI as the first line therapy.
All the patients received aspirin 325 mg orally and a 300 mg loading dose of clopidogrel before coronary angiography(CAG), or after PCI for the emergency cases. The patients were routinely treated with aspirin 200 mg/day, clopidogrel 75 mg/day and/or cilostazol 200 mg/day. The use of glycoprotein IIb/IIIa inhibitors was left to the discretion of the operator.
CAG was performed after administering 0.2 mg of intracoronary nitroglycerin. The blood pressure(BP) was recorded before the procedure and it was continuously monitored during the procedure with using a catheter. IABP was reserved for the emergency cases. Using the guiding catheter for magnification and calibration, we performed quantitative coronary angiography before and after the intervention. The stenting techniques for LMCA included the simple "Cross-over" stenting technique, the "T" stenting technique, the "Crush" stenting technique and the "Kissing" technique at the discretion of the operator and according to the characteristics of the lesion and the anatomy of the left coronary artery. There were two types of available DESs(Cypher, Cordis and Taxus, Boston Scientific, MA., USA) were used at the discretion of the operator. A "Kissing" balloon inflation was the final step of the procedure in all cases with bifurcated lesions.
The LMCA was considered to be unprotected if there were no patent coronary artery bypass grafts in the left anterior descending artery(LAD) or the left circumflex artery(LCX). Procedure-related hypotension was defined as an augmented systolic BP<90 mmHg lasting more than 10 minutes without hemodynamic support such as inotropics or IABP. Procedural success was defined as successful treatment of the LMCA with final TIMI 3 flow and a diameter stenosis <30%, in addition to the absence of death, myocardial infarction(MI) and repeat PCI for the treated lesion during the index hospitalization.
The data are expressed as means±SDs for the continuous variables, and as frequencies for the categorical variables. A two tailed student's test was used to test the differences among continuous variables. The χ2 test was used for comparison of the categorical variables. The contribution of clinical, angiographic and procedural variables to the clinical outcome was evaluated via multivariate logistic regression analysis; all variables with a p≤0.10 on the univariate analysis were included into the model. Probability values <0.05 were considered significant. The data was analyzed with using SPSS 12.0 for Windows(SPSS, Chicago, IL., USA).
We divided the study population into two groups: Group 1(n=69) did not need hemodynamic support and Group 2(n=23) required hemodynamic support due to their procedure related hypotension.
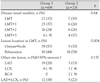
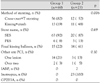
The baseline clinical characteristics did not differ between the two groups except for acute MI; this was more common in Group 2 than in Group 1(40% vs. 15%, respectively, p=0.014). In addition, Group 1 had a greater increased level of the left ventricular(LV) ejection fraction(EF) than Group 2(60±10 vs 47±11, respectively, p=0.01)(Table 1). The quantitative coronary angiographic data is shown in Table 2. Comparison of the angiographic characteristics between the two groups showed that the numbers of diseased vessels and lesions with stenosis greater than 50%, except for the main vessel, were not statistically different between the two groups; however, Group 2 had a greater number of bifurcated lesions compared to Group 1(44% vs 78%, respectively, p=0.004)(Table 3). Table 4 shows the clinical findings during the PCI procedure. Simple stenting techniques such as cross-over or T stenting were more common in Group 1(82% vs. 52%, respectively), and complex stenting techniques such as kissing or crush stenting were more frequently used in Group 2(19% vs 48%, respectively, p=0.006). Sirolimus eluting stents(Cypher) were most commonly used for stent implantation in both groups(92% in Group 1, 87% in Group 2, p=0.1). The patients in group 2 required IABP on two occasions; no patient in Group 1 and all of the patients in Group 2(n=23) needed inotropics for hemodynamic support. There were no differences in the use of glycoprotein IIb/IIIa inhibitors between the two groups. From the multivariate logistic regression analysis, the occurrence of MI(Odds ratio(OR)=3.74, p=0.014), the use of complex stenting procedures such as kissing or crushing(OR=3.99, p=0.006), the presence of bifurcated lesions(OR=4.58, p=0.004) and poor LV function such as an LVEF below 45%(OR=9.95, p=0.0001) were independent predictors of hemodynamic instability during LMCA stenting(Table 5)(Fig. 1). Table 6 shows the in-hospital outcomes of stenting in the patients with LMCA stenosis. There was 1 death and 1 myocardial infarction in group 2; during PCI in a 68 year old female, LCX stent distal dissection developed and an IABP was inserted. The patient was diagnosed with non-ST elevation myocardial infarction and the patient survived after IABP and supportive care. Another patient was a 55 year old male who developed cardiogenic shock after PCI. He didn't survive even after aggressive treatment, including IABP. There were no major adverse cardiovascular events in group 1.
