Abstract
Purpose
To document post-excision recurrence rates for epidermal cysts of the foot and ankle by location.
Materials and Methods
The authors retrospectively reviewed epidermal cysts confirmed histologically by excisional biopsy in 37 patients (male 20, female 17) from 2004 to 2011. Cyst locations and sizes were analyzed and preoperative and postoperative pain levels were compared using a visual analogue scale (VAS). Rates of recurrence and patient satisfaction levels were also measured.
Results
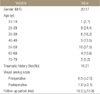
Epidermal cysts occurred most commonly on the 1st toe (15 cases, 40.6%), followed by the ankle (7 cases, 18.9%), 2nd toe (6 cases, 16.2%), 3rd toe (4 cases, 10.8%), 4th toe (1 case, 2.7%), 5th toe (2 cases, 5.4%), and heel (2 cases, 5.4%). Average cyst size in 35 cases was 15.5×15.0×7.9 mm. VAS reduced from 6.5 preoperatively to 1.0 postoperatively. Cysts recurred in 7 cases (18.9%); on the 1st toe in 5 and on the 2nd toe in 2. Thirty patients (81.0%) were very satisfied with treatment results, 2 patients (5.4%) were satisfied, and 5 (13.5%) were not satisfied. Recurrence occurred in 4 cases, and in one of these cases the cyst recurred after second excision.
Figures and Tables
 | Figure 1Picture showing a hyperkeratotic dome-shaped protruding epidermal cyst on a left sole. This patient had a chief complaint of a painful plantar mass. |
 | Figure 2Zones of the foot used for analysis by Kirby et al.4) Epidermal cysts were located in zones 1, 2, 3, 4, and 5 in 7, 2, 0, 9, and 19 cases, respectively. |
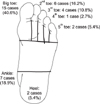 | Figure 3Distribution of epidermal cysts categorized by digit number, heel, and ankle. The most common location was the great toe, including first-second web space. |
 | Figure 4Photograph of a cyst of the great toe (Kirby's zone 5) in a 53-year-old woman. The cyst was treated by excision but recurred 6 months later. |
 | Figure 5Ultrasonographic findings (A) showing a well-defined hypoechoic mass with a smooth margin. The 24×27×29 mm sized, well-defined, soft tissue mass was located in the plantar subcutaneous layer. The central portion of the mass demonstrated intermediate signal intensity by T1-weighted imaging (C), low signal intensity by T2-weighted imaging (D), and a high signal intensity at its periphery by T1 and T2-weighted imaging. Enhanced sagittal magnetic resonance image showed epidermal wall enhancement (B). |
References
1. Silver SG, Ho VCG. Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Benign epithelial tumors. Fizpatrick's dermatology in general medicine. 2004. 6th ed. New York: Mcgrow-Hill;778–779.
2. Mihara M, Nishiura S, Aso M, Shimao S, Nakakuki S. Papillomavirus-infected keratinous cyst on the sole. A histologic, immunohistochemical, and electron microscopic study. Am J Dermatopathol. 1991. 13:293–299.
3. Shin DS, Park SH, Ahn JC. Tumors of the foot. J Korean Bone Joint Tumor Soc. 2003. 9:69–76.
4. Kirby EJ, Shereff MJ, Lewis MM. Soft-tissue tumors and tumor-like lesions of the foot. An analysis of eighty-three cases. J Bone Joint Surg Am. 1989. 71:621–626.

5. Lever WF, Schaumburg-Lever G. Histopathology of the skin. 1990. 7th ed. Philadephia: Lippincott;535–536.
6. Jun JH, Lee SJ, Jang YH, Lee WJ, Kim DW, Lee JH. A clinical and radiological study on 31 palmoplantar epidermal cysts. Korean J Dermatol. 2011. 49:707–713.
7. Cho HM, Kim SN. A clinical and histopathological study of 324 cases of epidermal cyst. Korean J Dermatol. 2007. 45:242–248.
8. Chung J, Ahn SK, Lee SH, Lee WS. Comparative histopathologic and immunohistochemical studies of epidermal cysts of palm & sole, other epidermal cysts and pilar cysts. Korean J Dermatol. 1994. 32:853–859.
9. Bolognia J, Jorizzo JL, Rapini RP, et al. Dermatology. 2008. 2nd ed. Missouri: Mosby Elsevier;1681–1683.
10. Shin KH, Park HJ, Kim JM, Hahn SB, Kang ES. Tumors of the foot and ankle. J Korean Bone Joint Tumor Soc. 2000. 6:69–76.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download