Abstract
Purpose
The aim of this study is to analyze the fusion rate according to the mixture ratio and the amount of bone graft in minimally invasive transforaminal lumbar interbody fusion (MI-TLIF).
Materials and Methods
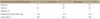
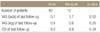
This study included 92 subjects who underwent MI-TLIF. Patients were classified into either group I, in which patients received transplantation with only autogenous bone, group II, in which patients received transplantation with hydroxyapatite mixed with autogenous bone by more than 50%, or group III, in which patients received transplantation with hydroxyapatite mixed with autogenous bone by less than 50%. For analysis of the correlation of amount of bone graft with fusion rate, patients were divided into group A, having less than 12 ml of bone graft, and group B, having more than 12 ml of bone graft. Visual analogue scale and Oswestry disability index were used for clinical assessment, and Burkus' classification method was used for evaluation of bone fusion.
Results
Fusion rates of groups I, II, and III according to the mixture ratio were 90.9%, 86.5%, and 86.2%, respectively. The fusion rate increased as the autobone ratio became higher; however, no significant difference was found (p=0.16). The fusion rates were 81.5% and 92.5% in group A and group B, respectively, which were classified according to the volume of bone graft, showing a significant increase in groups with bone graft volume more than 12 ml (p=0.03).
Figures and Tables
 | Figure 1(A) Autogenous local bone and hydroxyapatite (5 ml). (B) First, a cage was filled with autogeneous local bone, and interbody space was filled with the remaining mixture of autogenous local bone and hydroxyapatite. |
 | Figure 2Radiograph and computed tomography of a case of definitely solid fusion (Grade I). (A) No motion on flexion-extension radiographs. (B) Continuous bony incorporation within and around the cage and new bone formation adjacent to the cage. |
 | Figure 3Radiograph and computed tomography of a case that was probably not solid fusion (Grade III). (A) No motion on flexion-extension radiographs. (B) Non continuous bony incorporation within and around the cage and new bone formation adjacent to the cage. |
References
1. Isaacs RE, Podichetty VK, Santiago P, et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005; 3:98–105.

2. Mummaneni PV, Rodts GE Jr. The mini-open transforaminal lumbar interbody fusion. Neurosurgery. 2005; 57:256–261.

3. Park P, Foley KT. Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis: technique and outcomes after a minimum of 2 years' follow-up. Neurosurg Focus. 2008; 25:E16.

4. Park Y, Ha JW, Lee YT, Sung NY. The effect of a radiographic solid fusion on clinical outcomes after minimally invasive transforaminal lumbar interbody fusion. Spine J. 2011; 11:205–212.

5. Aspenberg P, Albrektsson T, Thorngren KG. Local application of growth-factor IGF-1 to healing bone. Experiments with a titanium chamber in rabbits. Acta Orthop Scand. 1989; 60:607–610.

6. Cook SD, Dalton JE, Tan EH, Whitecloud TS 3rd, Rueger DC. In vivo evaluation of recombinant human osteogenic protein (rhOP-1) implants as a bone graft substitute for spinal fusions. Spine (Phila Pa 1976). 1994; 19:1655–1663.

7. Cook SD, Dalton JE, Prewett AB, Whitecloud TS 3rd. In vivo evaluation of demineralized bone matrix as a bone graft substitute for posterior spinal fusion. Spine (Phila Pa 1976). 1995; 20:877–886.

8. Louis-Ugbo J, Murakami H, Kim HS, Minamide A, Boden SD. Evidence of osteoinduction by Grafton demineralized bone matrix in nonhuman primate spinal fusion. Spine (Phila Pa 1976). 2004; 29:360–366.

9. Martin GJ Jr, Boden SD, Titus L, Scarborough NL. New formulations of demineralized bone matrix as a more effective graft alternative in experimental posterolateral lumbar spine arthrodesis. Spine (Phila Pa 1976). 1999; 24:637–645.

10. Choi DJ, Ahn DK, Lee S, et al. The effect of demineralized bone matrix as a graft enhancer in posterior lumbar interbody fusion using cage and local bone chips. J Korean Soc Spine Surg. 2008; 15:157–164.

