Abstract
Juvenile idiopathic scoliosis includes scoliosis diagnosed from three to ten years old according to the chronological age. Spine growth in juveniles does not occur at a rapid rate spinal deformity does not show rapid progress. However, because of the intimate relationship between chest wall growth and the spine, decrease of chest wall capacity due to scoliosis could lead to development of cardiovascular and pulmonary complication, especially in early age. In scoliosis in early age, other causes of the deformity including neurological problems should be evaluated. If the scoliosis angle is more than 25 degrees, it could progress very easily, thus aggressive treatment is needed. A new growing-sparing surgical technique (growing rod and growth modulation) is introduced for improvement of spine and chest growth, and for prevention of crankshaft phenomenon.
Figures and Tables
Figure 1
Spinal growth from ages 1 through 15 years. Spinal growth decelerates during the juvenile period, between the age of 5 and 10 years. There is a second acceleration of the growth rate along with the puberty in the adolescent period. Therefore, early onset scoliosis is often defined as scoliosis that manifests before the age of 5 years, as compared to late onset scoliosis which manifests after the age of 5 years.
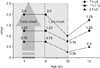
Figure 2
Growth of spine and thorax. The thoracic volume is 5% adulthood at birth, which increases to more than 30% at the age of 5 years. Early onset of scoliosis relates to reduced spinal length, which can ultimately lead to decreased thoracic volume and increased risk of pulmonary complications.

Figure 3
Serial radiographs of a 7-year-old boy with an initial deformity curve of 30 degrees. A 1 month follow-up radiograph showed resolution of the curve. After 2 months, a curve measuring 15 degrees is seen again in the radiograph. This case demonstrates the features of juvenile idiopathic scoliosis well.
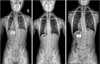
Figure 4
Tuning/balancing mechanism. Tuning/balancing mechanism is a characteristic feature of juvenile idiopathic scoliosis which the Cobb angle shows variation over time. The process of progression, quit and regression can be seen. Figure shows x is the onset time of scoliosis in growing spine; y is the time when curve will follow one of three pathway (A: regression; B: quit and C: progression); and z is the time of change in treatment approach.

Figure 5
(A) A 6 year and 9 month-old boy with a 29 degree of scoliosis in the radiograph. (B) Magnetic resonance imaging scan of the spine revealed syringomyelia (big arrow) with Chiari malformation (small arrow) in the cord and surgical treatment was performed. (C) After surgery, signs of syringomyelia has improved and the deformity angle remains stable with the conservative treatment of bracing.

Figure 6
Treatment algorithm of juvenile idiopathic scoliosis (JIS). MRI: magnetic resonance imaging.

References
1. Pehrsson K, Larsson S, Oden A, Nachemson A. Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine (Phila Pa 1976). 1992; 17:1091–1096.

2. Little DG, Sussman MD. The Risser sign: a critical analysis. J Pediatr Orthop. 1994; 14:569–575.
3. Dimeglio A, Canavese F. The growing spine: how spinal deformities influence normal spine and thoracic cage growth. Eur Spine J. 2012; 21:64–70.

4. Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984; 66:1061–1071.

5. Ponseti IV, Friedman B. Prognosis in idiopathic scoliosis. J Bone Joint Surg Am. 1950; 32:381–395.

6. James JI. Idiopathic scoliosis; the prognosis, diagnosis, and operative indications related to curve patterns and the age at onset. J Bone Joint Surg Br. 1954; 36:36–49.
9. Tolo VT, Gillespie R. The characteristics of juvenile idiopathic scoliosis and results of its treatment. J Bone Joint Surg Br. 1978; 60:181–188.

10. Mannherz RE, Betz RR, Clancy M, Steel HH. Juvenile idiopathic scoliosis followed to skeletal maturity. Spine (Phila Pa 1976). 1988; 13:1087–1090.

