Abstract
Malignant vascular tumors (angiosarcoma) of bone are rare and represent a less than 1% of malignant bone tumors. The authors report a case of a patient with angiosarcoma misdiagnosed as infection, which developed adjacent to a stainless steel intra-medullary nail used for fixation of a femur fracture.
Angiosarcoma is an uncommon neoplasm characterized by rapidly proliferating extensively infiltrating anaplastic cells derived from blood vessels and lining irregular blood-filled spaces. Primary angiosarcoma arising in bone is rare, and accounts for less than 1% of malignant bone tumors.1) Even though the prognosis of angiosarcoma is mainly related to the pathologic characteristics of the sarcoma itself, delayed diagnosis and misdiagnosis as other diseases worsening illness. This report presents the case of an angiosarcoma of the distal femur around an intramedullary nail that was misdiagnosed as an infection. We would like to call attention to other orthopaedic doctors that although angiosarcoma around an intramedullary nail is rare, accurate and timely diagnosis is very essential for the treatment.
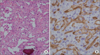
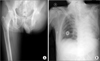
A 62-year-old man visited our outpatient clinic with complaints of pain and heat sensation in the distal thigh. The patient was not able to stand due to pain and complained of moderate resting pain and hardness to raise the affected leg or flex the affected knee. The patient remarked that the symptoms had worsened despite a prior visit to a private clinic and conservative treatment. A physical examination revealed no obvious cause despite tenderness and the local heat sensation in the distal thigh, and no palpable mass. The past history showed nothing significant in medicine or surgery. Sixteen years earlier, however, the patient had sustained a open femoral shaft fracture that was internally fixed with a stainless steel intra-medullary nail (Russell-Taylor interlocking intramedullary Nail System; Smith and Nephew, Memphis, TN, USA). This fracture had healed uneventfully, and the limb functioned well until 3 months before the current presentation when the patient complained of pain at the distal thigh. Due to the development of pain, the patient was evaluated by plain radiography, computed tomography (CT, without enhancement), and serologic study. Regretfully, a magnetic resonance imaging (MRI) could not be performed because the device was stainless steel. Simple radiograph revealed multiple moth-eaten pattern of bone destruction in the anterior, medial and lateral areas of the distal part of the intramedullary nail (Fig. 1A). CT revealed that the localized bony destruction in both cortical and cancellous bones at the distal part of intramedullary nail was multiple and well- marginated, but no sclerotic rim, mass formation or periosteal reaction was evident (Fig. 1B). Hematologic studies were unexceptional, except for increased erythrocyte sedimentation rate (ESR) value of 58 m/hr and a C-reactive protein (CRP) concentration of 8.2 mg/L. Non-steroidal anti-inflammatory drugs or antibiotics were not administrated preoperatively. To rule out tumorous condition, infection or osteolysis related to loosening of orthopedic prosthesis, preoperative whole body work-up should have been done, but we assumed that the cause was an infection with scant attention owing to extremely low rate of malignancy around an intramedullary nail, an operation history for an open fracture, local heatness and pain and elevated ESR and CRP. Eventually, we operated to treat the infection. Initially, the distal screws were removed via mini-open incision and the intramedullary nail was removed via another proximal incision. Then, an additional incision was made into the distal femur, which was considered the infection focus, and the tissue around the distal femur was debrided and thoroughly irrigated. However, we did not find any obvious visible signs of infection, as had been anticipated. Instead, macroscopic, light brown-colored soft granulation tissue was observed spreading into the intramedullary space, the volume of removed granulation tissue was about the size of a chestnut. Considering this, we should have done a biopsy to rule out any malignancy. But, we presumed it was a low-grade infection without significant attention, and so only an ordinary swab culture was performed. We meticulously cleaned the intramedullary space and did not have to have the distal femur fixed using any devices because there was no pseudomotion or instability in the distal femur. Finally, we closed the surgical site. Postoperatively, the patient wore a long leg cast to prevent secondary fracture and the surgical wound was cared for via an open cast. On postoperative day 14, rapid bone lysis was observed by regular follow-up radiograph. A physical examination revealed pseudoarthrois at the operation site (Fig. 2A). Although no bacteria were identified in the primary culture, a decision was made to re-operate. However, no sign of infection was evident in the second operative field, but substantial progressive bony lysis of the cortex and markedly more extensive brown-colored granulation soft tissue was evident as compared with the previous surgery. Unfortunately, frozen biopsy was not possible. Instead, we harvested some tissues for biopsy. Antibiotic beads were inserted in the distal femur, and the femur was externally fixed to prevent any further progression of the pseudoarthrosis (Fig. 2B). Biopsy of the mass revealed a high-grade vascular lesion and histologic examination returned a diagnosis of high-grade angiosarcoma. Histologically, the tumor was composed of small nests of large epitheloid cells, and the majority of the cells were polygonal with eosinophilic cytoplasm with pale nuclei with prominent nucleoli. Numerous abnormal mitotic cells with cellular pleomorphism were observed. In certain areas, dilated and anastomotic vascular spaces adjacent to solid growth were present. Blood-filled channels were lined with epitheloid tumor cells. Stroma consisted mainly of thin fibrovascular connective tissue. Extensive hemorrhage, necrosis, and cystic changes were evident. Immunohistochemistry revealed CD 34 positivity, which suggested an endothelioid-related origin of the tumor (Fig. 3). The patient was transferred to an advanced medical institution, Consequently, disarticulation of the hip was performed 2 weeks later from the last operation (Fig. 4A), and three courses of chemotherapy including isosfamide 2500 mg/m2, mesna 2500 mg/m2, and adriamycin 60 mg/m2 were started. The patient was followed-up for 3 years. However, 41 months after the last surgery, he admitted to an emergency room complaining of fever and dyspnea and he was diagnosed with pneumonia. Even though he was treated with conservative treatment for the disease, he finally expired 10 days after the admission (Fig. 4B).
