Abstract
Intramedullary nailing is considered the most biomechanically advantageous therapeutic modality in the treatment of subtrochanteric femoral fractures. Many technical pitfalls and difficulties in nailing are well known. Reduction of the proximal fragment in a flexed, abducted, and externally rotated position should be performed before nailing of subtrochanteric fractures in order to avoid malalignment and nonunion. In this review, various reduction techniques to control the proximal fragment which are useful in nailing will be discussed.
Figures and Tables
 | Figure 1Koch's diagram showing the magnitude of the compressive stresses medially and the tensile stresses laterally. |
 | Figure 2(A) Unique configuration of alendronate-associated subtrochanteric fractures: transverse or slight obliquity; minimal comminution; and lateral cortical thickening with splaying of cortices suggesting a pre-existing structural abnormality. (B) Ellipsoid thickening in the lateral cortex of the subtrochanteric femur (arrow) preceded fracture in patients on long-term alendronate. |
 | Figure 3Russell-Taylor classification of subtrochanteric fractures. Note the emphasis on lesser trochanteric integrity and piriformis fossa extension. |
 | Figure 4Seinsheimer classification of subtrochanteric fractures. Note the emphasis on fracture obliquity, comminution, and proximal extension. |
 | Figure 6The illustration depicts the subtrochanteric region of the femur (between double arrows), most commonly demarcated by the lesser trochanter as its superior margin and 5-cm distal as its inferior margin. m., muscle. |
 | Figure 7The typical deforming muscular forces cause the proximal fragment to be flexed by the iliopsoas, externally rotated by the short rotators, and abducted by the abductors. The femoral shaft is shortened and adducted by the adductors and quadriceps. |
 | Figure 9Malreduction after unsuccessful nailing of a subtrochanteric fracture. Flexion, abduction, and external rotation of the proximal fragment was not reduced at all. |
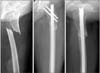
 | Figure 10(A) Initial X-ray shows a segmental fracture (AO-OTA 32B) with subtrochanteric involvement. (B) Postoperative X-ray after open wiring and nailing. (C, D) X-ray taken 3 months after operation shows nonunion (arrow). |
 | Figure 11(A) Satisfactory alignment was achieved postoperatively. (B) Follow-up radiograph after 7 months showed solid union of the fracture. |
 | Figure 13Intraoperative images show use of a Steinmann pin as a joystick to control the external rotation of the proximal fragment. |
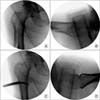
 | Figure 14(A, B) Intraoperative lateral images show that malalignment persists even after nail passed mainly due to the wire medullary canal at the proximal fragment. (C, D) The blocking pin (arrows) neutralizes the deforming force and in turn the deformity was corrected as the nail passed. |
 | Figure 15(A, B) Intraoperative anteroposterior (AP) and lateral images of an insufficiency fracture. (C, D) Joystick inserted from the lateral side does not neutralize the deforming force. (E, F) The calcar joystick neutralizes the external rotation on AP view but flexion force on lateral view is not ideally controlled. |
 | Figure 16(A, B) Failed attempt of reduction using the intramedullary joystick technique due to a wide medullary canal at the proximal fragment. (C, D) restoration of alignment with a bone hook placed percutaneously through a 2 cm incision (arrow). |
 | Figure 17(A, B) Intraoperative traction views show a simple spiral subtrochanteric fracture. (C, D) Near anatomical reduction was achieved by minimally invasive direct reduction of the fracture. |
 | Figure 18(A, B) Intraoperative traction views show a long oblique fracture involving the subtrochanteric area. (C, D) Near anatomical reduction was achieved by percutaneous direct reduction with reduction forcep and compression by forcep of the fracture. |
 | Figure 19(A) Intraoperative compression view by forcep at inferior incision. (B) The picuture shows compression at mid line incision makes more rotational error than inferior incision. White and black arrow indicate greater and lesser trochanter rotation. |
 | Figure 20(A, B) The entry point could be reached without problems in two-thirds of the specimens. (C, D) The entry point is often covered by parts of the greater trochanteric one-third of the specimens. |
 | Figure 21(A) An illustration shows 5 degrees of proximal bending in a cephalomedullary nail. (B) Intraoperative anteroposterior image shows that the angle between the entry portal and the axis of the medullary canal is much larger (18°) than proximal bending (5°) of a nail used. (C) As the proximal part of the nail passes the nail pushes the head fragment into varus, resulting in primary reduction loss. (D) Entry was corrected using a cannulated cutter. Now the angle between the entry portal and the axis of the proximal femur has decreased. (E) Compared to C, varus, tilt and the resulting gap on the lateral cortex was reduced. |
References
1. Kim JW, Oh CW, Byun YS, et al. A biomechanical analysis of locking plate fixation with minimally invasive plate osteosynthesis in a subtrochanteric fracture model. J Trauma. 2011; 70:E19–E23.