11. Modi HN, Suh SW, Yang JH, Hong JY, Venkatesh K, Muzaffar N. Spontaneous regression of curve in immature idiopathic scoliosis - does spinal column play a role to balance? An observation with literature review. J Orthop Surg Res. 2010; 5:80.

12. Navarro R, Olavarria G, Seshadri R, Gonzales-Portillo G, McLone DG, Tomita T. Surgical results of posterior fossa decompression for patients with Chiari I malformation. Childs Nerv Syst. 2004; 20:349–356.

13. Tubbs RS, McGirt MJ, Oakes WJ. Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg. 2003; 99:291–296.

14. Alzate JC, Kothbauer KF, Jallo GI, Epstein FJ. Treatment of Chiari I malformation in patients with and without syringomyelia: a consecutive series of 66 cases. Neurosurg Focus. 2001; 11:E3.
15. Park JK, Gleason PL, Madsen JR, Goumnerova LC, Scott RM. Presentation and management of Chiari I malformation in children. Pediatr Neurosurg. 1997; 26:190–196.

16. Ellenbogen RG, Armonda RA, Shaw DW, Winn HR. Toward a rational treatment of Chiari I malformation and syringomyelia. Neurosurg Focus. 2000; 8:E6.

17. Krieger MD, McComb JG, Levy ML. Toward a simpler surgical management of Chiari I malformation in a pediatric population. Pediatr Neurosurg. 1999; 30:113–121.

18. Gupta P, Lenke LG, Bridwell KH. Incidence of neural axis abnormalities in infantile and juvenile patients with spinal deformity. Is a magnetic resonance image screening necessary? Spine (Phila Pa 1976). 1998; 23:206–210.
19. Lewonowski K, King JD, Nelson MD. Routine use of magnetic resonance imaging in idiopathic scoliosis patients less than eleven years of age. Spine (Phila Pa 1976). 1992; 17:S109–S116.

20. Bell J, Parker KL, Swinford RD, Hoffman AR, Maneatis T, Lippe B. Long-term safety of recombinant human growth hormone in children. J Clin Endocrinol Metab. 2010; 95:167–177.

21. Craig ME, Cowell CT, Larsson P, et al. Growth hormone treatment and adverse events in Prader–Willi syndrome: data from KIGS (the Pfizer International Growth Database). Clin Endocrinol (Oxf). 2006; 65:178–185.

22. Kim JY, Rosenfeld SR, Keyak JH. Increased prevalence of scoliosis in Turner syndrome. J Pediatr Orthop. 2001; 21:765–766.

23. Hoikka V, Ylikoski M, Tallroth K. Leg-length inequality has poor correlation with lumbar scoliosis. A radiological study of 100 patients with chronic low-back pain. Arch Orthop Trauma Surg. 1989; 108:173–175.
24. Papaioannou T, Stokes I, Kenwright J. Scoliosis associated with limb-length inequality. J Bone Joint Surg Am. 1982; 64:59–62.

25. Dobbs MB, Weinstein SL. Infantile and juvenile scoliosis. Orthop Clin North Am. 1999; 30:331–341.

26. Dabney KW, Bowen JR. Juvenile idiopathic scoliosis. Semin Spine Surg. 1991; 3:254–265.
27. Klemme WR, Denis F, Winter RB, Lonstein JW, Koop SE. Spinal instrumentation without fusion for progressive scoliosis in young children. J Pediatr Orthop. 1997; 17:734–742.

28. Dubousset J, Herring JA, Shufflebarger H. The crankshaft phenomenon. J Pediatr Orthop. 1989; 9:541–550.

29. Sanders JO, Herring JA, Browne RH. Posterior arthrodesis and instrumentation in the immature (Risser-grade-0) spine in idiopathic scoliosis. J Bone Joint Surg Am. 1995; 77:39–45.

