Abstract
As the expertise of the surgeon improves in arthroscopic surgery of the hip, the number of conditions treated by it also increases. In this case, an arthroscopic treatment was performed on a patient with piriformis syndrome due to schwannoma on the sciatic nerve. Meticulous excision of the cystic lesion on the sciatic nerve was completely performed and neither recurrence nor complication of the surgery was observed. Endoscopic excision using arthroscopy is useful for reducing postoperative pain and achieving early return to activities for the patient.
Piriformis syndrome is the most common cause of persistent sciatica in patients for whom a proper diagnosis was not established and for whom the routine spine-centered approach for treatment failed. Primary piriformis syndrome is for all intrinsic piriformis muscle problems itself.12) Secondary piriformis syndrome includes all other etiologies and other conditions impinging the sciatic nerve.3)
Hip arthroscopy is now becoming increasingly used for surgery to the structures surrounding the hip, not just those within the cavity of the hip.4) Recently, arthroscopy of the hip has been on the rise as a treatment of extra-articular hip disease including piriformis syndrome.
In this case, we report a case of patient with schwannoma on the sciatic nerve, which was treated through endoscopic excision using arthroscopy.
A 53-year-old man presented to our clinic with intermittent radiating pain to the left lower extremity for duration of 2 years. The pain has aggravated for 2 months, which is from left posterior hip and radiating to medial thigh with pricking nature at night. He had a history of mitral valve replacement for mitral valve stenosis and several operations for neurilemmoma related to neurofibromatosis type 2 in multiple sites, such as, buttock, thigh, flank area, brain and spinal cord for about 10 years. He complained of tenderness on the sciatic notch area. Physical examination showed that there were no limitation on range of motion of the left hip joint and freiberg sign. Pace sign and impingement sign were positive. Patrick test was negative. Neurological examination revealed hypesthesia on L5 to S1 sensory area in the left lower leg.
The laboratory findings showed no abnormality.
Whole spine T2-weighted sagittal magnetic resonance imaging (MRI) and lumbar and sacrum MRI with enhancement revealed multiple intradural mass on lower thoracic and lumbar spine and small enhanced lesions on left quadratus lumborum muscle and psoas muscle (Fig. 1). MRI and magnetic resonance arthrography of the hip showed a well capsulized, regular margin and 2.5×1.8 cm sized mass, highly suggestive neurilemmoma originated from sciatic nerve between piriformis and gluteus maximus (Fig. 2). There was no anatomical abnormality or deformity of piriformis muscle itself.
We decided to perform an arthroscopic procedure. It was performed under spinal anesthesia with supine position on the hip endoscopic table. The patient was positioned supine with 15 degree tilting upward on the hip endoscopic table. Exploration of the sciatic nerve was carried out through the anterolateral and posterolateral and/or axillary portals. The anterolateral portal was placed about 1 cm anterior and 1 cm superior to the greater trochanter (GT) on 60° internal rotation of lower extremity. The posterolateral portal was placed 5 cm posterior to the GT and in line with the anterolateral portal. The axillary portal was placed 3 cm superior or inferior to center between anterolateral and posterolateral portals (Fig. 3), which allowed for better visualization of sciatic nerve up to the sciatic notch. Through the endoscopy, sciatic nerve may be detected, that passes around piriformis, obturator internus and gemelli muscles in deep gluteal space.
The mass was located in the fibrous sheath of the sciatic nerve and adhered to epineural vessel and the branch of the inferior gluteal artery. Using a blunt probe, the sciatic nerve and vascular scar bands were inspected thoroughly. The epineural blood vessels were dissected from the mass carefully and ligated with absorbable vascular clip. The fibrous sheath of the mass was incised with arthroscopic scissors and nerve retractor was used to delineateh et base of the mass from the sciatic nerve sheath. The mass on the sciatic nerve was enucleated from the sheath by delicate dissection (Fig. 4) and small vascular branches were coagulated with arthroscopic electocautery. After the mass was free from the nerve, we held it using arthroscopic grasper to prevent loss by fluid circulation. Additional portal was made to facilitate extraction of relatively large mass. The mass was removed using laparoscopic storage bag without cutting. And the tissue was sent for histological examination (Fig. 5). Arthroscopic inspection was performed again from sciatic notch to ischial tuberosity to confirm complete removal and suction drain was inserted.
For 1 day postoperatively, suction drain was kept in deep gluteal space to prevent hematoma that may cause sciatic nerve palsy.
The histological examination of the mass confirmed neurilemoma (Fig. 6). After the operation, the pain disappeared at once. The patient was discharged after postoperative wound care and went back to normal life within 3 days after the surgery. We had 13 months of follow-up after the surgery and neither recurrence nor complication of the surgery were observed.