2. Tencer AF, Johnson KD, Johnston DW, Gill K. A biomechanical comparison of various methods of stabilization of subtrochanteric fractures of the femur. J Orthop Res. 1984; 2:297–305.

3. Wiss DA, Brien WW. Subtrochanteric fractures of the femur. Results of treatment by interlocking nailing. Clin Orthop Relat Res. 1992; 283:231–236.

4. Yoon YC, Jha A, Oh CW, et al. The pointed clamp reduction technique for spiral subtrochanteric fractures: a technical note. Injury. 2014; 45:1000–1005.

5. Abrahamsen B, Eiken P, Eastell R. Subtrochanteric and diaphyseal femur fractures in patients treated with alendronate: a register-based national cohort study. J Bone Miner Res. 2009; 24:1095–1102.

6. Black DM, Kelly MP, Genant HK, et al. Fracture Intervention Trial Steering Committee. HORIZON Pivotal Fracture Trial Steering Committee. Bisphosphonates and fractures of the subtrochanteric or diaphyseal femur. N Engl J Med. 2010; 362:1761–1771.

7. Ricci WM, Bellabarba C, Lewis R, et al. Angular malalignment after intramedullary nailing of femoral shaft fractures. J Orthop Trauma. 2001; 15:90–95.

8. Velasco RU, Comfort TH. Analysis of treatment problems in subtraochanteric fractures of the femur. J Trauma. 1978; 18:513–523.
9. van Doorn R, Stapert JW. The long gamma nail in the treatment of 329 subtrochanteric fractures with major extension into the femoral shaft. Eur J Surg. 2000; 166:240–246.
10. Russell TA, Mir HR, Stoneback J, Cohen J, Downs B. Avoidance of malreduction of proximal femoral shaft fractures with the use of a minimally invasive nail insertion technique (MINIT). J Orthop Trauma. 2008; 22:391–398.

11. Park J, Yang KH. Correction of malalignment in proximal femoral nailing--Reduction technique of displaced proximal fragment. Injury. 2010; 41:634–638.

12. Reiter MJ, Bui-Mansfield LT, O'Brien SD, Tubb CC. Subtrochanteric femur fractures: review of the complete pathologic spectrum with emphasis on distinguishing imaging features. J Comput Assist Tomogr. 2015; 39:47–56.
13. Liu X, Zhu Y, Lu Y, Li F, Wu G, Jiang C. Locked posterior shoulder dislocation associated with isolated fractures of the lesser tuberosity: a clinical study of 22 cases with a minimum of 2-year follow-up. J Orthop Trauma. 2015; 29:271–275.
14. Celebi L, Can M, Muratli HH, Yagmurlu MF, Yuksel HY, Bicimoğlu A. Indirect reduction and biological internal fixation of comminuted subtrochanteric fractures of the femur. Injury. 2006; 37:740–750.

15. Kennedy MT, Mitra A, Hierlihy TG, Harty JA, Reidy D, Dolan M. Subtrochanteric hip fractures treated with cerclage cables and long cephalomedullary nails: a review of 17 consecutive cases over 2 years. Injury. 2011; 42:1317–1321.

16. Grechenig W, Pichler W, Clement H, Tesch NP, Grechenig S. Anatomy of the greater femoral trochanter: clinical importance for intramedullary femoral nailing. Anatomic study of 100 cadaver specimens. Acta Orthop. 2006; 77:899–901.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download