Abstract
Chronic granulomatous infection of the skin and soft tissue by nontuberculous mycobacteria in patients with normal immune system is rarely reported. This case was about a child patient, with normal immune system, whose lower leg was lacerated after a slip down in the Philippines and it was previously treated at a hospital in the Philippines. After a couple of surgical debridement of the wound, the cause of the soft tissue infection was found to be a combined infection of nontuberculous mycobacteria and mycobacterium tuberculosis. We present a case that has been rare in Korea, but common overseas.
Figures and Tables
Figure 1
Preoperative photograph shows erythematous swelling with pus-like discharge and wound dehiscence on a lower leg.

Figure 2
The magnetic resonance images show ill defined soft tissue swelling and contrast enhancement at the anteri or subcutaneous tissue of the lower leg, left. But, there was no remarkable finding at the bone and muscle.
Figure 3
The three phase bone scan shows no specific abnormal finding at the wound. RT, right; LT, left; ANT, anterior; POST, posterior.

Figure 4
After adequate excision of the wound, rotational flap was performed for the soft tissue defect.
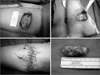
Figure 5
Pathologic findings show mixed chronic granulomatous and acute inflammation in dermis and subcutis (a: ×100, b: ×400, H&E stain, A). There are revealed some acid-fast bacilli (black arrows) within vacuoles (×400, Ziehl-Neelsen stain, B).

References
1. Choi YJ, Lee HJ, Lee KY, Ryu DJ, Lee MG. A case of mycobacterium fortuitum infection at the site of acupuncture. Korean J Dermatol. 2009. 47:755–758.
2. Liao CH, Lai CC, Ding LW, et al. Skin and soft tissue infection caused by non-tuberculous mycobacteria. Int J Tuberc Lung Dis. 2007. 11:96–102.
3. Chen HY, Chen CY, Huang CT, et al. Skin and soft-tissue infection caused by non-tuberculous mycobacteria in Taiwan, 1997-2008. Epidemiol Infect. 2011. 139:121–129.

4. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci. 2005. 20:913–925.

5. Goodhart GL. Mycobacterium fortuitum osteomyelitis following trauma. J Orthop Trauma. 1993. 7:142–145.

6. Devi DR, Indumathi VA, Indira S, Babu PR, Sridharan D, Belwadi MR. Injection site abscess due to Mycobacterium fortuitum: a case report. Indian J Med Microbiol. 2003. 21:133–134.
7. Kim BJ, Lee KH, Park BN, et al. Differentiation of mycobacterial species by PCR-restriction analysis of DNA (342 base pairs) of the RNA polymerase gene (rpoB). J Clin Microbiol. 2001. 39:2102–2109.
8. Brown-Elliott BA, Wallace RJ Jr. Clinical and taxonomic status of pathogenic nonpigmented or late-pigmenting rapidly growing mycobacteria. Clin Microbiol Rev. 2002. 15:716–746.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download