Abstract
Purpose
The purpose of this study is to evaluate risk factors for wrist stiffness after treatment of distal radius fractures.
Materials and Methods
A total of 55 consecutive patients who were diagnosed with distal radius fracture at the current authors' institution and followed-up for at least 6 months were included in this retrospective study. Data on all factors related to wrist stiffness were considered. The degree of association for each of the factors was determined by calculation of the odds ratio (OR), with a 95% confidence interval. Logistic regression analyses were performed. p-value was set below 0.05.
Results
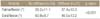
Among radiologic indexes reflecting the degrees of fracture reduction, only ulnar variance showed significant association with wrist stiffness of distal radius fracture (p<0.05). In univariate analysis, age (p=0.037; OR, 1.051) and diabetes mellitus (DM) (p=0.016; OR, 8.000) showed significant association with wrist stiffness. Various factors significant at the p-value less than 0.20 level in univariate analyses were included in the multivariate analyses. In multivariate analyses, only DM (p=0.034; OR, 6.588) showed significant association with wrist stiffness.
Figures and Tables
References
1. Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles', or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989; 149:2445–2448.

2. Hagino H, Yamamoto K, Ohshiro H, Nakamura T, Kishimoto H, Nose T. Changing incidence of hip, distal radius, and proximal humerus fractures in Tottori Prefecture, Japan. Bone. 1999; 24:265–270.

3. Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006; 88:1944–1951.

4. Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007; 21:316–322.

5. Soong M, van Leerdam R, Guitton TG, Got C, Katarincic J, Ring D. Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg Am. 2011; 36:3–9.

6. Lucado AM, Li Z. Static progressive splinting to improve wrist stiffness after distal radius fracture: a prospective, case series study. Physiother Theory Pract. 2009; 25:297–309.

7. Ahn JY, Han JS, Min KS. Experimental study for defining range of motion required for daily activities in wrist joint. J Korean Orthop Assoc. 2000; 35:797–802.

8. Tsukazaki T, Takagi K, Iwasaki K. Poor correlation between functional results and radiographic findings in Colles' fracture. J Hand Surg Br. 1993; 18:588–591.

9. Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000; 25:19–28.

10. Chung KC, Squitieri L, Kim HM. Comparative outcomes study using the volar locking plating system for distal radius fractures in both young adults and adults older than 60 years. J Hand Surg Am. 2008; 33:809–819.

11. Jupiter JB, Marent-Huber M. LCP Study Group. Operative management of distal radial fractures with 2.4-millimeter locking plates. A multicenter prospective case series. J Bone Joint Surg Am. 2009; 91:55–65.

12. Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011; 93:2146–2153.

13. Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010; 92:1851–1857.

14. Lutz K, Yeoh KM, MacDermid JC, Symonette C, Grewal R. Complications associated with operative versus nonsurgical treatment of distal radius fractures in patients aged 65 years and older. J Hand Surg Am. 2014; 39:1280–1286.

15. McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br. 1988; 70:649–651.

16. Chen NC, Jupiter JB. Management of distal radial fractures. J Bone Joint Surg Am. 2007; 89:2051–2062.

18. Trumble TE, Wagner W, Hanel DP, Vedder NB, Gilbert M. Intrafocal (Kapandji) pinning of distal radius fractures with and without external fixation. J Hand Surg Am. 1998; 23:381–394.

19. Tang JB, Ryu J, Kish V, Wearden S. Effect of radial shortening on muscle length and moment arms of the wrist flexors and extensors. J Orthop Res. 1997; 15:324–330.

20. Karnezis IA, Panagiotopoulos E, Tyllianakis M, Megas P, Lambiris E. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005; 36:1435–1439.

21. Barton T, Chambers C, Bannister G. A comparison between subjective outcome score and moderate radial shortening following a fractured distal radius in patients of mean age 69 years. J Hand Surg Eur Vol. 2007; 32:165–169.

22. Adams BD. Effects of radial deformity on distal radioulnar joint mechanics. J Hand Surg Am. 1993; 18:492–498.

23. Hirahara H, Neale PG, Lin YT, Cooney WP, An KN. Kinematic and torque-related effects of dorsally angulated distal radius fractures and the distal radial ulnar joint. J Hand Surg Am. 2003; 28:614–621.

24. Nishiwaki M, Nakamura T, Nagura T, Toyama Y, Ikegami H. Ulnar-shortening effect on distal radioulnar joint pressure: a biomechanical study. J Hand Surg Am. 2008; 33:198–205.

25. Hollevoet N, Verdonk R. The functional importance of malunion in distal radius fractures. Acta Orthop Belg. 2003; 69:239–245.
26. Ljungqvist O, Nygren J, Thorell A. Insulin resistance and elective surgery. Surgery. 2000; 128:757–760.

27. Gamstedt A, Holm-Glad J, Ohlson CG, Sundström M. Hand abnormalities are strongly associated with the duration of diabetes mellitus. J Intern Med. 1993; 234:189–193.

28. Rosenbloom AL, Silverstein JH, Lezotte DC, Richardson K, McCallum M. Limited joint mobility in childhood diabetes mellitus indicates increased risk for microvascular disease. N Engl J Med. 1981; 305:191–194.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download