The term angiosarcoma refers to malignant vascular tumors that have many functional and morphologic features of normal endothelium, and is used for all sarcomas showing endothelial differentiation. 2) Approximately 6% of all angiosarcomas are found in bone.2)
Primary angiosarcoma in bone is rare, and accounts for less than 1% of malignant bone tumors.1) The bones of the lower limbs, particularly the femur and tibia, are most commonly involved, followed by the pelvis, vertebral column, and bones of the upper limbs.3) However, primary angiosarcoma around an orthopedic device is very rare. The development of cancer in association with metallic implants is well recognized but poorly understood. Fortunately, its occurrence is rare considering the number of orthopedic implants being used. A number of criteria must be met for the differential diagnosis of metal-associated sarcoma. First, the tumor should be in the direct vicinity of a metallic implant in bone or soft tissue, which excludes lesions that occur in the general region of the implant or in a more distant in the same extremity. Second, the tumor should develop after a latency of around 2 years or more, as a tumor identified within 1 year of placement of an implant in all likelihood was present before surgery at an unrecognizable stage. Third, there should be no other obvious, well-recognized factor predisposing the development of a secondary malignancy, such as, radiation or chronic infection.4) With regard to these criteria, our case raises an interesting point. We cannot conclude that the angiosarcoma was directly aroused from the metallic implant, however, we had difficulty in detecting it earlier thorough examination due to factors including metal artifact. It is interesting that the angiosarcoma arised from the supracondylar area, which was far from the shaft of the distal femur that was fractured previously.
Even though the most common location of occurrence of angiosarcoma is a femur regardless of the insertion of metal device, we think that implies the relationship between metal and angiosarcoma might be possible.
Additionally, at the initial visit to clinic and primary surgery, we overlooked the possibility of malignancy without sufficient attention, which delayed appropriate diagnosis and treatment. With an inappropriate procedure, the margin of the tumor was disrupted and the cells of angiosarcoma might have infiltrated to vicinity via surrounding soft tissues and vessels. It could have helped it progress rapidly.
Clinically, angiosarcoma presents with pain and swelling, especially when the affected bone is superficial, or as an enlarging mass (most are smaller than 5 cm), and pathological fractures occur in nearly 10% of patients.5) The initial clinical appearance of angiosarcoma can mimic infection, bruising, a soft tissue mass, or a vascular lesion,6) and diagnosis can be difficult because of the tumor's variable expression of epithelioid features. In our case, no palpable mass was evident and the patient presented with pain and a sensation of heat, which we misdiagnosed as infection. Consequently the diagnosis of angiosarcoma was delayed. A combination of this fever with pain, abnormal selologic findings and an inconclusive radiograph led to a suspicion of infectious disease, such as osteomyelitis, which has been reported.7,8) This initial misdiagnosis delayed correct treatment.
On radiological studies, angiosarcoma of bone is generally a nonspecific and malignant-appearing lesion with ill-defined borders.3,9) A permeative and destructive pattern may also be seen. Given the degree of bone destruction caused by the tumor. Periosteal reaction and pathologic fractures are relatively uncommon.9) Some lesions may exhibit a mixed lytic and sclerotic pattern, but purely sclerotic lesions are rare. CT and MRI are useful in determining the extent of the lesion and soft tissue involvement. We were inconvenienced by not performing detailed radiological examinations, owing to the device made of stainless steel, such as enhanced CT or MRI, and by not scrutinizing radiologic findings. Regretfully, we jumped to the conclusion that the symptoms and the radiologic findings of multiple lytic lesions indicated infection, which delayed a definitive diagnosis and appropriate treatment. On reflection, we should have included infection, a primary tumor, and even a metastatic tumor in the initial differential diagnosis.
Histologically, angiosarcoma of bone has an aggressive and variable appearance. Solid cellular sheets and spindling of the cells may be seen. Large, pleomorphic nuclei with clumped chromatin are common, as are frequent and atypical mitoses and necrosis.10) Other histologic signs include anastomotic vascular channels with reticulum staining, proliferating endothelial cells in the basement membrane, the presence of embryonal-like vessels and Weibel-Palade bodies, and positivity for VIII related antigen and Ulex Europeus.3,10)
The differential diagnosis of angiosarcoma includes multiple myeloma and a wide range of carcinomas and sarcomas, and narrowing the diagnosis requires careful clinical and imaging examinations, and, ultimately, biopsy. Furthermore, the treatment of malignant tumors differs significantly from that of benign tumors, and appropriate biopsy and the use of immunohistochemical tests are often required to reach an accurate diagnosis, to stage the disease, and to determine prognosis and treatment. If not recognized and diagnosed early, the opportunity for selecting appropriate treatment is diminished and the prognosis worsens. Therapeutic alternatives for patients with angiosarcoma of bone are similar to those available for patients with other types of bone sarcomas, and involve radical resection or amputation. The role of radiation therapy and chemotherapy in this context is currently being investigated.9)
Malignant tumor in the orthopedic field might not be diagnosed properly because it could not show any specific symptoms until late stage of disease. However, we should bear the possibility of malignant tumor in mind as early diagnosis and proper treatment have a decisive effect on the prognosis.
Figures and Tables
Figure 1
(A) An anteroposterior and lateral radiographs of the left femur show lytic destruction of bone adjacent to intra-medullary nail fixation placed for the femur fracture. (B) Computed tomography revealed that the localized bony destruction in both cortical and cancellous bones around the distal part of intramedullary nail.

