Abstract
Purpose
The purpose of the current study is to evaluate the clinical and radiographic outcomes of primary total hip arthroplasty (THA) using a single titanium tapered stem with alumina bearing, which was performed through a modified direct lateral approach.
Materials and Methods
One hundred twenty consecutive primary THAs were performed in 102 patients, and retrospectively reviewed. There were 53 men and 49 women of mean age 54 years, and all patients were followed for a minimum follow-up period of 5 years (range, 5-8.1 years). Clinical outcomes assessment consisted of calculation of the Harris hip score (HHS), and evaluation of the presence of thigh pain or limp. Sequential radiographs were evaluated for implant migration, osteolysis, reactive line, cortical hypertrophy, or evidence of component loosening.
Results
At the final follow-up, the mean preoperative HHS of 46 points improved to 94 points; and activity-related thigh pain occurred in two hips, and mild limps in four hips. There was no evidence of implant migration, osteolysis, or component loosening. Audible squeaking was present in two hips, without pain and radiographic abnormality. Dislocation occurred in three hips.
Figures and Tables
Figure 1
Modified direct lateral approach. (A) Marking of musculoosseous sleeve composed of the anterior 2/3 of the gluteus medius and minimus, anterior trochanteric fragement, and the anterior 1/3 of vastus lateralis. (B) Osteotomy is oriented in coronal plane. G, gluteus medius; T, greater trochanter; V, vastus lateralis.

Figure 2
(A) Musculoosseous sleeve is reflected anteriorly (asterisk: reflected anterior trochanteric fragment, arrow: gluteus minimus). (B) The anterior joint capsule J is exposed through dissection the interval between the abductors and the capsule.

Figure 3
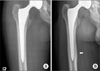
(A) An immediate postoperative radiograph. (B) The radiograph taken 6 years after surgery shows calcar rounding (arrow).

Figure 4
(A) An immediate postoperative radiograph. (B) Distal cortical hypertrophy (arrow) was observed on the radiograph taken 5 years after surgery, which was asymptomatic.
References
1. Engh CA Jr, Claus AM, Hopper RH Jr, Engh CA. Long-term results using the anatomic medullary locking hip prosthesis. Clin Orthop Relat Res. 2001. 393:137–146.

2. Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cementless Zweymüller Alloclassic system. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 2003. 85:296–303.
3. Grant P, Nordsletten L. Total hip arthroplasty with the Lord prosthesis. A long-term follow-up study. J Bone Joint Surg Am. 2004. 86:2636–2641.
4. Dalury DF, Gonzales RA, Adams MJ. Minimum 5-year results in 96 consecutive hips treated with a tapered titanium stem system. J Arthroplasty. 2010. 25:104–107.

5. Hwang BH, Lee WS, Park KK, Yang IH, Han CD. Straight tapered titanium stem with alumina bearing in cementless primary total hip arthroplasty: a minimum 5-year follow-up. J Arthroplasty. 2011. 26:1310–1317.
6. García-Cimbrelo E, Bru-Pomer A, García-Benítez B, Hernández-Blanco M, Vaquero J. Multicentric and prospective study of the Summit cementless stem. Hip Int. 2010. 20:Suppl 7. 63–69. [Epub ahead of print].

7. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993. 14:231–242.

8. Callaghan JJ, Dysart SH, Savory CG. The uncemented porous-coated anatomic total hip prosthesis. Two-year results of a prospective consecutive series. J Bone Joint Surg Am. 1988. 70:337–346.

9. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979. 141:17–27.
10. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973. 55:1629–1632.
11. Barrack RL, Jasty M, Bragdon C, Haire T, Harris WH. Thigh pain despite bone ingrowth into uncemented femoral stems. J Bone Joint Surg Br. 1992. 74:507–510.

12. Campbell AC, Rorabeck CH, Bourne RB, Chess D, Nott L. Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. J Bone Joint Surg Br. 1992. 74:63–66.

13. Katsimihas M, Katsimihas G, Lee MB, Learmonth ID. Distal femoral cortical hypertrophy: predisposing factors and their effect on clinical outcome. Hip Int. 2006. 16:18–22.

14. Herzwurm PJ, Simpson SL, Duffin S, Oswald SG, Ebert FR. Thigh pain and total hip arthroplasty: scintigraphy with 2.5-year followup. Clin Orthop Relat Res. 1997. 336:156–161.

15. Kröger H, Venesmaa P, Jurvelin J, Miettinen H, Suomalainen O, Alhava E. Bone density at the proximal femur after total hip arthroplasty. Clin Orthop Relat Res. 1998. 352:66–74.
16. Karachalios T, Tsatsaronis C, Efraimis G, Papadelis P, Lyritis G, Diakoumopoulos G. The long-term clinical relevance of calcar atrophy caused by stress shielding in total hip arthroplasty: a 10-year, prospective, randomized study. J Arthroplasty. 2004. 19:469–475.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download