Abstract
Biceps long head tendon rupture is relatively common and requires approximately four weeks of splintage as a general treatment. Musculocutaneous nerve entrapment is commonly caused by excessive exercise or direct external force. Musculocutaneous nerve syndrome has barely been reported; however, association of biceps long head tendon rupture and musculocutaneous nerve entrapment syndrome has never been reported. The authors experienced a 70-year-old male patient, who suffered a traffic accident and was hospitalized due to shoulder joint pain caused by direct external force, delayed forearm lateral aspect hypoesthesia and elbow flexion weakness. For identification of the cause, magnetic resonance imaging, electromyography, and surgical opinion were synthesized, resulting in diagnosis of delayed musculocutaneous nerve entrapment syndrome occurring after biceps long head tendon rupture. With surgical treatment, pain, sense, and elbow flexion weakness were recovered, a showing successful treatment result.
Musculocutaneous nerve arises from the lateral nerve bundle of brachial plexus. After innervating coracobrachialis, musculocutaneous nerve drives the way between biceps brachii and brachialis diagonally and then goes the upper arm laterally on and on. After then, it pierces through the deep fascia of brachiallis right in the upper part of elbow joint and becomes lateral antebrachial cutaneous nerve, driving the forearm part laterally. Because of such pathway, musculocutaneous nerve is rarely damaged alone and can be easily co-damaged when biceps brachii is damaged.1) When it's pressed in the area of coracobrachialis muscle, damages may occur to all the motor and sensory nerves, but when it's pressed in the area of terminal nerve branch, only sensory nerve is usually damaged.2) In general, such nerve entrapment symptoms are treated with conservative treatment, and when there is no treatment effect, it can be treated with surgical method.3)
Musculocutaneous nerve entrapment syndrome has been rarely reported in the operation of dislocation of shoulder or arthroscopic shoulder-joint.4) However, musculocutaneous nerve entrapment syndrome, which was delayed after biceps long head tendon damage, has not been reported yet. The authors get favorable progress through surgical treatment regarding the delayed musculocutaneous nerve entrapment syndrome 1 case, occurred in the process of conservative treatment of biceps long head tendon rupture after traffic accident and make a report on it with literature review accordingly.
He was a 70-year-old male patient, who had injuries in the left shoulder side by out-car traffic accident and was hospitalized due to pain. On the day he was injured, he complained of tenderness at left shoulder and anterior aspect of upper arm, worsening pain when doing an exercise in the left shoulder from the physical exam in emergency room. There was no definite abnormal finding in simple radiographic examination, but left elbow joint flexion force and elbow supination force reduced (motor grade 4/5). Hypoesthesia, numbness, and referred pain were not found around the injured area. Also there was no neurologic abnormality at distal portion of injured area such as forearm, hand. It was determined that long arm splint should be applied and then conservative treatment and close follow-up.5)
On the second day of his injury, he came to outpatient clinic due to continuous pain in the injured area. A mass as big as the size of an egg, which wasn't observed in the emergency room was felt in the middle of upper arm and 'Popeye sign' was shown and more noticeable when elbow flexion status. Elbow flexion, forearm supination force reduction (grade 4/5) was not changed. From the magnetic resonance imaging (MRI) conducted when biceps brachii rupture was doubted,6) biceps brachii long head tendon was dislocated after rupture and observed in the middle of upper arm: it was dislocated downward by about 12 cm than the normal location (Fig. 1). The dislocated biceps brachii long head tendon was adjacent to musculocutaneous nerve,7) but musculocutaneous nerve rupture or abnormal driving pathway was not found (Fig. 2). We recommended the patient to do the surgery of decompression and tendon suture, but he refused to do so for his personal reason.
For progress observation on the sixth weeks after injury, he came to Inha University Hospital while leaning on the long arm splint and appealed that he had hypoesthesia in the left forearm lateral side (grade 5/10) and numbness, and intermittent referred pain and worsened upper arm muscle force decreased (motor grade 3/5). To detect the musculocutaneous nerve injury, electromyography was performed and then it was observed that there was a compatible opinion on the temporary paralysis of musculocutaneous nerve (Table 1, 2).
We assumed that upper arm pain, elbow flexion force reduction was appeared by biceps brachii long head tendon injury at initial visit. At MRI exam, ruptured biceps brachii long head tendon was dislocated downward and positioned just near to musculocutaneous nerve. But there was no definite associated symptom. Six weeks after injury, hypoesthesia was appeared at lateral side of forearm which was not found at initial exam. We thought that conglutination between musculocutaneous nerve and ruptured biceps brachii long head tendon was occurred in healing process. In succession, musculocutaneous entrapment symptom was appeared at last follow-up. Accordingly, on the 45th day after injury, surgical decompression was conducted.
In terms of surgical opinion, biceps brachii long head tendon was ruptured at intertubercular groove area and dislocated downward by about 13 cm from the greater tuberosity of humerus and conglutinated adjacently right to the musculocutaneous nerve. The driving pathway to musculocutaneous nerve was normal, but the part which was conglutinated area had narrow pathway (Fig. 3). The authors peeled off the conglutinated musculocutaneous nerve and biceps brachii long head tendon, moved the peeled-off biceps long head tendon upward than musculocutaneous nerve, and moved it into anatomical location where musculocutaneous nerve drives between biceps brachill and brachialis muscle for tenodesis.
