Abstract
Purpose
Using magnetic resonance imaging (MRI) as the standard of reference, the purpose of this study was to evaluate the accuracy of sonoelastography (SE) for assessment of fatty degeneration of suprasupinatus (SSP).
Materials and Methods
A retrospective analysis was conducted in 131 shoulders of 126 consecutive patients who underwent shoulder MRI, and SE. Oblique sagittal images of SSP were obtained using SE; the SE images were evaluated by two orthopedic surgeons using a 256 degree color map image.
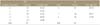
Results
When the supraspinatus fatty degenerations were based on MRI findings, the sensitivity of SE was 89.47%, specificity 92.85%, and accuracy 91.60%. The interobserver reliability of the SE findings was 'almost perfect agreement' with a weighted kappa coefficient of 0.81. By comparison of MRI with the SE findings, the grades of MRI and SE showed positive correlation (r=0.85, p≤0.001). In addition, the occupation ratio and blue region area ratio also showed positive correlation (r=0.69, p≤0.001).
Figures and Tables
Figure 1
T1-weighted oblique sagittal magnetic resonance image shows the method of calculation of the occupation ratio of supraspinatus muscle. Occupation ratio=actual occupied area (B)/estimated anatomical area (A) ×100. Solid lines indicate suprascapular fossa. Dotted lines indicate supraspinatus.
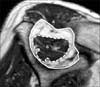
Figure 2
Photograph shows the investigation of the supraspinatus muscle belly. The transducer was perpendicular to the central tendon of the muscle belly of the supraspinatus muscle; this plane corresponded to the oblique sagittal magnetic resonance imaging plane.

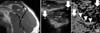
Figure 3
Blue region area ratio=total surface area of blue regions (B)/total surface area in desired region (A) ×100. Solid lines indicate suprascapular fossa. Dotted lines indicate total surface area of blue regions. Subcu, subcutaneous tissue; TR, trapezius.

Figure 4
(A) T1-weighted oblique sagittal image of magnetic resonance images of grade 1 supraspinatus fatty degeneration shows some fatty streaks. (B) Oblique sagittal view of the sonoelasticography of grade 0 supraspinatus fatty degeneration shows an absolute dominant blue region (a few focal lesions) in the elasticity image. Solid lines indicate suprascapular fossa. Subcu, subcutaneous tissue; TR, trapezius; SSP, supraspinatus.

Figure 5
(A) T1-weighted oblique sagittal image of magnetic resonance images of grade 4 supraspinatus fatty degeneration shows that fat is more extensive than the muscle. (B) Oblique sagittal view of the sonoelasticography of grade 2 supraspinatus fatty degeneration shows a non-dominant blue region (≤1/2 of desired region) in the elasticity image. Solid lines indicate suprascapular fossa. Dotted lines indicate supraspinatus. Subcu, subcutaneous tissue; TR, trapezius; SSP, supraspinatus.

Figure 6
(A) T1-weighted oblique sagittal image of magnetic resonance images of grade 1 supraspinatus fatty degeneration shows some fatty streaks. (B) Oblique sagittal view of the sonoelasticography; arrows indicate posterior acoustic shadowing of the superior border and the spine of the scapula; arrowheads indicate a low echogenecity signal around the scapula by the reaction force of the scapula. TR, trapezius; SSP, supraspinatus; SU, superior border of scapula; SP, spine of scapula.
References
1. Goutallier D, Postel JM, Lavau L, Bernageau J. Impact of fatty degeneration of the suparspinatus and infraspinatus msucles on the prognosis of surgical repair of the rotator cuff. Rev Chir Orthop Reparatrice Appar Mot. 1999; 85:668–676.
2. Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003; 12:550–554.

3. Melis B, DeFranco MJ, Chuinard C, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res. 2010; 468:1498–1505.

4. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994; 304:78–83.
5. Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol. 1998; 33:163–170.

6. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999; 8:599–605.

7. Wiener SN, Seitz WH Jr. Sonography of the shoulder in patients with tears of the rotator cuff: accuracy and value for selecting surgical options. AJR Am J Roentgenol. 1993; 160:103–107.

