Abstract
Purpose
The purpose of this study was to evaluate the effectiveness of bipolar hemiarthroplasty for unstable intertrochanteric fracture in patients over the age of 80 years.
Materials and Methods
Sixty-two patients (62 cases) who had unstable comminuted intertrochanteric fractures between January 2007 and February 2012 were evaluated. All patients were over 80 years old at the time of the diagnosis, and were followed-up for at least 12 months. Patients were divided into two groups: those who received cementless stems (group 1, n=32) and those who received cemented stems (group 2, n=30). Functional results including Harris hip score, thigh pain, Koval's ambulatory classification, postoperative mortality rate, operation time, and the amount of blood loss were evaluated.
Results
The operation time and the amount of blood loss were significantly lower in group 1 compared to group 2. The Harris hip score was 82.1±8.6 points for group 1 and 83.4±7.5 points for group 2 at the final follow-up. One patient with poor cement press-fit level in group 2 experienced thigh pain. Twenty-seven patients (84.4%) in group 1 and 25 patients (83.3%) in group 2 recovered pre-injury ambulatory status. During the follow-up period, overall, 6 patients (18.8%) in group 1 and 8 patients (26.7%) in group 2 died. No significant differences in follow-up mortality rates were observed between the two groups.
With today's aging population, musculoskeletal diseases such as osteoporosis, degenerative arthritis, and degenerative spine disease, are on the rise, and these conditions are associated with increased fracture risk. Intertrochanteric fractures in elderly patients often involve severe displacement or comminution with poor bone quality.1) Accordingly, various treatment methods for hip fracture have been introduced.
The incidence of fixation failure is reported to be as high as 20% in unstable intertrochanteric fracture due to nonunion, metal failure, and femoral perforation. Also postoperative ambulation may be delayed in this population due to the difficulty of achieving firm fixation.2) In addition, when fixation failure happens, reoperation may not be possible due to the patient's general condition and medical complications.34) In comparison, bipolar hemiarthroplasty is performed as an alternative to osteosynthesis in elderly patients with unstable fracture patterns regardless of bone quality, and early ambulation is possible if stable fixation is attained.5) In cases of poor bone quality, cemented fixation was used in the past to enhance the initial fixation strength.6) A cemented stem is advantageous for stable fixation, early weight bearing, and less thigh pain, but it increases the operation time and blood loss, and complications such as cardiovascular toxicity.78910) In the past, cementless fixation was not favored because it led to problems with initial fixation strength, bone ingrowth, subsidence of the stem and intraoperative periprosthetic fracture. However, with improvements in implant design, material, and insertion techniques, cementless fixation has gained popularity because it facilitates initial strength and late biological fixation.11)
Lim et al.12) reported excellent ambulatory recovery of femoral neck and intertrochanteric fractures after bipolar hemiarthroplasty in patients over 80 years old. However, the study for bipolar hemiarthroplasty for unstable intertrochanteric fracture in patients over 80-year-old is rare. In this study, we aimed to evaluate the clinical and radiological outcomes of cementless and cemented bipolar hemiarthroplasty for unstable intertrochanteric fractures in patients over 80-year-old.
Between January 2007 and February 2012, 62 patients over 80-year-old, who underwent bipolar hemiarthroplasty for unstable intertrochanteric femur fracture at our institution were included in this retrospective study. All patients had unstable fractures according to the Evans classification. Patients with pathologic fractures, previous contralateral hip fractures, stable fractures, osteoarthritis, or rheumatoid arthritis in the fractured hip, and nonfunctional ambulatory before injury were excluded in the study.
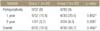
Thirty-two patients received cementless stems (group 1), and 30 patients received cemented stems (group 2). There were 12 men and 20 women in group 1, 10 men and 20 women in group 2. The mean age was 84.5±3.2 years in group 1 and 84.2±3.7 years in group 2. The mean T-score of femur neck bone mineral density was -3.7±0.3 in group 1 and -3.9±0.2 in group 2. Comorbidity scores were recorded before surgery by using the American Society of Anesthesiologists criteria (Table 1). Minimum follow-up was 12 months (mean, 24 months; range, 12-40 months).
Surgery was performed by the same surgeon in all cases. In both groups, the transgluteal approach (Hardinge approach) was used in the lateral position. The cementless stems used for group 1 were Summits Basic Press-fit Stem (Depuy, West Chester, PA, USA) in twenty cases and Bencox ID Stem (Corentec, Cheonan, Korea) in twelve cases. The cemented stems used for group 2 were Summits Basic Cemented Stem in twenty cases and Bencox ID Cemented Stem in ten cases. For stable reduction and fixation with cementless stems, proximal fixation of the implant was reinforced with additional wire fixation of the lesser trochanter and posteromedial area. To prevent deep vein thrombosis, compressive stockings were applied to both legs. Quadriceps femoris muscle strengthening exercises were begun one day after surgery. The postoperative rehabilitation using tilting table, parallel bar walking, and walker ambulation were performed depending on the patient's conditions, after removal of the drainage tube.