On the second day after operation, abnormal sense became better (grade 7/10) and the pain in the injury part reduced. On the 2nd week after operation, elbow flexion force (grade 5/5) recovered. Two months after operation, forearm lateral side abnormal sense became better and elbow flexion force (grade 5/5) maintained in the follow-up. On the sixth month after operation, the patient could maintain in the state of being able to do his daily life without appeals to special symptoms in the follow-up.
Musculocutaneous nerve entrapment syndrome after excessive exercise or shoulder-joint operation have been reported several times.5) Musculocutaneous nerve can be pressed depending on bulky coracobrachialis and its excessive use, and accordingly nerve palsy or Wallerian contracture may occur.8) Avulsion injury can occur when shoulder joint anterior dislocation or arm is strongly abducted or rotated externally. But, the musculocutaneous nerve entrapment symptom occurred after biceps brachii long head tendon damage has not been reported yet.
When biceps brachii long head tendon is ruptured, the ruptured part is dislocated to downward than the normal location. However, there is a small amount of activity in general or elderly patients can obtain satisfactory treatment result through splint or conservative treatment than the surgical treatment. Young patients or patients who require a lot of activity can be treated with tenodesis. In this case, we recommend conservative treatment at initial, considering patient age and activity. But at follow-up exam, the treatment plan changed to surgical management due to neurologic deficit development.
Musculocutaneous nerve entrapment symptom must be differential diagnosed from biceps brachii rupture, C5 or C6 radiculopathy, Brachial plexus damage.8) When biceps brachii long head tendon is ruptured, 'Popeye Sign', which can be felt like mass characteristically may appear on the anterior upper arm. But it does not involve abnormal sense. C5, C6 radiculopathy appears as neck pain or radiating pain and can be detected by electromyography. Brachial plexus damage can be generally detected from the observation that either the entire upper extremity muscle force reduction or hypoesthesia occurs.6,8)
This case of disease is considered that biceps brachii rupture and musculocutaneous nerve entrapment symptom occurred in order. It seems that the ruptured biceps long head tendon was dislocated downward and the musculocutaneous nerve was located right next to the driving pathway, and then in the process of recovering, conglutination between the two tissues occurred. If musculocutaneous nerve is damaged in coracobrachialis area, biceps brachii and brachialis force reduction and anterior/lateral forearm hypoesthesia may occur, but in this case of disease, it seems that although there was no damage in the musculocutaneous nerve itself, it was conglutinated with surrounding tissues in the process of recovering and subsequently captured neuropathy occurred. If there is initial traction injury of musculocutaneous nerve, the patient might be hypoesthesia at initial physical exam. It can be interpreted that the upper arm muscle force reduction occurred when the initial biceps long head tendon ruptured and after the occurrence of conglutination, delayed musculocutaneous nerve entrapment symptom occurred with muscle force reduction and forearm hypoesthesia.
Therefore, if the pain gets better in the patient with biceps brachii rupture, we recommend that early range of motion exercise is necessary as soon as possible with arm sling protection. We should avoid long-term splint or immobilization to prevent complication like above case. In addition, although splint or conservative treatment was performed initially, we should do careful follow-up evaluation of patient symptom. If symptom changes like biceps muscle force reduction and forearm hypoesthesia are seen in a follow-up, we can consider more evaluation such as MRI, electromyography. As a result of exam, active surgical treatment would be required.
Figures and Tables
Figure 1
T2-weighted magnetic resonance imaging coronal section, biceps brachii long head tendon (thin arrow) ruptured and distracted from humerus great tuberosity approximately 12 cm.
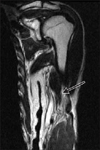
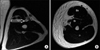
Figure 2
T2-weighted magnetic resonance imaging axial section, (A) migrated biceps brachii (Bb) long head tendon (thick arrow) located just next to the musculocutaneous nerve (thin arrow) at the left mid-arm level in this patient. (B) Normal musculocutaneous nerve (thin arrow) observed between Bb muscle and brachialis muscle (Br) at the left mid-arm level.
References
1. Yilmaz C, Eskandari MM, Colak M. Traumatic musculocutaneous neuropathy: a case report. Arch Orthop Trauma Surg. 2005; 125:414–416.

2. Dailiana ZH, Roulot E, Le Viet D. Surgical treatment of compression of the lateral antebrachial cutaneous nerve. J Bone Joint Surg Br. 2000; 82:420–423.

3. Felsenthal G, Mondell DL, Reischer MA, Mack RH. Forearm pain secondary to compression syndrome of the lateral cutaneous nerve of the forearm. Arch Phys Med Rehabil. 1984; 65:139–141.
4. Ma H, Van Heest A, Glisson C, Patel S. Musculocutaneous nerve entrapment: an unusual complication after biceps tenodesis. Am J Sports Med. 2009; 37:2467–2469.
5. Krupp RJ, Kevern MA, Gaines MD, Kotara S, Singleton SB. Long head of the biceps tendon pain: differential diagnosis and treatment. J Orthop Sports Phys Ther. 2009; 39:55–70.

6. Neal S, Fields KB. Peripheral nerve entrapment and injury in the upper extremity. Am Fam Physician. 2010; 81:147–155.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download