Abstract
Limb salvage should be considered after complete remission in young and physically active patients with osteosarcoma. Herein we described a patient who was treated with whole knee allograft reconstruction for the clinical implications of biological reconstruction which can avoid the problems with several consecutive sessions of mega-prosthesis revision. The mid-term result of this whole knee joint allograft reconstruction showed that it provided optimal joint congruence with durable joint stability, well balanced mechanical axis without joint space narrowing, and satisfactory gait pattern.
The distal femoral or proximal tibial hemi-side osteoarticular allografts have been widely used for skeletal reconstruction in patients with malignant bone tumors of adjacent knee joint. The overall rate of distal femoral osteoarticular allograft survival was 78% at ten years, and the rate of allograft survival without the need for resurfacing with a knee prosthesis was 71% at ten years.1) Despite the fact that hemi-osteoarticular allograft reconstruction shows a good long-term outcome, this reconstruction has raised various problems such as articular incongruence due to condylar size mismatching and joint instability due to ligament connecting.
We report herein a successful case of limb salvage surgery with a whole knee joint allograft containing the distal femur, proximal tibia and fibula, collateral and cruciate ligaments, menisci, joint capsule and patella tendon in a patient with an osteosarcoma of lower leg. The patient was informed that data concerning the case would be submitted for publication, and he consented.
A 16-year-old boy presented with intermittent pain in the right knee for 5 months. On physical examination, he had a normal range of knee joint motion and no palpable mass and neurologic deficiency; however, there was tenderness on the lateral condylar area and tuberosity of the proximal tibia. The initial magnetic resonance (MR) images exhibited a soft tissue extension toward fibular and lateral joint capsular area (Fig. 1A, 1B). Plain radiographs of the knee joint revealed bony destruction with osteolytic and sclerotic nature at the lateral eccentric location of right proximal tibia as well as tibial tuberosity (Fig. 1C, 1D). Positron emission tomography, bone scan and chest computed tomography showed no metastatic lesion. Histopathological examination of the tissue by incisional biopsy confirmed osteoblastic osteosarcoma (Fig. 1E).
During the neoadjuvant chemotherapy, we released the patient's information including age, sex, height and weight and lesion site to the regional bone bank. The most optimal size and quality was selected by clinical matching and plain radiographs. This current whole knee joint allograft was obtained from a 34-year-old male donor. The whole knee joint allograft was harvested by segmental cutting of lower leg between middle of thigh and middle of lower leg (Fig. 2A). We could not inspect of allograft's abnormality by MR imaging since it was frozen, therefore we just have informed bone-size matching by plain radiographs before surgery (Fig. 2B).
The procedure and possible complications were fully explained before the surgery and we obtained operative permission for using whole knee joint allograft.
Immediately after starting operation, the fresh frozen allograft was thawed in warm saline water, and its soft tissue of outside the joint capsule was removed with patella. The damage to the menisci, collateral and cruciate ligaments, and articular cartilage was thoroughly inspected and confirmed normality of all the joint structures (Fig. 2C). Surgery was performed through the lateral approach which included the previous biopsy site. Wide excision was conducted by osteotomy at a 6.5 cm of the proximal fibula, 13 cm of the proximal tibia and 4.5 cm of the distal femur from the knee joint. Wide excision of soft tissue was performed including lower half of the patella tendon, the anterior tibial artery and branches of the common peroneal nerve and parts of the anterior and deep posterior compartment muscles. The quadriceps tendon, patella and the upper half of the patella tendon, and joint capsule of suprapatellar pouch were remained. Since there were no specific abnormalities on the prepared allograft, extracorporeal osteotomy of allograft was performed as the same length of excised bones. Osteosynthesis was carried out from the proximal tibia and fibula to the femur. Unreamed tibial nail (Synthes, Solothurn, Switzerland) and anatomical locking plate were used for tibia, the intramedullary ulna rod (Acumed, Hillsboro, OR, USA) was inserted for fibula, and the anatomical locking plate (Synthes) applied for femur osteosynthesis (Fig. 3). The patella tendon and joint capsule of allograft sutured to the each remnant host's one. We don't need sutures for connecting of anterior and posterior cruciate ligaments as well as medial and lateral collateral ligaments. The medial gastrocnemius muscle transposition and split thickness skin graft was done for exposed tibia.
Although the patient was given access to a patient-controlled analgesia pump which was programmed to deliver analgesics on demand up to the third postoperative day, pain could be controlled with intermittent medication thereafter. Long leg splint immobilization was maintained by fourth week but quadriceps muscle strengthening exercise permitted all the time after surgery. Passive and active joint exercise was started from postoperative fifth week. Non-weight bearing two-crutch ambulation was started from two months, and partial weight bearing was permitted 3 months after surgery. In the third postoperative month, the knee was able to actively move in 120 degrees of flexion without any block of extension. The weight bearing ambulation without supporting tool was started from the postoperative 6 months. Ankle-foot orthosis was applied for weak dorsiflexion of ankle joint. Histopathological examination of the surgical specimen revealed 80% tumor necrotic rate by neoadjuvant chemotherapy. The wedge resections were performed for the metastatic nodule on the lower lobe of left lung at one year, and lower lobe of right lung at 20 months after limb salvage surgery. This patient has been followed-up until to postoperative 40 months with no evidence of disease state after finish of chemotherapy schedule.
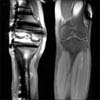
The follow up plain radiographs (Fig. 4) showed well union process and maintained skeletal axis without joint space narrowing and other complication. Although the MR imaging was not clear due to metal artifact, it seems like normal joint structures including cruciate ligaments and menisci (Fig. 5). All osteotomy sites showed stable union after postoperative 24 months. The patient was able to ambulate without walking aid until to last follow-up month. The musculoskeletal tumor society functional score2) was recorded 27 (90%) points at postoperative 24 months and 28 (93%) points at 36 months.
This current patient showed decreased right knee joint flexion/extension than normal side, and also the right hip joint flexion/extension and pelvic tilt were decreased in the 3-dimensional gait analysis3) applied at postoperative 36 months (Fig. 6). Therefore the strengthening exercise of abdominal and pelvic muscle was recommended as a rehabilitation program.
It has been hard to reconstruct a surgical defect using a distal femoral or a proximal tibial osteoarticualr allograft due to size mismatching with host condyle. Radiologic matching by computed tomography or plain radiography is currently the best option for detecting a similar-sized allograft. Muscolo et al.1) selected distal femoral osteoarticular allografts by measuring maximum total width, the anteroposterior dimension of the medial and lateral condyles and the width of the intercondylar notch. Their proximal tibial osteoarticular allograft were selected by comparing the age, gender, height, and radiographs of the patient with corresponding data from the donor to achieve the closest anatomic match.4) Whole knee joint allograft reconstruction does not require matching process but it should be obtained from a young healthy donor without a previous history of knee joint diseases or injuries. It has been reported that fracture is a common complication of allografts and that the incidences of infection and fracture are relatively high.5,6) In current case, we applied dual internal fixation using intramedullary nail and locking plate of titanium alloy implants for the tibia to prevent allograft fracture and easy radiological follow-up.
Unlike hemiside osteoarticular allograft, the whole knee joint allografts may result in less frequent meniscus injury or fatigue stress of the cruciate ligaments due to best matched joint congruence as well as less frequent articular destruction due to optimal joint excursion. Beside, whole knee joint allograft is no need for host-allograft sutures of the cruciate and collateral ligaments and joint capsule, the joint laxity or postoperative ankylosis may be less occurs.
A previous experimental study in a rabbit model has demonstrated that there is no significant difference in subsequence reintegration of cartilage, menisci and ligaments between whole knee joint autografts treated with heating at 60℃ for 30 minutes and those that are not.7,8) However, in the patient using pasteurized whole knee joint autograft, the early collapse of medial condyle of tibia and excessive ankylosis were occurred.9) Meniscal allograft transplantation has been already performed for 20 years and has played an important role in reducing knee joint pain and increasing function.10)
If a matched tibial hemiosteoarticular allograft is not available, a whole knee joint allograft can be a good alternative option as biological reconstruction. The host-allograft bone fixation without ligaments and capsular suturing of the knee can provide wider surgical margin, convenient surgical procedure with achieving best joint congruence and minimize joint laxity.
This mega-biologic reconstruction using whole knee joint allograft in the limb salvage surgery showed yet durable but need further observation through long lasting period with case collection.
Figures and Tables
 | Figure 1(A) A coronal magnetic resonance (MR) image showed an eccentric laterally located tumor of the right proximal tibia touching upward with joint cartilage and capsule. (B) A transverse view MR image showed extraosseous tumor extension to the anterior compartment. (C) Anterior-posterior plain radiograph showed bony destruction with osteolytic and sclerotic nature. (D) Lateral plain radiograph showed tumor extension to the tibial tuberosity. (E) The osteoblastic osteosarcoma was diagnosed (H&E, ×200). |
 | Figure 2(A) Photograph showing the delivered whole knee joint fresh frozen allograft. (B) Plain radiograph showed a similar bony size compare with the patient's knee. (C) Photograph illustrates the good intra-articular condition after removal of muscle and patellar bone. |
 | Figure 4Anterior-posterior (A) and lateral (B) radiographs taken 36 months after surgery bone union has been processed in the osteotomy sites. |
References
1. Muscolo DL, Ayerza MA, Aponte-Tinao LA, Ranalletta M. Use of distal femoral osteoarticular allografts in limb salvage surgery. J Bone Joint Surg Am. 2005; 87:2449–2455.

2. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993; 286:241–246.

3. Jang IG, Park HS, Nam KW, et al. 3D gait analysis of limb salvage patients with osteoarticular knee allograft reconstruction. J Biomed Eng Res. 2010; 31:74–80.
4. Muscolo DL, Ayerza MA, Farfalli G, Aponte-Tinao LA. Proximal tibia osteoarticular allografts in tumor limb salvage surgery. Clin Orthop Relat Res. 2010; 468:1396–1404.

5. Hornicek FJ Jr, Mnaymneh W, Lackman RD, Exner GU, Malinin TI. Limb salvage with osteoarticular allografts after resection of proximal tibia bone tumors. Clin Orthop Relat Res. 1998; 352:179–186.

6. Hornicek FJ, Gebhardt MC, Tomford WW, et al. Factors affecting nonunion of the allograft-host junction. Clin Orthop Relat Res. 2001; 382:87–98.

7. Judas F, Rosa S, Teixeira L, Lopes C, Ferreira Mendes A. Chondrocyte viability in fresh and frozen large human osteochondral allografts: effect of cryoprotective agents. Transplant Proc. 2007; 39:2531–2534.

8. Ahmed AR, Watanabe H, Takagishi K. Reconstruction with autologous pasteurized whole knee joint I: experimental study in a rabbit model. J Orthop Sci. 2003; 8:170–179.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download