For the clinical assessment, length of hospital stay, operation time, blood loss during surgery, time until postoperative weight bearing ambulation, last follow-up Harris hip scores (90-100: excellent, 80-89: good, 70-79: fair, <70: poor) and thigh pain were assessed. Ambulatory ability were assessed according to the Koval's classification (grade I: independent community ambulator, grade II: community ambulator with cane, grade III: community ambulator with walker/crutches, grade IV: independent household ambulator, grade V: household ambulator with cane, grade VI: household ambulator with walker/crutches, grade VII: nonfuctional ambulator)13) showing best ambulatory status within 12 months after surgery compared to pre-fracture level considering elderly patients. Mortality rates of the groups in follow-up period were recorded and reported as perioperatively, 1-year and 2-year mortality rates. For the radiological assessment, anteroposterior and lateral radiographs of the hip were taken at 6 weeks and at 3, 6, 9, and 12 months after surgery, as well as every year thereafter.
Cementless stem stability was assessed in terms of bony ingrowth, stable fibrous fixation, and instability of the prosthesis according to the criteria of Engh et al.14) Femoral stem fixation was classified into press-fit and non-press-fit fixation. The degree of vertical subsidence of the femoral stem was measured by using the distance between the greater trochanter and the superolateral margin of the stem.
Radiolucent lines, bone resorption, endosteal new bone formation, and osteolysis were examined in the seven zones described by Gruen et al.15) Radiolucent line denoted the radiolucent area around the stem surrounded by radiodense lines, and it was considered to be present if it occupied 50% or more of any zone. Loosening of the femoral stem was defined as the appearance of a radiolucent line that was progressive or at least 1mm-thick in all zones, or the presence of continuous migration of the femoral stem.
The press-fit level of the cemented stem to the bone cement was evaluated according to Kelley's cement scoring system by using the radiological images obtained immediately after surgery.16)
Data are expressed as mean values with standard deviation. Differences in variables were compared across subgroups with a chi-square test for categorical variables and an independent t test for numeric variables as appropriate. For comparison change in walking ability between cementless and cemented groups, Wilcoxon signed rank sum test was employed. For comparison follow up mortality rate, chi-square test and Fisher's exact test were employed. All statistical analyses were carried out using IBM SPSS ver. 21.0 statistical software (IBM Co., Armonk, NY, USA). p-values less than 0.05 were considered as statistically significant.
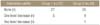
The mean hospital stay was 16.5±3.2 days for group 1 and 17.1±4.2 days for group 2. The mean operation time was 85.0±4.1 minutes for group 1 and 97.0±5.3 minutes for group 2. The mean blood loss was 395.0±40.2 ml for group 1 and 445.0±37.5 ml for group 2. Operation time and amount of blood loss were significantly lower in the cementless group compared to the cemented group (p<0.05). The mean time to weight bearing ambulation after surgery was five days for both groups. The mean Harris hip score at last follow-up was 82.1±8.6 points for group 1 and 83.4±7.5 points group 2. Better than fair results of Harris hip score were obtained in 29 patients (90.6%) for group 1 and 27 patients (90.0%) for group 2. None of patients in both group died perioperatively (Table 1). One patient with poor cement press-fit level in group 2 experienced thigh pain. The mean postoperative mortality rate within 1 year was 15.6% for group 1 and 20.0% for group 2. During the follow-up period, overall, 6 patients (18.8%) in group 1 and 8 patients (26.7%) in group 2 died. Regarding the follow-up mortality rates, there were no significant difference between the groups (Table 2). Twenty-seven patients (84.4%) in group 1 and 25 patients (83.3%) in group 2 recovered their preoperative ambulatory ability. Five patients (15.6%) in group 1 and 4 patients (13.3%) in group 2 showed a one-level decrease from their preoperative ambulatory ability. In group 2, 1 patient (3.3%) showed a two-level decrease; this patient had bed rest due to aggravation of underlying diseases. Overall, 52 of 62 patients (83.9%) regained their preoperative ambulatory ability within 12 months after surgery (Table 3, 4)
According to the radiological findings at last-follow-up, a press-fit was achieved for all patients in group 1. No cases of subsidence of femoral stem more than 5 mm were encountered (Fig. 1). There were no radiolucent lines around the femoral stem in any cases in group 1. Heterotopic ossification was observed in 1 patient (3.1%) in group 1. The postoperative cement press-fit level according to Kelly's cement scoring system was good in 29 patients and poor in only 1 patient (3.3%) (Table 5). Unfavorable result of poor cement filing was observed thigh pain. However, walker aided ambulation was possible after pain control with medication (Fig. 2).
Each group had one case of pneumonia, which were treated with admission to the intensive care unit and using antibiotics. No joint dislocation occurred during follow-up period, nor did symptomatic deep vein thrombosis, fat embolism, and pulmonary embolism. There were no intraoperative femoral fractures or deaths. Superficial infection occurred as a postoperative complication in 2 patients (6.3%) in group 1; the infection was cured with wire removal, curettage, and intravenous antibiotics administration.
The incidence of all hip fractures is approximately 80 per 100,000 persons and is expected to double over the next fifty years as the population ages.17) Anatomic reduction of the unstable intertrochanteric fractures in elderly patients with firm internal fixation is difficult to achieve and maintain; accordingly, malunion, reduction failure, and reoperation are common complications.18) Considering the importance of early postoperative ambulation and rehabilitation, bipolar hemiarthroplasty is considered one of the most effective primary treatment methods for unstable intertrochanteric fracture.192021) In 1958, Charnley22) was the first to use cement to achieve fixation in hip arthroplasty. However, particle induced osteolysis or implant loosening, known as cement disease were reported in the 1970s. Parvizi et al.10) found that elderly patients with preexisting cardiovascular conditions who underwent cemented arthroplasty were at increased risk for intraoperative death compared to patients who underwent elective hip arthroplasty.
