Abstract
Purpose
The purpose of this study was to clarify the difference between the remnant-preserving and remnant-sacrificing techniques in anterior cruciate ligament (ACL) reconstruction using stress test, functional score, 2nd look arthroscopy and magnetic resonance imaging (MRI).
Materials and Methods
Among 66 patients having anatomical ACL reconstruction with the fourstrand hamstring autograft using outside-in technique (FlipCutter®) for the femoral tunnel from April 2012 to April 2014, 23 patients who underwent 2nd look arthroscopy and MRI were included. The remnant-preserving group included 12 patients and the remnant-sacrificing group included 11 patients. The two groups were compared and analyzed with regard to stability (Stress test using GNRB®, pivot shift test), functional assessment (International Knee Documentation Committee [IKDC] scale, Lysholm score, one leg hoop test), and the result of second-look arthroscopy and signal to noise quotient (SNQ) ratio of the graft in MRI.
Results
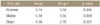
The two groups did not differ significantly in the stability test, IKDC scale, and Lysholm test. The remnant-preserving group showed significant improvement in one leg hoop test compared with the remnant-sacrificing group (p<0.05). The SNQ ratio of the grafted tendon in the remnant-preserving group was significantly lower than those in the remnant-sacrificing group in all regions (p<0.05). In second-look arthroscopy, no significant difference in tension, synovialization, and status of the bundle was observed between the two groups. The grade of synovialization and the status of the bundle in second-look arthroscopy did not influence the signal intensity of the graft in MRI (p>0.05).
Conclusion
More than 12 months after surgery, the graft of the remnant-preserving group showed lower signal intensity compared to that of the remnant-sacrificing group by MRI evaluation. The remnant preserving technique has biological difference compared with the remnant sacrificing technique in human study.
Figures and Tables
 | Figure 1Passage of grafted tendon. Leading sutures lay inside the anterior cruciate ligament (ACL) stump; pictorial description (A), arthroscopic finding (B). After the grafted tendon was passed, it lay inside the center of the ACL stump with circular synovial coverage of its major part. |
 | Figure 2Findings of a second look arthroscopy. Tensions of reconstructed grafts were evaluated subjectively with meticulous probing and it was graded as good, fair, and poor. Good tension was graded if tautness was felt. Fair was graded if the tension was slightly lax, but acceptable. Poor was graded if there was no firm tension. Synovial coverage of the reconstructed graft was graded as 'good' when the synovium covered the entire lengths of the graft, 'fair' when synovial coverage was incomplete, and 'poor' when the synovium covered less than half the lengths of the graft. Status of the fiber bundle was designated as 'good' in case where we could not see the fiber of the graft, 'fair' in case where we could see the fiber but it was not ruptured, 'poor' in case where we could see the fiber but it was ruptured. |
 | Figure 3Postoperative sagittal oblique plan, proton density magnetic resonance image of the knee shows the positions of the 5 regions of interest, which included a distal third (1), middle third (2), proximal third (3), quadriceps tendon (4), and 2 cm anterior to the patellar tendon (5). |
 | Figure 4Comparison of second look arthroscopic findings between the remnant preserving group and the remnant sacrificing group. (A, B) Second look arthroscopy in the remnant sacrificing group showed thin, pale and hypovascular synovial membrane. (C, D) Second look arthroscopy in the remnant preserving group showed thick and hypervascular synovial membrane like normal synovial membrane of the anterior cruciate ligament. |
 | Figure 5Comparison of magnetic resonance imaging (MRI) findings. Sagittal oblique proton density MRI image showed low signal intensity in the graft of the remnant sacrificing group (A) and the remnant preserving group (B). The signal intensity in the remnant preserving group was lower than the signal intensity in the remnant sacrificing group. The remnant tissue of the anterior cruciate ligament was observed in the remnant preserving group. |
References
1. Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL. Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o'clock and 10 o'clock femoral tunnel placement. 2002 Richard O'Connor Award paper. Arthroscopy. 2003; 19:297–304.
2. Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH. Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014; 22:1467–1482.

3. Barrett DS. Proprioception and function after anterior cruciate reconstruction. J Bone Joint Surg Br. 1991; 73:833–837.

4. Ochi M, Iwasa J, Uchio Y, Adachi N, Sumen Y. The regeneration of sensory neurones in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 1999; 81:902–906.

5. Georgoulis AD, Pappa L, Moebius U, et al. The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc. 2001; 9:364–368.

6. Lee BI, Min KD, Choi HS, et al. Immunohistochemical study of mechanoreceptors in the tibial remnant of the ruptured anterior cruciate ligament in human knees. Knee Surg Sports Traumatol Arthrosc. 2009; 17:1095–1101.

