Abstract
Multiple total knee arthroplasty (TKA) failure resulting from a recurrent infection is a challenging problem. Knee arthrodesis is one treatment option that normally involves the application of an external fixator, plate fixation, and intramedullary nailing. However, these approaches are not always successful, and a reinfection is a risk, particularly in older, medically compromised patients. This paper reports a new arthrodesis technique that uses a bundle of flexible intramedullary rods and an antibiotic-loaded cement spacer. This technique was used in two cases of multiple TKA failure that resulted from a recurrent infection. The procedure was successful in both cases with no evidence of rod or cement failure. Two advantages of this procedure are infection eradication and mechanical strength. However, this procedure should only be used for medically compromised elderly patients at high risk of rerevision TKA failure resulting from persistent periprosthetic infection because rod fracture or loosening can occur with time.
Infection after total knee arthroplasty (TKA) is an infrequent but serious complication that remains a challenging problem to treat. Although the standard treatment approach is a two-stage revision using antibiotic cement spacers,1) the failure rate can be high due to infection at the site. Salvage procedures for multiple TKA failures due to recurrent infection include arthrodesis, resection arthroplasty, and above-knee amputation. Arthrodesis is the preferable treatment option owing to its superior ambulatory potential.2) The goal of arthrodesis is achieving a bony union, which means that maximum contact between the viable knee joint bone surfaces is critical for success.3) However, multiple revision usually results in extensive bone loss that can hinder bony union in arthrodesis. Artificial arthrodesis using a long intramedullary nail and cement filler has been described for limb salvage after severe bone loss due to tumor resection.4) This technique has also been applied as a salvage procedure in cases of multiple TKA failure due to infection.5) However, current artificial arthrodesis techniques have many disadvantages, are not always successful, and may not be possible in all patients. The present report introduces our modified artificial arthrodesis method. This method involves the use of a bundle of flexible intramedullary rods and an antibiotic-loaded cement spacer. This approach was successfully used to treat two cases of multiple revision TKA failure due to persistent infection.
Patients were placed in a supine position as for standard TKA, and an anterior midline skin incision was made through the old scar. All previous prosthetic components were removed and cement was thoroughly excised using a small osteotome. Samples were taken for microbiological culture and pathological analysis, including intraoperative frozen sections to establish the extent of infection. Meticulous excision was performed to remove all remaining cement, granulation and necrotic devitalized tissue in a stepwise manner, including in the suprapatellar pouch, medial and lateral gutter, and posterior compartment of the knee. The sclerotic bony surfaces positioned by femoral and tibial components were cut back to the normal bone using a high-speed tip burr. Through the previous insertion site of the femur and tibial stem components, the medullary canal was debrided by retrograde (femur) and antegrade (tibia) intramedullary reaming in 0.5- or 1.0-mm increments to avoid possible infection. After thorough debridement, we determined tissue viability by observing blood oozing from the soft tissue and remaining bone stock using a 1-minute deflation of the tourniquet. Under fluoroscopy guidance, flexible intramedullary rods (Synthes Inc., West Chester, PA, USA) were inserted retrogradely in the femoral side with the knee in flexion. After the first rod was driven across the narrowest portion of the femoral canal (approximately 5 cm), second, third, fourth, fifth or more rods were inserted one by one as permitted by the intramedullary canal size. After filling the intramedullary canal, the inserted rods were tapped into the medullary canal for more secure positioning, and the end of each rod was cut at the level of the articular bony defect of the proximal tibia (Fig. 1A). The rods were then driven back securely into the proximal femur. We aimed for as much rod length as possible to cross the isthmus of the femoral canal to maximize stability. The rods on the tibial side were then antegradely inserted into the tibia using the same method as used on the femoral side. The tibial rods were trimmed to the level of the area of the distal anterior femoral cortex bone loss to maximize overlap with femoral-side rods (Fig. 1B). The rod ends from the femoral and tibial sides were arranged such that they overlapped and interdigitated (Fig. 1C) to maximize mechanical strength. The interdigitating rod ends were tightly fixed using two (or three) cerclage wires (Zimmer, Warsaw, IN, USA). Antibiotic-loaded cement was made by mixing two 40-g packs of Palacos bone cement (Biomet Merk, Warsaw, IN, USA) with 4 g vancomycin and 4.8 g tobramycin per cement pack. At the dough time period, usually 2 to 3 minutes from the beginning of the cement mixing, the cement was placed within the knee and polymerized so that the cement conformed to the irregular contour of the femur and tibia that resulted from the severe bone loss. The cement macrointerdigitated into bone defects and the intercondylar notch, extended into the medullary canal and suprapatellar pouch, and surrounded the rod bundle to create a cement arthrodesis of the knee joint (Fig. 1D). Postoperatively, patients were allowed to weight bear as tolerated. Patients were administered intravenous antibiotics until the wound dried, and were then administered oral antibiotics for 6 weeks.
The first patient was an 80-year-old woman who underwent a staged bilateral TKA in 2004 for degenerative osteoarthritis. Because of periprosthetic infection in the left TKA at postoperative 2 months, the patient then underwent a two-stage revision TKA comprising removal of the prosthesis and insertion of antibiotic cement followed by a 6-week antibiotic infusion and insertion of a stemmed-revision TKA component (Nexgen® LCCK, Zimmer; Legacy® knee constrained condylar knee, Zimmer). However, clinical signs of infection including pain, swelling, and drainage at the anterior aspect of proximal tibia continued for 9 months after this secondary surgery. The infecting organism was identified as methicillin-resistant Staphylococcus aureus (MRSA). Hematology findings included erythrocyte sedimentation rate (ESR: 76 mm/h) and C-reactive protein (CRP: 44 mg/dl) concentration. Radiology indicated stem loosening in the femur with a severe bone defect especially in the anterior tibia and around the anterior femur flange. The skin defect (3×2 cm) due to persistent drainage overlying the tibial tuberosity was prominent and expanding. We diagnosed a persistent prosthetic infection. The patient had infection recurrence, poor bone stock and was physico-psychologically compromised following multiple failed surgical interventions and old age. We decided to perform a one-stage artificial fusion with a bundle of flexible rods and an antibiotic-loaded cement spacer. The procedure was uneventful. At 8 weeks post-operatively, the joint showed no sign of infection, the patient could walk with a cane without pain. The most recent radiographs, at 44 months after surgery, showed no sign of rod or cement failure (Fig. 2).