Cemented fixation is advantageous for achieving initial implant stability and early rehabilitation in cases of unstable intertrochanteric fractures with poor bone quality. Haentjens et al.20) reported on 91 patients over the age of 75 whose unstable intertrochanteric or subtrochanteric fractures were treated with cemented bipolar hemiarthroplasty; they found good functional results in 78% of patients. In our study, cement filling was good in 96.7% of patients and ambulatory ability was good in 83.3% of patients.
The cementless stem can be used to prevent cement-related complications, but stem migration due to bone ingrowth failure, bone resorption, thigh pain, and stress shielding have been reported.1423) Archibeck et al.24) reported good long-term results in 86% of 78 cases, with improvements in stem design, stem components, and surgical techniques. In our study, stable fixation was observed in all cases in the cementless group at the last-follow-up, and patients showed excellent recovery of ambulatory ability (84.4%).
Taylor et al.25) reported better function and better mobility in the cemented group than in cementless group. In contrast, ambulatory ability recovery results of our study groups are similar (83.3% in cemented group, 84.4% in cementless group). For stable reduction of an unstable fragment, Jones26) suggested a method of screw fixation of the lesser trochanter fragment. In our study, additional wire fixation was performed in the posteromedial area, including the lesser trochanter area, for stable reduction and fixation.
It is important for elderly patients to recover their preoperative ambulatory ability. Early ambulation can prevent complications caused by long-term bed rest, such as pneumonia, bedsores, and poor general conditions. In our study, early ambulation was allowed when stable fixation was achieved after femoral stem insertion, as fast as possible considering the general condition of each patient. Overall, 52 patients (83.8%) regained their preoperative ambulatory ability.
Campbell et al.27) found that postoperative thigh pain in the cementless stem occurred in up to 22% of patients over two years and was caused by unstable femoral stems and biological fixation failure. In our study, no cases of thigh pain or reoperation due to stem subsidence or stem fixation failure in the cementless stem group were observed. It is considered to be due to the advanced stem design with primary mechanical stability and superior biological fixation. Because the posteromedial fragment provides essential resistance to axial loading and stem migration, stable reduction in the posteromedial area with wire fixation is important to reduce thigh pain for unstable intertrochanteric fracture. In our study, all patients had stable reduction of posteromedial fragment. Hossain and Andrew28) reported 1% risk of perioperative death after hip fracture surgery. Mortality rate at 1 year after surgery was reported as 17.2% to 27%.529) Our current study also supported the results reported in the literature (19% in cementless group and 27% in cemented group). However our results show no significant differences between the groups.
In our current comparative study, we found that cementless hemiarthroplasty had shorter surgical operation time and lesser blood loss compared to cemented hemiarthroplasty. Cementless hemiarthroplasty was thought to be helpful in preventing serious medical complications that are associated with elderly patients.
Both cemented and cementless hemiarthroplasty groups showed good functional results. The significance of our study is that it showed a comparable functional result between cemented and cementless groups. Mortality rates and complications did not increase in cementless group compared to cemented group.
The retrospective design, small sample size (62 cases) and the short follow-up period can be considered as limitations of our study. However, mid-to long term follow-up study are difficult due to their remaining life expectancy considering that patients are over 80-year-old.
Since many elderly patients are transferred to nursing homes after they are discharged from the hospital due to underlying diseases or lack of cooperation from family members, these patients may also need to be educated about compliance with follow-up instructions. It is necessary to analyze the mortality and complications in future multicenter studies.
Cementless bipolar hemiarthroplasty can be recommended for the treatment of unstable intertrochanteric fractures in patients over 80-year-old with early mobilization, satisfactory functional results, low rates of implant loosening, shorter surgery time, and lesser blood loss compared to cemented hemiarthroplasty.
Figures and Tables
 | Figure 1An 82-year-old woman with right hip pain. (A) Preoperative radiograph showing an unstable intertrochanteric fracture. (B) Cementless bipolar hemiarthroplasty was performed three days after the injury. Cerclage wire was used to fix the greater and lesser trochanters. (C) Postoperative 36-month follow-up radiograph showing no position change or subsidence of the stem; the patient had recovered her pre-injury ambulatory ability without complications. |
 | Figure 2An 85-year-old woman with left hip pain. (A) Preoperative radiograph showing an unstable intertrochanteric fracture. (B) Cemented bipolar hemiarthroplasty was performed four days after the injury. Bone-cement radiolucency was noted. (C) Postoperative 10-month follow-up radiography showing greater and lesser trochanter fragment displacement, but the patient was able to ambulate with a walker after pain control. |
Table 3
Koval's Ambulatory Ability* Results at 24 Months after Surgery