8. Nakajima D, Yamamoto A, Kobayashi T, et al. The effects of rotator cuff tears, including shoulders without pain, on activities of daily living in the general population. J Orthop Sci. 2012; 17:136–140.

9. Strobel K, Hodler J, Meyer DC, Pfirrmann CW, Pirkl C, Zanetti M. Fatty atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology. 2005; 237:584–589.

10. Varghese T, Ophir J, Konofagou E, Kallel F, Righetti R. Tradeoffs in elastographic imaging. Ultrason Imaging. 2001; 23:216–248.

11. Ophir J, Céspedes I, Ponnekanti H, Yazdi Y, Li X. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging. 1991; 13:111–134.

12. Pesavento A, Perrey C, Krueger M, Ermert H. A time-efficient and accurate strain estimation concept for ultrasonic elastography using iterative phase zero estimation. IEEE Trans Ultrason Ferroelectr Freq Control. 1999; 46:1057–1067.

13. Tsutsumi M, Miyagawa T, Matsumura T, et al. The impact of real-time tissue elasticity imaging (elastography) on the detection of prostate cancer: clinicopathological analysis. Int J Clin Oncol. 2007; 12:250–255.

14. Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996; 67:264–268.

15. Schaefer O, Winterer J, Lohrmann C, Laubenberger J, Reichelt A, Langer M. Magnetic resonance imaging for supraspinatus muscle atrophy after cuff repair. Clin Orthop Relat Res. 2002; 403:93–99.

16. Zanetti M, Hodler J. Imaging of degenerative and posttraumatic disease in the shoulder joint with ultrasound. Eur J Radiol. 2000; 35:119–125.

17. Frey H. Realtime elastography. A new ultrasound procedure for the reconstruction of tissue elasticity. Radiologe. 2003; 43:850–855.
18. De Zordo T, Lill SR, Fink C, et al. Real-time sonoelastography of lateral epicondylitis: comparison of findings between patients and healthy volunteers. AJR Am J Roentgenol. 2009; 193:180–185.

19. Li YY, Wang XM, Zhang YX, Ou GC. Ultrasonic elastography in clinical quantitative assessment of fatty liver. World J Gastroenterol. 2010; 16:4733–4737.

20. Wall LB, Teefey SA, Middleton WD, et al. Diagnostic performance and reliability of ultrasonography for fatty degeneration of the rotator cuff muscles. J Bone Joint Surg Am. 2012; 94:e83.

22. Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008; 190:1105–1111.

23. Chung SW, Kim SH, Tae SK, Yoon JP, Choi JA, Oh JH. Is the supraspinatus muscle atrophy truly irreversible after surgical repair of rotator cuff tears? Clin Orthop Surg. 2013; 5:55–65.

24. Botar-Jid C, Damian L, Dudea SM, Vasilescu D, Rednic S, Badea R. The contribution of ultrasonography and sonoelastography in assessment of myositis. Med Ultrason. 2010; 12:120–126.
25. Moon WK, Chang SC, Huang CS, Chang RF. Breast tumor classification using fuzzy clustering for breast elastography. Ultrasound Med Biol. 2011; 37:700–708.

26. Park SH, Kim SJ, Kim EK, Kim MJ, Son EJ, Kwak JY. Interobserver agreement in assessing the sonographic and elastographic features of malignant thyroid nodules. AJR Am J Roentgenol. 2009; 193:W416–W423.

27. Yoon JH, Kim MH, Kim EK, Moon HJ, Kwak JY, Kim MJ. Interobserver variability of ultrasound elastography: how it affects the diagnosis of breast lesions. AJR Am J Roentgenol. 2011; 196:730–736.

28. Calvete AC, Rodríguez JM, de Dios Berná-Mestre J, Ríos A, Abellán-Rivero D, Reus M. Interobserver agreement for thyroid elastography: value of the quality factor. J Ultrasound Med. 2013; 32:495–504.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download