30. Akbarnia BA, Marks DS, Boachie-Adjei O, Thompson AG, Asher MA. Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine (Phila Pa 1976). 2005; 30:S46–S57.
31. Bess S, Akbarnia BA, Thompson GH, et al. Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am. 2010; 92:2533–2543.
32. Akbarnia BA, Asher MA, Bagheri R, et al. Complications of dual growing rod technique in early onset scoliosis: can we identify risk factors? Spine. 2006; Meeting Abstract: Scoliosis Research Society:73. DOI: 10.1097/01.brs.0000317612.97782.9e.
33. Sankar WN, Skaggs DL, Emans JB, et al. Neurologic risk in growing rod spine surgery in early onset scoliosis: is neuromonitoring necessary for all cases? Spine (Phila Pa 1976). 2009; 34:1952–1955.
34. Miladi L. Magnetic powered extensible rod for thorax or spine. In : 45th Annual Meeting of the Scoliosis Research Society; 2010 Sep 21-24; Kyoto, Japan.
35. Akbarnia BA, Mundis GM Jr, Salari P, Yaszay B, Pawelek JB. Innovation in growing rod technique: a study of safety and efficacy of a magnetically controlled growing rod in a porcine model. Spine (Phila Pa 1976). 2012; 37:1109–1114.
36. Keller PM, Lindseth RE, DeRosa GP. Progressive congenital scoliosis treatment using a transpedicular anterior and posterior convex hemiepiphysiodesis and hemiarthrodesis. A preliminary report. Spine (Phila Pa 1976). 1994; 19:1933–1939.
37. King AG, MacEwen GD, Bose WJ. Transpedicular convex anterior hemiepiphysiodesis and posterior arthrodesis for progressive congenital scoliosis. Spine (Phila Pa 1976). 1992; 17:S291–S294.

38. Winter RB, Lonstein JE, Denis F, Sta-Ana de. Convex growth arrest for progressive congenital scoliosis due to hemivertebrae. J Pediatr Orthop. 1988; 8:633–638.

39. Winter RB. Convex anterior and posterior hemiarthrodesis and hemiepiphyseodesis in young children with progressive congenital scoliosis. J Pediatr Orthop. 1981; 1:361–366.

40. Wall EJ, Bylski-Austrow DI, Kolata RJ, Crawford AH. Endoscopic mechanical spinal hemiepiphysiodesis modifies spine growth. Spine (Phila Pa 1976). 2005; 30:1148–1153.

41. Lalonde NM, Aubin CE, Pannetier R, Villemure I. Finite element modeling of vertebral body stapling applied for the correction of idiopathic scoliosis: preliminary results. Stud Health Technol Inform. 2008; 140:111–115.
42. Puttlitz CM, Masaru F, Barkley A, Diab M, Acaroglu E. A biomechanical assessment of thoracic spine stapling. Spine (Phila Pa 1976). 2007; 32:766–771.

43. Stucker R. Results of treatment of progressive scoliosis with SMA staples. Orthopade. 2009; 38:176–180.
44. Braun JT, Ogilvie JW, Akyuz E, Brodke DS, Bachus KN. Creation of an experimental idiopathic-type scoliosis in an immature goat model using a flexible posterior asymmetric tether. Spine (Phila Pa 1976). 2006; 31:1410–1414.

45. Braun JT, Hoffman M, Akyuz E, Ogilvie JW, Brodke DS, Bachus KN. Mechanical modulation of vertebral growth in the fusionless treatment of progressive scoliosis in an experimental model. Spine (Phila Pa 1976). 2006; 31:1314–1320.

46. Newton PO, Upasani VV, Farnsworth CL, et al. Spinal growth modulation with use of a tether in an immature porcine model. J Bone Joint Surg Am. 2008; 90:2695–2706.

47. Betz RR, Asghar J, Samdani AF. Non-fusion anterior stapling. In : Akbarnia BA, Yazici M, Thompson GH, editors. The growing spine: management of spinal disorders in young children. Berlin, Heidelberg: Springer-Verlag Berlin Heidelberg;2010. p. 568–577.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download