*Categories of ambulation according to Koval et al.13) 1): independent community ambulator, 2): community ambulator with cane, 3): community ambulator with walker or crutches, 4): independent household ambulator, 5): household ambulator with cane, 6): household ambulator with walker or crutches, 7): non-functional ambulator.
References
1. Choy WS, Ahn JH, Ko JH, Kam BS, Lee DH. Cementless bipolar hemiarthroplasty for unstable intertrochanteric fractures in elderly patients. Clin Orthop Surg. 2010; 2:221–226.

2. Baumgaertner MR, Chrostowski JH, Levy RN. Intertrochanteric hip fractures. In : Browner BD, Levine AM, Jupiter JB, Trafton PG, editors. Skeletal trauma. Vol. 2. Philadelphia: WB Saunders;1992. p. 1833–1881.
3. Bickel WH, Jackson AE. Intertrochanteric fractures of the femur; an analysis of the end results of 126 fractures treated by various methods. Surg Gynecol Obstet. 1950; 91:14–24.
4. Cobelli NJ, Sadler AH. Ender rod versus compression screw fixation of hip fractures. Clin Orthop Relat Res. 1985; 201:123–129.

5. Kim Y, Moon JK, Hwang KT, Choi IY, Kim YH. Cementless bipolar hemiarthroplasty for unstable intertrochanteric fractures in octogenarians. Acta Orthop Traumatol Turc. 2014; 48:424–430.