7. Gohil S, Annear PO, Breidahl W. Anterior cruciate ligament reconstruction using autologous double hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascularisation. A randomised prospective study with a one-year follow-up. J Bone Joint Surg Br. 2007; 89:1165–1171.
8. Lee BI, Kwon SW, Kim JB, Choi HS, Min KD. Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy. 2008; 24:560–568.

9. Lee BI, Min KD, Choi HS, Kim JB, Kim ST. Arthroscopic anterior cruciate ligament reconstruction with the tibial-remnant preserving technique using a hamstring graft. Arthroscopy. 2006; 22:340.

10. Ahn JH, Lee YS, Ha HC. Anterior cruciate ligament reconstruction with preservation of remnant bundle using hamstring autograft: technical note. Arch Orthop Trauma Surg. 2009; 129:1011–1015.

11. Ahn JH, Wang JH, Lee YS, Kim JG, Kang JH, Koh KH. Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: clinical and magnetic resonance imaging results. Arthroscopy. 2011; 27:1079–1089.

12. Chun KC, Hwang JS, Kim KM, Kim DH, Chun CH. Comparison of clinical results and second-look arthroscopic findings of remnant preserving versus non-remnant preserving technique after anterior cruciate ligament reconstruction using achilles allograft. J Korean Orthop Assoc. 2013; 48:366–374.

13. Ahn GY, Nam IH, Moon GH, Lee YH, Choi SP, Yoo JY. The effect of a tibial remnant preservation technique on the synovialization of the graft tendon in anterior cruciate ligament reconstruction: based on the second look arthroscopic findings. J Korean Arthrosc Soc. 2013; 17:11–17.
14. Ochi M, Adachi N, Uchio Y, et al. A minimum 2-year followup after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009; 25:117–122.

15. Hong L, Li X, Zhang H, et al. Anterior cruciate ligament reconstruction with remnant preservation: a prospective, randomized controlled study. Am J Sports Med. 2012; 40:2747–2755.
16. Hu J, Qu J, Xu D, Zhang T, Zhou J, Lu H. Clinical outcomes of remnant preserving augmentation in anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014; 22:1976–1985.

17. Song GY, Zhang H, Zhang J, et al. The anterior cruciate ligament remnant: to leave it or not? Arthroscopy. 2013; 29:1253–1262.

18. Weiler A, Peters G, Mäurer J, Unterhauser FN, Südkamp NP. Biomechanical properties and vascularity of an anterior cruciate ligament graft can be predicted by contrast-enhanced magnetic resonance imaging. A two-year study in sheep. Am J Sports Med. 2001; 29:751–761.
19. Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I. The long-term followup of primary anterior cruciate ligament repair. Defining a rationale for augmentation. Am J Sports Med. 1991; 19:243–255.
20. Arnoczky SP. Blood supply to the anterior cruciate ligament and supporting structures. Orthop Clin North Am. 1985; 16:15–28.

21. Dunlap J, McCarthy JA, Joyce ME, Ogata K, Shively RA. Quantification of the perfusion of the anterior cruciate ligament and the effects of stress and injury to supporting structures. Am J Sports Med. 1989; 17:808–810.

22. Fulkerson JP, Berke A, Parthasarathy N. Collagen biosynthesis in rabbit intraarticular patellar tendon transplants. Am J Sports Med. 1990; 18:249–253.

23. Sun L, Wu B, Tian M, Liu B, Luo Y. Comparison of graft healing in anterior cruciate ligament reconstruction with and without a preserved remnant in rabbits. Knee. 2013; 20:537–544.

24. Wu B, Zhao Z, Li S, Sun L. Preservation of remnant attachment improves graft healing in a rabbit model of anterior cruciate ligament reconstruction. Arthroscopy. 2013; 29:1362–1371.

25. Xie GM, Huang Fu XQ, Zhao JZ. The effect of remnant preservation on patterns of gene expression in a rabbit model of anterior cruciate ligament reconstruction. J Surg Res. 2012; 176:510–516.

26. Pauzenberger L, Syré S, Schurz M. "Ligamentization" in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013; 29:1712–1721.

27. Muramatsu K, Hachiya Y, Izawa H. Serial evaluation of human anterior cruciate ligament grafts by contrast-enhanced magnetic resonance imaging: comparison of allografts and autografts. Arthroscopy. 2008; 24:1038–1044.

28. Janssen RP, Scheffler SU. Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014; 22:2102–2108.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download