Abstract
Bilateral patella tendon rupture is rare, particulary when associated with osteogenesis imperfecta. Brittleness of the bone in osteogenenesis imperfect patients may cause this rupture. We report on this rare case and suggest the direct repair with the additional wire loop as a proper treatment option for patients with the substantial rupture of patella tendon.
Bilateral patellar tendon rupture is rare and there are only a few case reports that are associated with osteogenesis imperfecta.1) In addition, it has never been report in this country. We report a case of bilateral simultaneous patellar tendon rupture in a 55-year-old female with underlying osteogenesis imperfecta. This is a congenital disorder that results from a mutation of the genes that codeos r ftype I collagen and expresses itself clinically by bone fragility, and similar manifestations result in tissue weakness in the tissues whicha hs type I collagen as the principal matrix protein (bone, dentin, sclerae, tendon, and ligaments).
A 55-year-old female admitted to our hospital due to bilateral knee pain. The pain occurred during working without obvious trauma episode. She had no history of anterior knee pain prior to this event. She had notable bruises and swelling on both knees, and was unable to raise thigh on both legs. Plain radiographs revealed patella alta and fracture of patellar inferior pole on both sides (Fig. 1). Computed tomography scan was taken on both knees and magnetic resonance imaging was also performed on the right knee (Fig. 2). The radiologic finding suggests the identical avulsion fracture of patellar at the inferior pole on both knees with accompanying patellar tendon rupture on the right knee. Decision was made to repair the patellar tendon on both knee and the operation was performed on the day of the visit. Total rupture of the patellar tendon rupture was confirmed in the operation and the repair was done on both sides using Ethibond suture for patellar tendon rupture with additional wire loop to fixate fragile patellar bone (Fig. 3). At 10 months follow-up, the patient was able to flex the knees up to 100 degrees and was able to perform straight legs raise on both knees (Fig. 4). She was able to return to similar level of activity as compare to the condition before the operation.
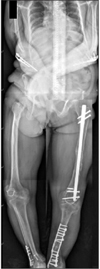
The patient had been admitted to the hospital thirteen times itnhe past for multiple fractures (Fig. 5) and the diagnosis of osteogenesis imperfecta (type I Sillence) had been made previously. The family history reveals her farther, her older brother and her daughter also have osteogenesis imperfecta. Prior to the current operation, she underwent the corrective osteotomy and plating due to the anterior bowing of left tibia 30 years ago. Also she underwent open reduction and internal fixation for a left femoral shaft fracture, but was re-operated after the plate removal, since she had a re-fracture in the left femoral shaft. Consequently, the femoral shaft fracture had to be stabilized with a unilateral external fixator and then the external fixation was converted to intramedullary nail fixation with corrective osteotomy 10 years ago. In addition, she had open reduction and internal fixation for the right ankle bimalleolar fracture 2 years ago.
The quadriceps tendon, the patella bone, and the patellar tendon form a biomechanical functional complex that transmits the contraction of the quadriceps muscle to the tibial bone, allowing extension of the knee joint.2) Injuries to this complex can be caused by direct or indirect trauma and usually involves the patella bone. The vast majority of patellar fracture occurs unilateral.2) In very rare cases, however, patients may present with simultaneous bilateral tendon ruptures.
Three mechanisms have been proposed as possible causes of structural abnormalities of the patella tendon: (1) systemic disorders, such as lupus erythematosus, diabetes mellitus, rheumatologic disease, chronic renal insufficiency, and hyperparathyroidism have been associated with a higher risk for tendon ruptures. (2) Chronic local stress on both knees can result in repeated microtraumas of ligamentous structures, inducing inflammatory and degenerative changes. This has been demonstrated previously in histological specimens of patella tendons harvested from patients with a history of stress to the knee. (3) Local or systemic administration of steroids has been associated with the susceptibility of the tendon ruptures, but its significance is still controversial. However, in our case, we did not find any of these associated conditions other than the osteogenesis imperfecta.
These matrix abnormalities affect the mineral phase. Compared with age-matched controls, the bone quality in osteogenesis imperfecta patients shows a higher average score in bone mineral density. These disturbances are associated with the altered biomechanical behavior. Mineralized osteogenesis imperfecta bone may be harder at the material level, but it breaks more easily when it is deformed, and fatigue damage accumulates much faster during repetitive loading.3) The sum of these abnormalities may explain the brittleness of the osteogenesis imperfecta bone.
In addition, osteogenesis imperfecta is characterized by an insufficient amount of bone. Both cortical thickness and the amount of trabecular bone are low.4) We think that the patella tendon rupture with fracture of patella inferior pole was caused by the brittleness in this patient. Tendon rupture in osteogenesis imperfecta patients has been reported in several cases.567) And bilateral occurence at tendon insertion site is common. Surgical repair is the most common treatment for ruptured patella tendon. The principle techniques involve primary repair with and without augmentation of the tendon.8)
Techniques for augmentation include tendon reconstruction using gracilis or semitendinosus grafts.9) Augmentation is usually used in cases where the structure of the patella tendon has been reduced in its substance or when the surgical repair is delayed. Additional implantation of patellotibial wire loops improves the stability of the tendon repair over the primary direct suture alone therefore may allow earlier postoperative mobilization and more intensive physiotherapy. It does, however, require a second operative intervention to remove the loops. The use of circlage wiring in patients with bilateral patella tendon rupture is controversial; while some authors strongly recommends it, others consider it unnecessary.10) We thought that only using non-absorbable sutures for direct repair cannot get rigid fixation due to the brittleness of osteogenesis imperfecta. Thus, additional wire loop was applied
We report the very rare case of bilateral simultaneous patella tendon rupture associated with osteogenesis imperfecta. The authors believe if the patient has the substance rupture of patella tendon, a direct repair with the additional wire loop is a proper treatment option.
Figures and Tables
Figure 1
Plain radiographs showed patella alta and fracture of the patellar inferior pole on both sides.