Treatment options for lower back pain and sciatica related to piriformis syndrome include the more conservative option of physical therapy, the use of anti-inflammatory agents, injections of local anesthetics and corticosteroids, and the more recently studied option of botulinum neurotoxin injections.5) The surgical technique can be performed in patients who did not respond to these conservative therapy. As open surgical approach of piriformis syndrome, piriformis dissection on insertion site and sciatic nerve detachment was widely performed.6) Open surgical approach involves the disconnection and resection of the piriformis muscle, and can cause adhesion and scar formation. These adhesion and scar formation can cause recurrent pain.
Dezawa et al.7) performed arthroscopic technique for piriformis syndrome in 6 patients and achieved good results in all. Arthsrcoopic decompression of piriformis syndrome on the sciatic nerve decreases the soft tissue injury and secondary scar formation by making smaller skin incision and appears useful in improving function and diminishing pain in sciatic nerve entrapment.
Benign schwannoma is the most common tumor of peripheral nerves and malignant transformation is extremely rare. Although most peripheral schwannomas can be resected with minimal to no postoperative neurological deficits, the surgeon must anticipate and discuss with the patient that, besides the usual surgical complications, new neurological deficits could develop.8) In the majority of cases, even when the tumor is carefully dissected from the involved nerve, incomplete nerve palsies sometimes occur. Levi et al.9) reported an 25.3% incidence of postoperative neurologic deficits in patients who had previously undergone schwannoma excision.
But, Hwang et al.10) a patient with perineural cyst on sciatic nerve complaining of the symptoms of piriformis syndrome, which was treated through arthroscopic cyst incision and decompression without neurologic deficits. Even in arthroscopy, experienced surgeons have demonstrated that peripheral nerve sheath tumor can be resected completely and safely from major peripheral nerves. Endoscopic excision using arthroscopy is useful for reducing postoperative pain and achieving early return to activities for the patient.
Figures and Tables
Figure 1
(A) Whole spine T2-weighted sagittal magnetic resonance imaging (MRI) shows multiple intradural masses on lower thoracic and lumbar spine. (B) Lumbar and sacrum MRI with enhancement reveal small enhancing lesions on the left quadratus lumborum muscle and psoas muscle.
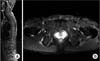
Figure 2
T2-weighted hip magnetic resonance imaging. (A) In axial view, image showed a well capsulized, regular margin and a 2.5×1.8 cm sized mass. It showed low signal intensity in the central lesion, and high signal intensity in the peripheral lesion. (B) In coronal view, neurilemmoma originated from the sciatic nerve between piriformis and gluteus maximus. The mass was highly estimated to be a neurilemmoma.
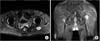
Figure 3
The anterolateral portal is placed approximately 1 cm anterior and 1 cm superior to the greater trochanter (GT) on 60° internal rotation of lower extremity ①. The posterolateral portal is placed 5 cm posterior to the GT and in line with the anterolateral portal ②.

Figure 4
(A) The huge mass was located in the fibrous sheath of the sciatic nerve and adhered to the epineural vessel and the branch of the inferior gluteal artery. (B) The vessels were carefully dissected from the mass and ligated with an absorbable vascular clip. (C) The fibrous sheath was incised and the mass was excised from the sciatic nerve.

References
1. Benzon HT, Katz JA, Benzon HA, Iqbal MS. Piriformis syndrome: anatomic considerations, a new injection technique, and a review of the literature. Anesthesiology. 2003; 98:1442–1448.
2. Parziale JR, Hudgins TH, Fishman LM. The piriformis syndrome. Am J Orthop (Belle Mead NJ). 1996; 25:819–823.
3. Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin North Am. 2004; 35:65–71.
4. Reich MS, Shannon C, Tsai E, Salata MJ. Hip arthroscopy for extra-articular hip disease. Curr Rev Musculoskelet Med. 2013; 6:250–257.
5. Cassidy L, Walters A, Bubb K, Shoja MM, Tubbs RS, Loukas M. Piriformis syndrome: implications of anatomical variations, diagnostic techniques, and treatment options. Surg Radiol Anat. 2012; 34:479–486.
6. Foster MR. Piriformis syndrome. Orthopedics. 2002; 25:821–825.
7. Dezawa A, Kusano S, Miki H. Arthroscopic release of the piriformis muscle under local anesthesia for piriformis syndrome. Arthroscopy. 2003; 19:554–557.
8. Siqueira MG, Socolovsky M, Martins RS, et al. Surgical treatment of typical peripheral schwannomas: the risk of new postoperative deficits. Acta Neurochir (Wien). 2013; 155:1745–1749.
9. Levi AD, Ross AL, Cuartas E, Qadir R, Temple HT. The surgical management of symptomatic peripheral nerve sheath tumors. Neurosurgery. 2010; 66:833–840.
10. Hwang DS, Kang C, Lee JB, Cha SM, Yeon KW. Arthroscopic treatment of piriformis syndrome by perineural cyst on the sciatic nerve: a case report. Knee Surg Sports Traumatol Arthrosc. 2010; 18:681–684.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download