Abstract
Materials and Methods
A total of 38 patients were included in this study, who visited Daegu Catholic Medical Center from August 2, 2011 to September 2, 2011. Bacterial culture was performed at the pre-scrub, post-scrub, and postoperation; patients were divided into two groups according to use of povidone iodine (3.75%) and povidone iodine with Softa-Man® as antiseptic agents at the surgical.
Results
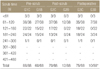
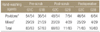
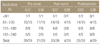
Comparison between the antiseptic solutions showed a significant difference for the presence of gram positive cocci (p=0.034), however, no difference was observed for the presence of gram positive bacilli (p=0.838). As the scrub time increased, the positive detection ratio of bacteria decreased (p=0.000), and decreased significantly at more than 120 seconds. However, positive detection ratio of bacteria increased significantly at more than 300 seconds in cases with povidone iodine only (p=0.014). Glove wearing time did not have a significant influence on the positive detection ratio of bacteria, and no significant difference was observed between the antiseptic solutions (p=0.143).
Figures and Tables
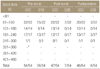
Table 3
Relationship between Scrub Time and Bacterial Growth after Culture with Povidone Iodine as a Hand-Washing Agent
References
1. Yinusa W, Li YH, Chow W, Ho WY, Leong JC. Glove punctures in orthopaedic surgery. Int Orthop. 2004; 28:36–39.

2. Eitzen HE, Ritter MA, French ML, Gioe TJ. A microbiological in-use comparison of surgical hand-washing agents. J Bone Joint Surg Am. 1979; 61:403–406.

3. Gruendemann BJ, Bjerke NB. Is it time for brushless scrubbing with an alcohol-based agent? AORN J. 2001; 74:859–873.

4. Berguer R, Heller PJ. Strategies for preventing sharps injuries in the operating room. Surg Clin North Am. 2005; 85:1299–1305.

5. Hollaus PH, Lax F, Janakiev D, Wurnig PN, Pridun NS. Glove perforation rate in open lung surgery. Eur J Cardiothorac Surg. 1999; 15:461–464.

6. Thanni LO, Yinusa W. Incidence of glove failure during orthopedic operations and the protective effect of double gloves. J Natl Med Assoc. 2003; 95:1184–1188.
9. Chapman S, Duff P. Frequency of glove perforations and subsequent blood contact in association with selected obstetric surgical procedures. Am J Obstet Gynecol. 1993; 168:1354–1357.

10. St Germaine RL, Hanson J, de Gara CJ. Double gloving and practice attitudes among surgeons. Am J Surg. 2003; 185:141–145.
11. Quebbeman EJ, Telford GL, Wadsworth K, Hubbard S, Goodman H, Gottlieb MS. Double gloving. Protecting surgeons from blood contamination in the operating room. Arch Surg. 1992; 127:213–216.
12. Webb JM, Pentlow BD. Double gloving and surgical technique. Ann R Coll Surg Engl. 1993; 75:291–292.
13. Avery CM, Taylor J, Johnson PA. Double gloving and a system for identifying glove perforations in maxillofacial trauma surgery. Br J Oral Maxillofac Surg. 1999; 37:316–319.

14. Greco RJ, Garza JR. Use of double gloves to protect the surgeon from blood contact during aesthetic procedures. Aesthetic Plast Surg. 1995; 19:265–267.

15. de Castro-Peraza ME, Garzón-Rodríguez E, Rodríguez-Pérez V, Sosa-Alvarez I, Gutierrez-Hernández J, Asiain-Ugarte C. Glove perforation in surgery and protective effect of double gloves. Enferm Clin. 2010; 20:73–79.
16. Korniewicz DM. Barrier protection of latex. Immunol Allergy Clin North Am. 1995; 15:123–136.
17. Furukawa K, Ogawa R, Norose Y, Tajiri T. A new surgical handwashing and hand antisepsis from scrubbing to rubbing. J Nippon Med Sch. 2004; 71:190–197.

18. Girard R, Aho LS, Aupée M, et al. Alcohol-based rubs for hand antisepsis. Lancet Infect Dis. 2008; 8:584–585.

19. Al-Naami M, Anjum M, Afzal M, et al. Alcohol-based handrub versus traditional surgical scrub and the risk of surgical site infection: a randomized controlled equivalent trial - annotated bibliography. EWMA J. 2009; 9:5–6. 8–10.
20. Larson E. Guideline for use of topical antimicrobial agents. Am J Infect Control. 1988; 16:253–266.

21. Hobson DW, Woller W, Anderson L, Guthery E. Development and evaluation of a new alcohol-based surgical hand scrub formulation with persistent antimicrobial characteristics and brushless application. Am J Infect Control. 1998; 26:507–512.

22. Herruzo-Cabrera R, Vizcaino-Alcaide MJ, Fdez-Aciñero MJ. Usefulness of an alcohol solution of N-duopropenide for the surgical antisepsis of the hands compared with handwashing with iodine-povidone and chlorhexidine: clinical essay. J Surg Res. 2000; 94:6–12.

23. Tucci VJ, Stone AM, Thompson C, Isenberg HD, Wise L. Studies of the surgical scrub. Surg Gynecol Obstet. 1977; 145:415–416.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download