Abstract
We report on an unusual case with infiltrating extradural spinal angiolipoma. Most spinal angiolipomas involve the thoracic spine and infiltrating ones are also located mainly at the thoracic levels rather than lumbar lesion. In particular, there are few cases of lumbar extradural infiltrating type spinal angiolipoma. One case is that of a 52-year-old female with infiltrating extradural spinal angiolipoma involving lumbar 4 (L4) vertebra, who underwent a L4-5 laminectomy and surgical removal of the tumor. We achieved satisfactory results with surgical treatment of the patient. Spinal angiolipoma has a benign course with a good postoperative outcome.
Spinal angiolipomas are benign tumors composed of both mature adipose and abnormal vascular elements that represent a distinct clinical and pathological entity.1) They are very rare, estimated to account for between 0.04% and 1.2% of all spinal axis tumors and 2% to 3% of extradural spinal tumors.1,2) The first report of spinal angiolipoma was found in a 16-year-old boy with an unsuccessfully treated spinal thoracic mass which was confirmed at autopsy in 1890. In 1901, Liebscher was the first to describe a spinal angiolipoma.3)
Angiolipomas can be further categorized into two sub-types: noninfiltrating and infiltrating. The noninfiltrating type is more common, usually well encapsulated, typically involves the subcutaneous tissues and usually seen in young adults, present clinically as painful nodules.4) The infiltrating ones are rare, and partially or entirely unencapsulated, ill-defined, infiltrate the surrounding tissues, especially the bone and usually involve the extremities.3,5)
Mostly previous reports were about angiolipomas involving the thoracic spine or noninfiltratig type rather than lumbar lesion or infiltrating type.6,7)
We report an unusual case with lumbar extradural infiltrating type spinal angiolipoma.
A 52-year-old female patient was admitted to a hospital with severe low back pain radiating to right lower extremity that had developed for several months. She had previous history of comedocarcinoma in situ on right breast and chronic renal failure. Breast cancer had been treated with modified radical mastectomy. Physical examination revealed weakness on the right hamstrings and tibialis anterior and right extensor hallucis longus and a negative straight leg raise on both side. The remainder of the lower extremity myotomes revealed grade 5 in strength. She was diminished sensation to light touch from the knee down her ankle in a lumbar 4 (L4) dermatomal pattern. The patient underwent simple radiograph, magnetic resonance imaging (MRI) and computed tomography (CT) scan examination on the lumbar area at a hospital. Simple radiograph showed a radiolucent lesion in posterior one third of L4 vertebral body (Fig. 1). MRI and CT scan showed a 2.65 cm sized, well-defined fatty mass in the right anterior epidural space at L4 with bony erosion of posterior body, but cortex was intact. The lesion was hyperintense on T1-weighted and hypointense on T2-weighted images (Fig. 2) and homogenous enhancement on T1-weighted image with gadolinium (Fig. 3). Tc99m-HDP 20 mCi was administrated intravenously, and then 3 hours later scan was obtained. But bone scan reveals no definite evidence of abnormal radiotracer uptake in the entire bony structures.
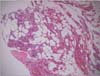
L4-5 laminectomy was perfomed. We identified the tumor which was a yellow-gray, soft-to-firm tissue in epidural area and easily dissected from the dura and then excision of tumor was performed with Kerrison and pituitary rongeur (Fig. 4). No residual tumor was identified caudal and rostal to the removed fatty tumor with mild bleeding. The patient underwent posterior instrumentation with 4 pedicle screws with autogenous bone graft considering invasion to body of L4 and presence of associated neurologic deficit. Nonsteroidal anti-inflammatory drugs, which influence blood coagulation and renal function, were not administered after surgery. A postoperative neurological changes were not detected. Three days after surgery, the patient was encouraged to ambulation with corset brace, and could walk without difficulty. Microscopic finding (H&E, ×200) showed varyng sized vessels and mature adipose tissue (Fig 5). There is no evidence of encapsulation, although some tendency to lobulation may be encountered. The blood vessels may predominate in some areas to the exclusion of fat. Six months after surgery, a recovery of neurological function was noted. At 24 months after surgery, there has been complete resolution of the pain and sensory symptoms in the lower extremities. The patient was clinically and radiologically disease free at the 24-month follow-up visit.