LMCA disease is found in 4 to 9% of the diagnostic CAG procedures.9) Coronary artery bypass grafting(CABG) has been the first line treatment for LMCA. The recent emergence of DES has dramatically reduced the risk of complications following PCI, and these complications are mainly due to the dramatic reduction in the restenosis rate of various subsets of lesion.10) Perhaps the less invasive LMCA stenting with DES may help decrease the frequency of CABG; this may lead to a reduction of the frequency of acute coronary vessel occlusion as well as a decrease in the restenosis rate that develops with balloon angioplasty or bare metal stent(BMS) procedures. Currently, surgery is often replaced with LMCA stenting in selected cases. Although the frequency of DES implantation for LMCA stenting is increasing, the use of IABP during LMCA stenting remains controversial.
Prior studies have reported a wide range, from 3% to 50%, of using elective IABP.11-17) The percutaneous intervention guidelines recommend that cardiopulmonary support, for high-risk PCI, should be reserved for those patients at the extreme end of the spectrum of hemodynamic compromise, such as those patients with extremely depressed LV function and patients in cardiogenic shock.18) This recommendation suggests the importance of defining the clinical and/or angiographic factors that affect hemodynamic compromise during PCI in order to identify the high risk patients such as those suffering with LMCA stenosis. Briguori et al.8) suggested that elective use of IABP support may be useful to: 1) maintain pressure and flow across the arterial system during LMCA occlusion,19) 2) maintain perfusion during manipulation of the left main coronary artery and limit the ischemic cycles,20) and 3) maintain hemodynamic stabilization so as to allow the operator to better focus and concentrate. In addition to its many advantages, IABP also has many disadvantages, including peripheral vascular complications and bleeding during the PCI.21-24) Even if the rate of complications with employing IABP is low, the other problems to be considered are its expense and the time needed to insert it. Therefore, it is important to select only those patients who are at high risk before inserting IABP during LMCA stenting.
In patients with normal LV function during LMCA stenting, routine prophylactic IABP is not needed for hemodynamic support because the normal functioning myocardium can endure the temporary ischemia caused by balloon occlusion. However, in patients with decreased LV function and severe hemodynamic changes during the procedure, IABP may be helpful and useful for preventing procedure-related complications.
In this study, we determined the risk factors for hemodynamic instability in the patients undergoing LMCA stenting. These risk factors were poor LV function, complex stent procedures such as kissing or crushing, lesion located in the LMCA and the diagnosis of AMI. Among them, the most important risk factor during LMCA stenting was poor LV function.
We also determined the risk factors during the procedure of unprotected LMCA stenting, and we found that elective LMCA stenosis stenting without the above-noted risk factors can result in successful outcomes regardless of using hemodynamic support. We collected data on LMCA stenosis stenting without hemodynamic support as part of this study. The findings showed that it is possible to implant a stent in a LMCA lesion without prophylactic use of IABP. However, if risk factors are present, then additional care is needed when deploying the stent; administering hemodynamic support, including IABP, should considered as part of the treatment for these patients.
In conclusion, the results of this study showed that routine backup hemodynamic support is not always necessary when performing LMCA stenting. However, hemodynamic support, including IABP or inotropics, should be considered before the performing this procedure in high risk patients.
Figures and Tables
 | Fig. 1The risk factors and odds ratio for hemodynamic instability during left main coronary artery stenting. The identified risk factors were the presence of acute myocardial infarction (AMI), use of complex stenting techniques (kissing or crushing), the lesion location (bifurcated lesion) and poor left ventricular (LV) function (especially a left ventricular ejection fraction (LVEF) <45%); the odds ratio for poor LV function was the most significant predictive factor. |
References
1. Lopez JJ, Ho KK, Stoler RC, et al. Percutaneous treatment of protected and unprotected left main coronary stenoses with new devices: immediate angiographic results and intermediate-term follow-up. J Am Coll Cardiol. 1997. 29:345–352.
2. Ellis SG, Tamai H, Nobuyoshi M, et al. Contemporary percutaneous treatment of unprotected left main coronary stenoses: initial results from a multicenter registry analysis 1994-1996. Circulation. 1997. 96:3867–3872.
3. Park SJ, Park SW, Hong MK, et al. Long-term(three year) outcomes after stenting of unprotected left main coronary artery stenosis in patients with normal left ventricular function. Am J Cardiol. 2003. 91:12–16.
4. Tan WA, Tamai H, Park SJ, et al. Long-term clinical outcomes after unprotected left main trunk percutaneous revascularization in 279 patients. Circulation. 2001. 104:1609–1614.
