Abstract
Purpose
Spinal fusion surgery can be associated with significant blood loss, often requiring blood transfusion. The objective of this retrospective study was to evaluate the efficacy of tranexamic acid in reducing blood loss and transfusion after lumbar spinal fusion.
Materials and Methods
A total of 75 consecutive patients undergoing spinal fusion surgery for spinal stenosis were included in this study. Thirty-five patients who were administered tranexamic acid were compared with 40 patients who did not receive the drug. Blood loss through drain, amount of blood transfusion, and hematological laboratory findings were evaluated.
Results
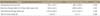
Blood loss through drain for the first 24 hours after surgery was 548.6±192.1 ml in the tranexamic acid group and 1,089.8±368.3 ml in the control group with a significant difference (p=0.001). Total blood loss through drain was 1,010.5±452.5 ml in the tranexamic acid group and 1,512.7±427.8 ml in the control group with a significant difference (p=0.005). Time to removal of drains after surgery was not different, 2.6±0.8 days in the tranexamic acid group and 2.5±1.1 days in the control group (p=0.885). Packed red blood cell (RBC) transfusion for the postoperative period and the number of patients requiring transfusion was significantly lower in the tranexamic acid group than in the control group. A prolongation of protrombin time was observed in the control group on first postoperative day. There were no complications related to the use of tranexamic acid.
References
1. Cho KJ, Suk SI, Park SR, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2007; 32:2232–2237.

2. Kang SB, Cho KJ, Moon KH, Jung JH, Jung SJ. Does low-dose aspirin increase blood loss after spinal fusion surgery? Spine J. 2011; 11:303–307.

3. Guay J, Reinberg C, Poitras B, et al. A trial of desmopressin to reduce blood loss in patients undergoing spinal fusion for idiopathic scoliosis. Anesth Analg. 1992; 75:405–410.

4. Murray DJ, Pennell BJ, Weinstein SL, Olson JD. Packed red cells in acute blood loss: dilutional coagulopathy as a cause of surgical bleeding. Anesth Analg. 1995; 80:336–342.
5. Behrman MJ, Keim HA. Perioperative red blood cell salvage in spine surgery A prospective analysis. Clin Orthop Relat Res. 1992; 278:51–57.
6. Bidstrup BP, Royston D, Sapsford RN, Taylor KM. Reduction in blood loss and blood use after cardiopulmonary bypass with high dose aprotinin (Trasylol). J Thorac Cardiovasc Surg. 1989; 97:364–372.

7. Chareancholvanich K, Siriwattanasakul P, Narkbunnam R, Pornrattanamaneewong C. Temporary clamping of drain combined with tranexamic acid reduce blood loss after total knee arthroplasty: a prospective randomized controlled trial. BMC Musculoskelet Disord. 2012; 13:124.

8. Ekbäck G, Axelsson K, Ryttberg L, et al. Tranexamic acid reduces blood loss in total hip replacement surgery. Anesth Analg. 2000; 91:1124–1130.

9. Woo KS, Tse LK, Woo JL, Vallance-Owen J. Massive pulmonary thromboembolism after tranexamic acid antifibrinolytic therapy. Br J Clin Pract. 1989; 43:465–466.
10. Endo Y, Nishimura S, Miura A. Deep-vein thrombosis induced by tranexamic acid in idiopathic thrombocytopenic purpura. JAMA. 1988; 259:3561–3562.

11. Rydin E, Lundberg PO. Letter: tranexamic acid and intracranial thrombosis. Lancet. 1976; 2:49.
12. Mandal AKJ, Missouris CG. Tranexamic acid and acute myocardial infarction. Br J Cardiol. 2005; 12:306–307.
13. Taparia M, Cordingley FT, Leahy MF. Pulmonary embolism associated with tranexamic acid in severe acquired haemophilia. Eur J Haematol. 2002; 68:307–309.

14. Demirjian Z, Sara M, Stulberg D, Harris WH. Disseminated intravascular coagulation in patients undergoing orthopedic surgery. Clin Orthop Relat Res. 1974; 102:174–180.

15. Mayer PJ, Gehlsen JA. Coagulopathies associated with major spinal surgery. Clin Orthop Relat Res. 1989; 245:83–88.

16. Bux J. Transfusion-related acute lung injury (TRALI): a serious adverse event of blood transfusion. Vox Sang. 2005; 89:1–10.

17. Park HG, Yoo BH, Lee SS, Yon JH, Hong KH. The effect of low dose aprotinin in patients with adolescent idiopathic scoliosis undergoing posterior spinal fusion. Anesth Pain Med. 2008; 3:178–182.
18. Okubadejo GO, Bridwell KH, Lenke LG, et al. Aprotinin may decrease blood loss in complex adult spinal deformity surgery, but it may also increase the risk of acute renal failure. Spine (Phila Pa 1976). 2007; 32:2265–2271.

19. Shapiro F, Zurakowski D, Sethna NF. Tranexamic acid diminishes intraoperative blood loss and transfusion in spinal fusions for duchenne muscular dystrophy scoliosis. Spine (Phila Pa 1976). 2007; 32:2278–2283.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download