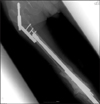
A 75-year-old man who had renal insufficiency underwent a right-side TKA in 2003 due to posttraumatic arthritis resulting from a tibial plateau fracture 10 years ago. Postoperative infection developed 6 months after TKA. A two-stage revision arthroplasty was performed but failed due to a recurrent MRSA infection. The patient refused a further revision TKA and was very concerned about reinfection. Therefore, we performed a knee arthrodesis. It was not possible to use a long intramedullary nail because the patient had a dynamic hip screw on the ipsilateral (right) hip for a previous intertrochanteric fracture. Therefore, knee arthrodesis using dual plate fixation was performed. However, pain, swelling and elevated ESR and CRP levels persisted for 6 months after arthrodesis. Therefore, we performed artificial fusion using a flexible rod bundle and antibiotic-loaded bone cement. The previous plates were removed and a thorough debridement performed, after which the rods and cement were applied (Fig. 3). Partial weight-bearing was permitted 1 week after surgery, and full weight-bearing was allowed at 3 weeks postoperatively. At a 56-month follow-up, the patient could walk independently without any support and without pain. There was no evidence of infection according to physical, laboratory or radiograph examinations. Similarly, there was no evidence of rod or cement failure.
Arthrodesis is regarded as an effective limb-salvage procedure following multiple TKA failure due to recurrent infection, and commonly involves external fixation, compression with external pin frame devices, and internal fixation using either an intramedullary nail or plate fixation. However, the arthrodesis success rates using these fixation methods in patients with a TKA site infection are only 50% to 80%,6) and none of these fixation methods is complete.
The ultimate goal of arthrodesis is bony union of the femorotibial joint. Therefore, a major problem in cases of multiple failed revision TKAs due to recurrent infections is the extensive bone loss in the proximal tibia and distal femur. In cases of marked bone loss at the TKA site, especially after revision TKA, substantial leg shortening is unavoidable after knee arthrodesis due to tibial and femoral bone cutting for maximum contact between viable bleeding cancellous bone. In a series of 19 knee arthrodeses using an intramedullary nail, De Vil et al.6) reported an average limb-length discrepancy of 4.5 cm. Thus, the assumption that arthrodesis of the knee is always possible as a salvage procedure appears to be invalid. In cases with severe bone loss, artificial fusion7) can be an alternative to arthrodesis because it can restore functional ability after surgery without leg length discrepancy by using a cement spacer to compensate for bone loss.
The use of a long intramedullary nail and a cement spacer was devised originally as a limb salvage procedure after tumor excision.4) This technique has subsequently been applied to infected TKA salvage cases involving severe bone destruction. Our modified arthrodesis method described here used flexible intramedullary rods rather than a rigid nail. This surgical technique has advantages over artificial fusion using an antegrade rigid nail. Firstly, the procedure uses the same surgical approach as was used for the previous TKA, thereby simplifying the approach and reducing trochanteric pain by avoiding unnecessary incisions. Retrograde flexible rod insertion on the femoral side also results in reduced trochanteric pain, as such pain usually arises from antegrade rigid nail insertion from a greater trochanter. Secondly, flexible rods are easier to source and cheaper than rigid nails; in particular, it is often difficult to source long intramedullary nails as they are not commonly required, and custommade short stems with a connector are also difficult to obtain due to their high cost. Finally, retrograde insertion of a more manageable flexible rod allows for versatile surgical indications. As observed in the second case reported here, use of an antegrade long intramedullary nail may not be possible in some patients due to previous hip surgery in the ipsilateral side resulting in obstruction by the femoral stem or dynamic hip screw; such hip surgery is not uncommon in older patients.
A major concern of artificial fusion is longevity of the flexible rod and antibiotic-loaded cement spacer. Although not an infected TKA study, Capanna et al.8) reported a 4.5-year follow-up of a series of 76 patients treated with an intramedullary rod and cement spacer after distal femur or proximal tibia tumor resection. The implant lasted longer than expected, with only 12 (16%) cases of failure (i.e., fracture, bending, or migration of the rod). It should also be noted that the mechanical strength of cement is many times greater than required in the clinical ambulatory setting, and that even a 45% decrease in compressive strength due to addition of antibiotics would not compromise its function as a spacer.9) This is consistent with observations that many complications associated with antibiotic-loaded cement static spacers do not involve cement fracture but rather quadriceps and soft tissue contracture.10)
A limitation of artificial fusion is that bone healing cannot occur and that rod fracture or loosening usually occurs over time. Therefore, this procedure should be limited to low demand elderly patients with multiple failed TKAs due to infection recurrence and who are medically compromised. In our opinion, in cases of failed artificial fusion, reartificial fusion (i.e., removal of the cement spacer and rods and use of another set of rods and cement spacer) using the present method may be the best option because it is technically easier than bone transport using an Ilizarov intercalary allograft or fitting a tumor prosthesis.
In conclusion, artificial arthrodesis using a bundle of flexible intramedullary rods and an antibiotic-loaded static cement spacer was a successful salvage procedure for multiple failed TKAs due to infection and where there was extensive bone loss and poor bone stock. The method provides for infection eradication and sufficient mechanical strength for early ambulation. We believe that this simple method can be used in medically compromised elderly patients at high risk of rerevision TKA failure due to persistent periprosthetic infection.
Figures and Tables
Figure 1
(A) Flexible rods were inserted retrogradely until they filled the femur medullary cavity, after which they were trimmed at the level of the articular bony defect of the proximal tibia. (B) Flexible rods were inserted antegradely until they filled the tibial cavity, after which they were trimmed at the level of the distal femur bony defect to allow sufficient overlap with rods from the femoral side. (C) Overlapping rod ends from the femoral and tibial sides were interdigitated and fixed using cerclage wires. (D) During the dough time period, antibiotic-loaded cement was placed within the knee and molded to the irregular contours of the bony defects of the distal femur and proximal tibia.