Angiolipomas are benign tumors of mature adipose tissue containing abnormal vascular elements. Spinal angiolipomas may be subdiviedd into two types. The commonest form is usually confined to the posterior epidural space. The other less common variety of spinal angiolipomas is termed 'infiltrating' in the literature since it invades bone. These tumors typically reside anterior or anterolateral to the spinal cord.6,8)
Histologically, a nonencapsulated (rarely partially encapsulated) tumor composed of mature lipocytes with delicate proliferating blood vessels wedging haphazardly into the surrounding tissue is seen.4) The blood channels range from capillary, to sinusoidal and venular, to arterial in size with irregularly thickened walls. Tumors with an abundance of smooth muscle proliferation are further subclassified as angiomyolipomas. Vessels may lack a definitive adventitia, with smooth muscle cells merging into the surrounding adipose tissue.2) The only difference between infiltrating and noninfiltrating types is that infiltrating angiolipoma is nonencapsulated.4)
Others have considered the tumor to be a congenital malformation or a benign hamartoma. Hemangiomas and lipomas may represent a spectrum within which angiolipomas constitute an intermediate entity. The more invasive infiltrating type of spinal angiolipoma would then represent a shift towards the hemangioma end of the spectrum. Whereas noninfiltrating spinal angiolipoma has a female preponderance,9) the infiltrating type is seen equally in male and female patients. Hormonal influence on the development, maintenance or progression of spinal noninfiltrating angiolipomas is theorized to account for the female preponderance.3) Spinal angiolipomas predominate among the 40- to 60-year age group.9) In the infiltrating tumor group, the age of patients ranged from 17 to 81 years, and the mean age was 50.5 year
Most spinal angiolipomas involve the thoracic spine with 53% of cases involving the midthoracic (T6-T9) region.2) The reason for this is unknown and is out of proportion to the relative length of each vertebral segment. Almost all noninfiltrating epidural angiolipomas are posterior or posterolateral in location, with four exceptions reported.3) Infiltrating angiolipomas are almost always anterior or anterolateral in position with two rare cases.2,3) Of a total of 98 spinal extradural angiolipoma cases, 18 including the one presented here have infiltrating type tumors.5) These tumors are generally located in the thoracic levels an anterior or anterolateral parts of extradural space.
Spinal angiolipomas are typically hyperintense on noncontrast T1-weighted images owing to their fatty content. Although they do not typically contain vascular flow voids on magnetic resonance images because of their low vascular flow characteristics, the degree of central hypointensity on T1-weighted images is predictive of the degree of vascularity.6) Most spinal angiolipomas enhance and fat suppression magnetic resonance in conjunction with contrast administration better defines the borders of the tumor and aids in surgical planning. In this presentation, the plain film and CT scans showed the scalloping erosion of the posterior portion at the vertebra body. There was no evidence of abnormal bony structures like as hemangioma with trabeculation of the affecting vertebral boyd. In the MRI of our case, the usual nature of the angiolipoma was suggested by the homogeneously hypointense extradural components on T1-weighted images
The first choice of treatment is total removal, but if total excision endangers life or impairs the functional acivities, cord decompression must be performed. Adjuvant radiotherapy is not recommende for patients with these benign pathological entities, since the prognosis, even with subtotal resection, is excellent.8,10) However, most patients have a good prognosis even with subtotal removal, because the tumors are usually slow growing and do not undergo malignant transformation.5) Recurrence is rare in spinal angiolipomas. In the cases with infiltrating tumor treated with subtotal resection, there are no recurrences after an average 37.6 months (2-114 months) follow-up.
In conclusion, an angiolipoma is uncommon at lumbar spine infiltratively. We took an operative resection of infiltrating lumbar spinal angiolipoma. We had a satisfactory result. There was no evidence of recurrence and the recovery of neurologic deficit was good. We had an unsual experience about spinal angiolipoma. So it needs a consideration that spinal angiolipoma sometimes can occur at lumbar spine.
Figures and Tables
 | Figure 1Preoperative plain radiograph shows a radiolucent lesion in lumbar 4 vertebral body (arrow). |
 | Figure 2Computed tomography (CT) scan and magnetic resonance imaging show a well-defined fatty mass at lumbar 4 (L4) vertebral body with bony erosion. (A) CT scan showing bony erosion of the right posterior L4 vertebral body. (B) T-1 weighted sagittal and axial images showing a hyperintense fatty mass in the right anterior epidural space. (C) T-2 weighted sagittal and axial images showing hypointense fatty mass in the right anterior epidural space. |
 | Figure 3T-1 weighted sagittal and axial images with gadolinium showing a hyperintense fatty mass in the right anterior epidural space. |
References
1. Ehni G, Love JG. Intraspinal Lipomas
Report of cases; Review of the literature, and clinical and pathologic study. Arch Neurol Psychiatry. 1945; 53:1–28.
2. Preul MC, Leblanc R, Tampieri D, Robitaille Y, Pokrupa R. Spinal angiolipomas. Report of three cases. J Neurosurg. 1993; 78:280–286.
3. Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer. 1974; 34:720–727.
4. Fourney DR, Tong KA, Macaulay RJ, Griebel RW. Spinal angiolipoma. Can J Neurol Sci. 2001; 28:82–88.

5. Leu NH, Chen CY, Shy CG, et al. MR imaging of an infiltrating spinal epidural angiolipoma. AJNR Am J Neuroradiol. 2003; 24:1008–1011.
6. Shin BJ, Kim KJ, Suh YS, Kim DW. Epidural angiolipoma: a case report. J Korean Soc Spine Surg. 1997; 4:165–169.
7. Park JH, Jeon SR, Rhim SC, Roh SW. Lumbar spinal extradural angiolipoma: case report and review of the literature. J Korean Neurosurg Soc. 2008; 44:265–267.
8. Rocchi G, Caroli E, Frati A, Cimatti M, Savlati M. Lumbar spinal angiolipomas: report of two cases and review of the literature. Spinal Cord. 2004; 42:313–316.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download