Abstract
Purpose
We aimed to report the clinical results of diaphyseal osteoplasty and primary soft tissue closure in recalcitrant poor skin lesion with superficial or localized bone infection on the anterior shin after chronic osteomyelitis.
Materials and Methods
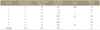
We retrospectively reviewed 7 patients with poor shin skin lesion complicated by superficial and localized bone infection after chronic osteomyelitis. The average duration of chronic osteomyelitis was 39 years. After excision of the poor skin lesion, diaphyseal osteoplasty of the tibia was performed for the resection of infected bone and primary closure of the soft tissue defect. Postoperative results were evaluated with recovery of skin lesion, the amount of bone resection by osteoplasty and complications including recurrence of osteomyelitis.
Results
Mean size of excised skin lesion during surgery was 3.0×14.1 cm and successful primary closures of the defect were possible in all cases. All shin skin lesions were recovered and the amount of resected bone was mean of 18.7% of the anteroposterior diameter of the tibia. There was no recurrence of skin lesion, osteomyelitis or stress fracture.
Conclusion
After treatment of a previous intramedullary infection in chronic osteomyelitis of the tibia, recalcitrant poor shin skin lesion complicated with superficial or localized bone infection was effectively recovered by diaphyseal osteoplasty and primary soft tissue closure. This procedure is relatively simple compared to other surgeries and effective in recovery of healthy shin skin without recurrence of osteomyelitis.
Figures and Tables
Figure 1
Schematic diagrams of diaphyseal osteoplasty. (A) Preoperative axial extent of poor skin lesion (between a and b). Asterisk indicates the amount of bone supposed to be resected. (B) Postoperative apposition of the defect (ab) by soft tissue primary closure.

Figure 2
Photographs of diaphyseal osteoplasty. (A) Preoperative finding of the left shin shows papered thinned scarring and exposure of infected bone. Planned scar excision (B) and osteoplasty with bone chisel (C). (D) Postoperative finding shows successful primary closure.

Figure 3
Resection rate was calculated by measurement of preoperative (a) and postoperative (b) anteroposterior diameters of the tibia at the same height (h) on a lateral X-ray.

Figure 4
Photographs and X-rays of the case 1 patient. (A) A 72-year-old male patient had a skin problem in the middle 1/3 of his left shin for 50 years. The soft tissue defect (4×16 cm) and surrounding poor skin condition were noted. (B) Postoperative radiographs after saucerization and diaphyseal osteoplasty with bone resection showed a straightened anterior cortex of the tibia. (C) Tension-free approximation and additional release on the lateral part of the leg were performed and the resultant defect was covered by a full thickness skin graft. (D) Radiographs 16 months after the operation show a completely healed lesion and acceptable remodeling.

Figure 5
Photographs and X-rays of the case 4 patient. (A) A 73-year-old female patient had skin problem in the mid-leg for 60 years. Thinned papered poor shin skin (5×20 cm) and multiple bone exposure with sinus drainage implied chronic osteomyelitis. Radiographs showed an impending pathologic fracture. (B) Under the impression of chronic osteomyelitis, sequestrectomy, diaphyseal osteoplasty, and external fixation were performed. After release of deep fascia, tension-free approximation was possible without additional treatment. (C) At 1 year follow-up, healthy normal skin with a linear scar was observed on the mid leg and radiographs showed a well remodeled tibia shaft.

References
1. Seligson D, Klemm K. Adult posttraumatic osteomyelitis of the tibial diaphysis of the tibial shaft. Clin Orthop Relat Res. 1999; 360:30–36.
2. Green NE, Edwards K. Bone and joint infections in children. Orthop Clin North Am. 1987; 18:555–576.
3. Reckling FW, Rosen H. Treatment of infected tibial fractures: posterior vs anterior bone grafting techniques. Orthopedics. 1991; 14:1025–1030.
4. Fisher J. Soft tissue coverage of bone: a historical perspective and review. Eur J Plast Surg. 1986; 9:13–17.
5. Thul JR, Stone ML, Goodin CV Jr. Primary wound closure in chronic osteomyelitis. J Foot Surg. 1984; 23:31–34.
6. Musharafieh R, Osmani O, Musharafieh U, Saghieh S, Atiyeh B. Efficacy of microsurgical free-tissue transfer in chronic osteomyelitis of the leg and foot: review of 22 cases. J Reconstr Microsurg. 1999; 15:239–244.
7. Cierny G 3rd, Mader JT. Approach to adult osteomyelitis. Orthop Rev. 1987; 16:259–270.
8. Daoud A, Saighi-Bouaouina A. Treatment of sequestra, pseudarthroses, and defects in the long bones of children who have chronic hematogenous osteomyelitis. J Bone Joint Surg Am. 1989; 71:1448–1468.
9. Patzakis MJ, Abdollahi K, Sherman R, Holtom PD, Wilkins J. Treatment of chronic osteomyelitis with muscle flaps. Orthop Clin North Am. 1993; 24:505–509.
10. Fodor L, Horesh Z, Lerner A, Ramon Y, Peled IJ, Ullmann Y. The distally based sural musculoneurocutaneous flap for treatment of distal tibial osteomyelitis. Plast Reconstr Surg. 2007; 119:2127–2136.
11. Hahn SB, Kang HJ, Joo SY. Sural artery flap for the treatment of osteomyelitis of the lower leg. J Korean Orthop Assoc. 2009; 44:54–60.
12. Kim HM, Park CS, Kim YS, Chu IT, Cho SR. Medial gastrocnemius myocutaneous flap for soft tissue defect of anteromedial aspect of leg. J Korean Orthop Assoc. 1993; 28:1795–1801.
13. May JW Jr, Gallico GG 3rd, Lukash FN. Microvascular transfer of free tissue for closure of bone wounds of the distal lower extremity. N Engl J Med. 1982; 306:253–257.
14. Weiland AJ, Moore JR, Daniel RK. The efficacy of free tissue transfer in the treatment of osteomyelitis. J Bone Joint Surg Am. 1984; 66:181–193.
15. Arnold PG, Mixter RC. Making the most of the gastrocnemius muscles. Plast Reconstr Surg. 1983; 72:38–48.
16. Cavadas PC. The split medial gastrocnemius muscle flap. Plast Reconstr Surg. 1998; 102:1782–1783.
17. Lee JM, Song KH, Park JH. Muscle free flap transplantation in chronic osteomyelitis of the lower extremities. J Korean Soc Microsurg. 2009; 18:49–54.
18. Perrot P, Bouffaut AL, Perret C, Connault J, Duteille F. Risk factors and therapeutic strategy after failure of free flap coverage for lower-limb defects. J Reconstr Microsurg. 2011; 27:157–162.
19. Parsons B, Strauss E. Surgical management of chronic osteomyelitis. Am J Surg. 2004; 188:1A Suppl. 57–66.
20. Tetsworth K, Cierny G 3rd. Osteomyelitis debridement techniques. Clin Orthop Relat Res. 1999; 360:87–96.
21. Fodor L, Ullmann Y, Soudry M, Calif E, Lerner A. Prophylactic external fixation and extensive bone debridement for chronic osteomyelitis. Acta Orthop Belg. 2006; 72:448–453.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download