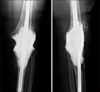
Figure 2
Knee anteroposterior (A) and lateral (B) radiographs at postoperative 40 months showing the flexible rod bundle with cerclage wires crossing from the femur to the tibia, and antibiotic-loaded cement used to compensate for bone loss. Note the lack of evidence of rod or cement spacer failure.
References
1. Hart WJ, Jones RS. Two-stage revision of infected total knee replacements using articulating cement spacers and short-term antibiotic therapy. J Bone Joint Surg Br. 2006; 88:1011–1015.
2. Senior CJ, da Assunção RE, Barlow IW. Knee arthrodesis for limb salvage with an intramedullary coupled nail. Arch Orthop Trauma Surg. 2008; 128:683–687.
3. Klinger HM, Spahn G, Schultz W, Baums MH. Arthrodesis of the knee after failed infected total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2006; 14:447–453.
4. Campanacci M, Costa P. Total resection of distal femur or proximal tibia for bone tumours. Autogenous bone grafts and arthrodesis in twenty-six cases. J Bone Joint Surg Br. 1979; 61-B:455–463.
5. Sundgren K. Cemented modular intramedullary nail in failed knee arthroplasty--a report of 2 cases. Acta Orthop Scand. 1999; 70:305–307.

6. De Vil J, Almqvist KF, Vanheeren P, Boone B, Verdonk R. Knee arthrodesis with an intramedullary nail: a retrospective study. Knee Surg Sports Traumatol Arthrosc. 2008; 16:645–650.

7. Persson BM, Rydholm A. Artificial fusion of the knee joint with intramedullary nail and acrylic cementation following radical excision for tumor. Arch Orthop Trauma Surg. 1984; 102:260–263.

8. Capanna R, Biagini R, Ruggieri P, Bettelli G, Casadei R, Campanacci M. Temporary resection-arthrodesis of the knee using an intramedullary rod and bone cement. Int Orthop. 1989; 13:253–258.

9. Hsieh PH, Tai CL, Lee PC, Chang YH. Liquid gentamicin and vancomycin in bone cement: a potentially more cost-effective regimen. J Arthroplasty. 2009; 24:125–130.

10. Ha CW. A technique for intraoperative construction of antibiotic spacers. Clin Orthop Relat Res. 2006; 445:204–209.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download