Figure 2
(A) Fourteen days after the first operation, pathological femoral fracture and rapid osteolysis has developed. (B) For the pathological fracture, antibiotic beads were inserted in distal femur, and the femur was externally-fixed to prevent any further progress of the pseudarthrosis.

References
1. Unni KK. Dahlin's bone tumors. General aspects and data on 11,087 cases. 1996. 5th ed. Philadelphia: Lippincott-Raven;317–331.
2. Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weeiss's soft tissue tumors. 2001. 4th ed. St. Louis: Mosby;917–954.
3. Hasegawa T, Fujii Y, Seki K, et al. Epithelioid angiosarcoma of bone. Hum Pathol. 1997. 28:985–989.

4. McDonald DJ, Enneking WF, Sundaram M. Metal-associated angiosarcoma of bone: report of two cases and review of the literature. Clin Orthop Relat Res. 2002. (396):206–214.

5. Boutin RD, Spaeth HJ, Mangalik A, Sell JJ. Epithelioid hemangioendothelioma of bone. Skeletal Radiol. 1996. 25:391–395.

6. Lewis JM, Sondak VK. Angiosarcoma an Electronic Sarcoma Update Newsletter(ESUN) article. Liddy Shriver Sarcoma Initiative. 2008. 12. 08. accessed 2010 Aug. Sarcoma LLearning Center;Available from: http://sarcomahelp.org/learning_center/angiosarcoma.html.

7. Durbin M, Randall RL, James M, Sudilovsky D, Zoger S. Ewing's sarcoma masquerading as osteomyelitis. Clin Orthop Relat Res. 1998. (357):176–185.

8. Willis RB, Rozencwaig R. Pediatric osteomyelitis masquerading as skeletal neoplasia. Orthop Clin North Am. 1996. 27:625–634.

9. Wenger DE, Wold LE. Malignant vascular lesions of bone: radiologic and pathologic features. Skeletal Radiol. 2000. 29:619–631.
10. Campanacci M. Campanacci M, Enneking WF, editors. Hemangioendothelioma bengin, heman-gioendothelioma low grade, hemangioendothe lioma high grade (angiosarcoma). Bone and soft tissue tumors. 1999. 2nd ed. New York: Springer-verlag;623–641.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download