6. Brander VA, Malhotra S, Jet J, Heinemann AW, Stulberg SD. Outcome of hip and knee arthroplasty in persons aged 80 years and older. Clin Orthop Relat Res. 1997; 345:67–78.

7. Ahnfelt L, Herberts P, Malchau H, Andersson GB. Prognosis of total hip replacement. A Swedish multicenter study of 4,664 revisions. Acta Orthop Scand Suppl. 1990; 238:1–26.
8. Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am. 1985; 67:1074–1085.

9. Parker MJ. The management of intracapsular fractures of the proximal femur. J Bone Joint Surg Br. 2000; 82:937–941.

10. Parvizi J, Holiday AD, Ereth MH, Lewallen DG. The Frank Stinchfield Award. Sudden death during primary hip arthroplasty. Clin Orthop Relat Res. 1999; 369:39–48.
11. Hungerford DS, Jones LC. The rationale for cementless total hip replacement. Orthop Clin North Am. 1993; 24:617–626.

12. Lim CH, Chung YY, Kim JS, Kim CY. Hemiarthroplasty for hip fractures in elderly patients over 80 years old: comparative analysis between femoral neck fracture and intertrochanteric fracture. Hip Pelvis. 2013; 25:44–50.
13. Koval KJ, Aharonoff GB, Rosenberg AD, Bernstein RL, Zuckerman JD. Functional outcome after hip fracture. Effect of general versus regional anesthesia. Clin Orthop Relat Res. 1998; 348:37–41.
14. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990; 257:107–128.

15. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; 141:17–27.
16. Kelly AJ, Lee MB, Wong NS, Smith EJ, Learmonth ID. Poor reproducibility in radiographic grading of femoral cementing technique in total hip arthroplasty. J Arthroplasty. 1996; 11:525–528.

18. Kang SY, Lee EW, Kang KS, et al. Mode of fixation failures of dynamic hip screw with tsp in the treatment of unstable proximal femur fracture: biomechanical analysis and a report of 3 cases. J Korean Orthop Assoc. 2006; 41:176–180.

19. Stern MB, Angerman A. Comminuted intertrochanteric fractures treated with a Leinbach prosthesis. Clin Orthop Relat Res. 1987; 218:75–80.

20. Haentjens P, Casteleyn PP, Opdecam P. Primary bipolar arthroplasty or total hip arthroplasty for the treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Acta Orthop Belg. 1994; 60:Suppl 1. 124–128.
21. Ereth MH, Weber JG, Abel MD, et al. Cemented versus noncemented total hip arthroplasty: embolism, hemodynamics, and intrapulmonary shunting. Mayo Clin Proc. 1992; 67:1066–1074.
22. Charnley J. Long-term results of low-friction arthroplasty. Hip. 1982; 42–49.
23. Kawamura H, Dunbar MJ, Murray P, Bourne RB, Rorabeck CH. The porous coated anatomic total hip replacement A ten to fourteen-year follow-up study of a cementless total hip arthroplasty. J Bone Joint Surg Am. 2001; 83:1333–1338.
24. Archibeck MJ, Berger RA, Jacobs JJ, et al. Second-generation cementless total hip arthroplasty Eight to eleven-year results. J Bone Joint Surg Am. 2001; 83:1666–1673.
25. Taylor F, Wright M, Zhu M. Hemiarthroplasty of the hip with and without cement: a randomized clinical trial. J Bone Joint Surg Am. 2012; 94:577–583.

26. Jones JB. Screw fixation of the lesser trochanteric fragment. Clin Orthop Relat Res. 1977; 123:107.

27. Campbell AC, Rorabeck CH, Bourne RB, Chess D, Nott L. Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. J Bone Joint Surg Br. 1992; 74:63–66.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download