Abstract
Patella infera (baja) is a rare condition that can result from several etiologies including trauma around the knee. Risk factors include scar tissue formation in the retropatella fat pad, extensor mechanism dysfunction, immobilization in extension position of the knee joint, etc. Unawareness and delayed recognition are known to be associated with long-term disability. In this condition, arthroscopic treatment is generally recommended only for early cases. In this report, we present a case with reasonable outcome of delayed patella infera treated by arthroscopic treatment. Prudent arthroscopic debridement of the responsible scar tissue and accelerated rehabilitation therapy is necessary for achievement of a successful outcome.
Patella infera (baja) is a condition with an abnormally low patella, which may be associated with several etiologies including poliomyelitis,1) tourniquet paralysis of the quadriceps,2) fractures about the knee,3) following harvesting of the patella tendon for anterior cruciate ligament reconstruction,4,5) and high tibial osteotomy6,7) etc. The patella infera has been supposed to result from biological adaptation of the extensor mechanism, shrinking of scar tissue, scarring, formation of new bone, immobilization and patellofemoral fibrosis, intra-articular fibrous bands, ischaemia and trauma to the patella tendon.4,6,7)
Treatment of patella infera is difficult. However, early recognition and intervention seem to improve outcomes compared with the natural history of this condition.5) The arthoscopic treatment is known to be effective if the condition is recognized early, that is within 6 months.5) In this report, we present a case of delayed patella infera occurring after conservative management of inferior pole fracture of patella. Prudent arthroscopic debridement without any direct surgical procedure on contracted patella tendon together with accelerated rehabilitation therapy showed reasonable outcome even in this delayed case. The patient and the guardians were informed that data concerning the case would be submitted for publication.
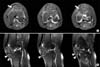
A 44-year-old woman fell onto her left knee (direct injury) during walking. She visited local hospital and the initial radiographs revealed a minimally displaced transverse fracture at inferior pole of the patella (Fig. 1A). Nonoperative treatment was decided, and long leg splint was applied for six weeks allowing partial weight using crutches. The splint was removed under supervision of orthopaedic doctor after reviewing the follow-up radiograph. Outpatient physical therapy including gentle range of motion (ROM) exercise was started at that point. The five month follow up radiographs demonstrated progression of union without displacement of fracture fragment (Fig. 1B). The lateral view of the knee revealed an Insall-Salvati ratio of 1.0. However, despite of supervised physical therapy, the patient continuously had discomfort around patella and referred to our hospital for further evaluation.
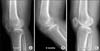
On initial visit to our clinic, she showed antalgic gait. On physical examination, tenderness was present at the inferior aspect of patella, and the mobility (including mediolateral and superoinferior translation motion) of patella was markedly decreased. She had quadriceps atrophy (3 cm decreased mid-thigh circumference compared to the contralateral limb). Her left knee ROM was between flexion contracture 15° and further flexion of 50°. Extension block was present. The lateral radiographs revealed an Insall-Salvati ratio of 0.41 (Fig. 1C) and further decreased over a month (Fig. 1D). The magnetic resonance imaging showed hypertrophied soft tissue from retropatella fat pad area to medial retinaculum (Fig. 2A). In addition, thickened patella tendon with intrasubstance signal change was also identifiable (Fig. 2B).
With the impression of delayed patella infera, the patient underwent arthroscopic surgery. Initially, superolateral and superomedial portals were used as a working and viewing portal visa versa. By expecting a cramped space at retropatella area, it was easy to identify the lesions by using these superior portals. Arthroscopy revealed thickened fibrotic scar tissue extending from the retropatella fat pad area to medial retinaculum tethering the patella tendon (Fig. 3). This scar tissue was extensive and after debridement of this thickened fibrotic tissue, mobility of the patella bone was improved. Then, standard anteromedial and anterolateral portals were made after debridement. Further debridement of interface between the patella tendon and the upper tibia was performed until the tibial insertion site of patella tendon was visible. Passive knee flexion of 130° was gained intraoperatively.
Postoperatively, the patient participated in an accelerated rehabilitation therapy including early range of knee motion with emphasis on full extension and patella mobility. The quadriceps and hamstring exercise was concomitantly applied. Progressive improvement of knee motion was observed and at 12 month follow up, Insall-Salvati ratio was 0.55 with knee ROM of 5 to 100 degrees (Fig. 4).
Prognostic factors for patella infera are not well described in any literature, Noyes et al.5) emphasized the importance of early diagnosis, that is within 6 months. The progression phase they suggested were characterized by transient patella infera resulting from peripatella scar tissue formation including the retropatella fat pad, leading to contracture of the retropatella fat pad scar tissue, and quadriceps weakness or malfunction usually accompanied by decreased motion. Eventually, permanent shortening of the patella tendon leading finally to patellofemoral arthrosis occurs. They recommended that diagnosis and intervention within 6 months can lead to improvement in function, decrease shortening of the patella tendon, and prevent permanent contracture of this structure. As intervention, early debridement (either open or arthroscopically) is recommended.
However, once the patella tendon contracture has become permanent, arthroscopic treatment is known to be less successful and more complicated.5) The literature on the treatment of delayed stages of patella infera is limited.8,9) Lengthening of the patella tendon, osteotomy of the tibial tuberosity and patellectomy has been described in such cases, with variable results.8) Paulos et al.8) reviewed 75 patients with the infrapatella contracture syndrome. The patients were treated with an open soft tissue debridement or, when the tendon was short by >8 mm, with a proximal transfer of the tibial tuberosity. They noted more improvement of knee joint motion than of function.
As presented in this report, arthroscopic surgery for delayed patella infera demonstrated reasonable outcome. Arthroscopic procedures include thorough debridement of fibrotic tissues and additional further release of tibial insertion site of patella tendon. Postoperative rehabilitation is another major factor contributing to the outcome. The patient in this case underwent a modified postoperative rehabilitation program as reported by Shelbourne and Nitz.10) This program included ROM exercises which were started immediately after surgery (range, 0-90 flexion), and walking with full weight-bearing was permitted immediately after surgery as tolerated. Weight room activities, including leg press, quarter squats, calf raise, and stationary bicycling were started 2 to 3 weeks after surgery. The accelerated rehabilitation therapy at postoperative period may have affected the remaining contracted patella tendon resulting in partial lengthening (Fig. 4). In conclusion, arthroscopic treatments and accelerated rehabilitation therapy may be beneficial even on delayed patella infera cases.
Figures and Tables
Figure 1
Preoperative radiographs. Patella infera is shown at 7, 8 months after initial trauma. (A) Initial radiograph showing a minimally displaced transverse fracture at the inferior pole of the patella. (B) Post-trauma 5 month radiograph showing progression of union without patella infera. (C) Post-trauma 7 months, and (D) 8 months after trauma.