5. Park SJ, Park SW, Hong MK, et al. Stenting of unprotected left main coronary artery stenosis without angicoagulation: immediate and late outcomes. Korean Circ J. 1997. 27:947–957.
6. Park JH, Cho YH, Lee SH, et al. Long term clinical follow-up in patients with left main coronary disease according to treatment strategies. Korean Circ J. 2003. 33:568–573.
7. Park SJ, Lee CH, Kim YH, et al. Technical feasibility safety, and clinical outcome of stenting of unprotected left main coronary artery bifurcation narrowing. Am J Cardiol. 2002. 90:374–378.
8. Briguori C, Airoldi F, Chieffo A, et al. Elective versus provisional intraaortic balloon pumping in unprotected left main stenting. Am Heart J. 2006. 152:565–572.
9. Lenzen MJ, Boersma E, Bertrand ME, et al. Management and outcome of patients with established coronary artery disease. Eur Heart J. 2005. 26:1169–1179.
10. Moses JW, Leon MB, Popma JJ, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003. 349:1315–1323.
11. Chieffo A, Stankovic G, Bonizzoni E, et al. Early and mid-term results of drug-eluting stent implantation in unprotected left main. Circulation. 2005. 111:791–795.
12. Valgimigli M, van Mieghem CA, Ong AT, et al. Short and long term clinical outcome after drug eluting stent implantation for the percutaneous treatment of left main coronary artery disease: insights from the Rapamycin-eluting and Taxus Stent Evaluated At Rotterdam Cardiology Hospital registries(RESEARCH and T-SEARCH). Circulation. 2005. 111:1383–1389.
13. Park SJ, Kim YH, Lee BK, et al. Sirolimus eluting stent implantation for unprotected left main coronary artery stenosis: comparison with bare metal stent implantation. J Am Coll Cardiol. 2005. 45:351–356.
14. Black A, Cortina R, Bossi I, Choussat R, Fajadet J, Marco J. Unprotected left main coronary artery stenting: correlates of midterm survival and impact of patient selection. J Am Coll Cardiol. 2001. 37:832–838.
15. Park SJ, Hong MK, Lee CW, et al. Elective stenting of unprotected left main coronary artery stenosis: effect of debulking before stenting and intravascular untrasound guidance. J Am Coll Cardiol. 2001. 38:1054–1060.
16. Takagi T, Stankovic G, Finci L, et al. Results and long-term predictors of adverse clinical events after elective percutaneous interventions on unprotected left main coronary artery. Circulation. 2002. 106:698–702.
17. Kelley MP, Klugherz BD, Hashemi SM, et al. One-year clinical outcomes of protected and unprotected left main coronary artery stenting. Eur Heart J. 2003. 24:1554–1559.
18. Smith SC Jr, Dove JT, Jacobs AK, et al. ACC/AHA guidelines of percutaneous coronary interventions(revision of the 1993 PTCA guidelines)-executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines(committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty). J Am Coll Cardiol. 2001. 37:2215–2239.
19. Szatmary LJ, Marco J. Haemodynamic and antiischemic protective effects of intraaortic balloon counterpulsation in high risk coronary heart patients undergoing percutaneous transluminal coronary angioplasty. Cor Vasa. 1987. 29:183–191.
20. Kern MJ, Aguirre F, Bach R, Donohue T, Siegel R, Segal J. Augmentation of coronary blood flow by intra-aortic balloon pumping in patients after coronary angioplasty. Circulation. 1993. 87:500–511.
21. Dietl CA, Berkheimer MD, Woods EL, Gilbert CL, Pharr WF, Benoit CH. Efficacy and cost-effectiveness of preoperative IABP in patients with ejection fraction of 0.25 or less. Ann Thorac Surg. 1996. 62:401–409.
22. Stone GW, Marsalese D, Brodie BR, et al. A prospective randomized evaluation of prophylactic intraaortic balloon counterpulsation in high risk patients with acute myocardial infarction treated with primary angioplasty. J Am Coll Cardiol. 1997. 29:1459–1467.
23. Van't Hof AW, Liem AL, de Boer MJ, Hoomtje JC, Suryapranata H, Zijlstra F. A randomized comparison of intraaortic balloon pumping after primary coronary angioplasty in high risk patients with acuty myocardial infarction. Eur Heart J. 1999. 20:659–665.
24. Alderman JD, Gabliani GI, McCabe CH, et al. Incidence and management of ischemia with percutaneous wire guided intraaortic balloon catheters. J Am Coll Cardiol. 1987. 9:524–530.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download