11. Spivak JM, Hasharoni A. Use of hydroxyapatite in spine surgery. Eur Spine J. 2001; 10:Suppl 2. S197–S204.

12. Chung JY, Chang BS, Lee CK, et al. Posterior lumbar interbody fusion using hydroxyapatite block -comparison with metal and PEEK cages-. J Korean Soc Spine Surg. 2009; 16:243–250.
13. Burkus JK, Foley K, Haid RW, LeHuec JC. Surgical Interbody Research Group--radiographic assessment of interbody fusion devices: fusion criteria for anterior lumbar interbody surgery. Neurosurg Focus. 2001; 10:E11.

14. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976). 2003; 28:S26–S35.

15. Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005; 18:Suppl. S1–S6.
16. Isaacs RE, Podichetty VK, Santiago P, et al. Minimally invasive microendoscopy-assisted transforaminal lumbar interbody fusion with instrumentation. J Neurosurg Spine. 2005; 3:98–105.

17. Hwang C, Bae JY, Koo KH, et al. A comparative experimental study of allograft and porous hydroxyapatite as bone substitutes. J Korean Orthop Assoc. 2007; 42:545–552.

18. Thalgott JS, Giuffre JM, Fritts K, Timlin M, Klezl Z. Instrumented posterolateral lumbar fusion using coralline hydroxyapatite with or without demineralized bone matrix, as an adjunct to autologous bone. Spine J. 2001; 1:131–137.

19. Finkemeier CG. Bone-grafting and bone-graft substitutes. J Bone Joint Surg Am. 2002; 84:454–464.

20. Sartoris DJ, Gershuni DH, Akeson WH, Holmes RE, Resnick D. Coralline hydroxyapatite bone graft substitutes: preliminary report of radiographic evaluation. Radiology. 1986; 159:133–137.

21. Cheong US, Kim DY, Cho JL, Kim YH, Park YS. Comparison of the effect of hydroxyapatite and allogeneous bone as an adjunct to autogenous iliac bone grafting in posterolateral spinal fusion. J Korean Orthop Assoc. 2008; 43:347–352.
22. Kang HJ, Kim TK, Kweon SH, Shim DM, Lee SI. The usefulness of hydroxyapatite bone transplantation in treatment of metaphyseal fracture with bone defect. J Korean Musculoskelet Transplant Soc. 2011; 11:36–41.
23. Korovessis P, Koureas G, Zacharatos S, Papazisis Z, Lambiris E. Correlative radiological, self-assessment and clinical analysis of evolution in instrumented dorsal and lateral fusion for degenerative lumbar spine disease. Autograft versus coralline hydroxyapatite. Eur Spine J. 2005; 14:630–638.

24. Bucholz RW. Nonallograft osteoconductive bone graft substitutes. Clin Orthop Relat Res. 2002; 395:44–52.

25. Boden SD, Martin GJ Jr, Morone M, Ugbo JL, Titus L, Hutton WC. The use of coralline hydroxyapatite with bone marrow, autogenous bone graft, or osteoinductive bone protein extract for posterolateral lumbar spine fusion. Spine (Phila Pa 1976). 1999; 24:320–327.

26. Gocmen-Mas N, Karabekir H, Ertekin T, Edizer M, Canan Y, Duyar I. Evaluation of lumbar vertebral body and disc: a stereological morphometric study. Int J Morphol. 2010; 28:841–847.

27. Pfirrmann CW, Metzdorf A, Elfering A, Hodler J, Boos N. Effect of aging and degeneration on disc volume and shape: A quantitative study in asymptomatic volunteers. J Orthop Res. 2006; 24:1086–1094.

28. Riouallon G, Lachaniette CH, Poignard A, Allain J. Outcomes of anterior lumbar interbody fusion in low-grade isthmic spondylolisthesis in adults: a continuous series of 65 cases with an average follow-up of 6.6 years. Orthop Traumatol Surg Res. 2013; 99:155–161.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download