Figure 2
Hypertrophied soft tissue (white arrows) extending from the retropatella fat pad area to the medial retinaculum was observed on preoperative magnetic resonance imaging. Thickened patella tendon with signal change (arrowheads) was also identifiable. (A) Axial T2 proton density fat suppression images. (B) Saggital T2 fat suppression images.
References
1. Conner AN. The treatment of flexion contractures of the knee in poliomyelitis. J Bone Joint Surg Br. 1970; 52:138–144.

2. Mingo-Robinet J, Castañeda-Cabrero C, Alvarez V, León Alonso-Cortés JM, Monge-Casares E. Tourniquet-related iatrogenic femoral nerve palsy after knee surgery: case report and review of the literature. Case Rep Orthop. 2013; 2013:368290.

3. Mariani PP, Del Signore S, Perugia L. Early development of patella infera after knee fractures. Knee Surg Sports Traumatol Arthrosc. 1994; 2:166–169.

4. Hantes ME, Zachos VC, Bargiotas KA, Basdekis GK, Karantanas AH, Malizos KN. Patellar tendon length after anterior cruciate ligament reconstruction: a comparative magnetic resonance imaging study between patellar and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2007; 15:712–719.

5. Noyes FR, Wojtys EM, Marshall MT. The early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop Relat Res. 1991; 265:241–252.

6. Okamoto R, Koshino T, Morii T. Shortening of patellar ligament and patella baja with improvement of quadriceps muscle strength after high tibial osteotomy. Bull Hosp Jt Dis. 1993; 53:21–24.
7. Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am. 1989; 71:245–248.

8. Paulos LE, Wnorowski DC, Greenwald AE. Infrapatellar contracture syndrome. Diagnosis, treatment, and long-term followup. Am J Sports Med. 1994; 22:440–449.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download