Figure 2
Computed tomography scan was taken on both knees and magnetic resonance imaging was also performed on the right knee. (A) The identical avulsion fracture of patellar at the inferior pole on both knees. (B) Patellar tendon rupture on the right knee.

Figure 3
Postoperative radiographs. The repair was done on both sides using Ethibond suture for patellar tendon rupture with an additional wire loop to fixate the fragile patellar.

References
1. Kothari P, Mohan N, Hunter JB, Kerslake R. Case report. Bilateral simultaneous patellar tendon ruptures associated with osteogenesis imperfecta. Ann R Coll Surg Engl. 1998; 80:416–418.
2. Müller KH, Knopp W. Ruptures of the tendons of the extensor system of the knee joint. Unfallchirurgie. 1984; 10:254–261.
3. Jepsen KJ, Schaffler MB, Kuhn JL, Goulet RW, Bonadio J, Goldstein SA. Type I collagen mutation alters the strength and fatigue behavior of Mov13 cortical tissue. J Biomech. 1997; 30:1141–1147.

4. Rauch F, Travers R, Parfitt AM, Glorieux FH. Static and dynamic bone histomorphometry in children with osteogenesis imperfecta. Bone. 2000; 26:581–589.

5. Dent CM, Graham GP. Osteogenesis imperfecta and Achilles tendon rupture. Injury. 1991; 22:239–240.

6. Imbert P, Loy S. Rupture in the palm of a flexor tendon in a young man with osteogenesis imperfecta. Chir Main. 1999; 18:290–294.
7. Ogilvie-Harris DJ, Khazim R. Tendon and ligament injuries in adults with osteogenesis imperfecta. J Bone Joint Surg Br. 1995; 77:155–156.

9. Rosenberg JM, Whitaker JH. Bilateral infrapatellar tendon rupture in a patient with jumper's knee. Am J Sports Med. 1991; 19:94–95.

10. Kuo RS, Sonnabend DH. Simultaneous rupture of the patellar tendons bilaterally: case report and review of the literature. J Trauma. 1993; 34:458–460.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download