Abstract
Spondylodiscitis is very rare complication caused by Klebsiella pneumoniae. Among those, few cases of spondylodiscitis concomitant with epidural abscess due to Klebsiella pneumoniae have been reported. We present a case of lumbar pyogenic spondylodiscitis with epidural abscess caused by Klebsiella pneumoniae that successfully treated with administration of cefotaxime, surgical drainage and intermittent closed continuous saline irrigation.
Non-tuberculous pyogenic spinal infection has an incidence of 2-4% in adult musculoskeletal infection. The incidence is relatively low but mortality rate is high up to 1-20%, according to the condition of the patients and the kind of pathogenic organisms.1) In early stage, the patients do not show any specific symptom. But the disease progresses abruptly and rapidly, which may lead to paralysis or death. The most prevalent pathogenic organism identified in nontuberculous pyogenic spinal infection is Staphylococcus aureus (60% of the patients was caused by the pathogen of S. aureus).2,3) However, pyogenic spinal infection by Klebsiella pneumoniae is very rare and only a few cases have been reported.1,4,5)
We report a case of non-tuberculous pyogenic spondylodiscitis with epidural abscess by Klebsiella pneumoniae.
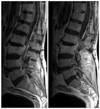
A 65-year-old male presented sudden onset of fever and low back pain for one day. He underwent a L4-5 decompressive laminectomy for lumbar herniated nucleus pulposus 11 years ago. Since then, the patient had shown no specific symptoms and episodes in lumbar spine. On the admission day, he had a blood pressure of 143/76 mmHg, a pulse rate of 91/min and a temperature of 38.4℃. The patient did not show any neurologic symptom but had some local heatness and mild dull nature pain with tenderness in his lumbar area. Any other infectious focus was not found. The routine laboratory evaluation showed 21,540/mm3 white blood cell, 87.9% polymorphonuclear, and erythrocyte sedimentation rate/C-reactive protein of 35 mm/hr (normal range, 0 to 15)/12.3 mg/dl (normal range, 0 to 0.5). The blood culture with periodic acid stain (PAS) and tuberculosis polymerase chain reaction (PCR) were performed. The urine culture was performed. Also, a computerized tomogram (CT) and magnetic resonance imaging (MRI) evaluations were performed. CT and MRI revealed the epidural abscess at L2-3 level with the destruction and liquefaction of L2-3 intervertebral disc, the bone marrow edema in the vertebral bodies of L2 and L3, and the psoas abscess at L3-4 level caused by spreaded infection (Fig. 1). The treatment was started with empirical intravenous antibiotics (the 1st generation cephalosporin and aminoglycoside).
On the 2nd day after admission, body temperature elevated up to 40℃, general condition was worse than the 1st day. However, there was no neurologic symptom.
On the 3rd day, Klebsiella pneumoniae was identified in blood culture. But, PAS and tuberculosis PCR were negative. Urine culture was also negative. Antibiotics was changed to the 3rd generation cephalosporin (Ceftriaxone).
On the 7th day, the authors found elevated liver enzyme. Antibiotics was changed again from Ceftriaxone to Cefotaxime.
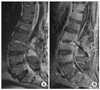
On the 12th day, the patient showed sudden onset of neurologic symptoms such as radiating pain of both legs, dorsiflexion weakness of both ankle, and numbness at perianal area. Emergency follow-up MRI evaluation revealed the increased pus in epidural space (Fig. 2). This neurologic symptom seemed to be associated with cauda equina compression caused by surrounding epidural abscess. The authors planned the two stage operation. The first was urgent decompression and drainage of epidural abscess due to patient's severe neurologic symptoms and pain. The second was anterior lumbar interbody fusion (ALIF), which would be considered according to patient's condition. The patient underwent the urgent operation; L2-3 decompressive laminectomy, the drainage of epidural abscess, partial discectomy, and insertion of two draining tubes through L2-3 intervertebral disc space (Fig. 3). The psoas abscess was remained. If the drainage of the psoas abscess was necessary, it would be performed with the secondary operation, ALIF. Then the patient underwent the intermittent continuous saline irrigation through draining entry tube and outlet tube for 1 week. After the first operation, his general condition showed significant improvement and neurologic symptom was gradually disappeared. As a result of intraoperative specimen (pus) culture examination, Klebsiella pneumoniae was also identified. Because the patient was improved rapidly, the second operation was not performed. Until the 6th week, he was treated with intravenous antibiotics (Cefotaxime) until ESR/CRP were normalized. On the 6th week, the patient discharged with prescription of oral antibiotics (ciprofloxacin) for 1 month. Until now (for 22 months), the patient had no recurrent symptom and sign of lumbar infection.
Among the patients diagnosed as pyogenic arthritis, the pyogenic arthritis by Klebsiella pneumoniae has a rare incidence of 1%. It most commonly involves lower big joints, especially knee when it is accompanied with underlying medical conditions or immunocompromised states such as diabetes, malignancy, chronic renal failure, alcoholism, rheumatoid arthritis, and bone marrow stem transplant recipients.6) Recently, an increased incidence of immunocopromised patients was associated with an increased incidence of atypical pyogenic infection. However, this patient had no evidence of immunocompromised condition except heavy alcohol drinking.
Pyogenic spinal infection by Klebsiella pneumoniae is more rarer than pyogenic spinal infection by Staphylococcus or Streptococcus. It was reported that the most frequent organism of pyogenic spinal infections is staphylococcus (69.6%) and others were Pseudomonas (8.7%), E. coli (4.3%), Proteus (4.3%), etc in Korea. Pyogenic spondylodiscitis with epidural abscess by Klebsiella pneumoniae had never been reported in Korea and only few cases had been reported in the world.1,7) Although infection by Klebsiella pneumoniae was rare, it has a susceptibility to the 3rd generation cephalosporins and sulfonamides fortunately.
In general, conservative therapy with antibiotic administration is the treatment of choice for pyogenic spondylitis due to respond well to antibiotics. Also, psoas abscess rarely requires surgical treatment because it usually responses to antibiotics.8) If conservative treatment is failed or neurologic symptom progresses, open surgery is required. For an appropriate treatment, many authors recommend the adequate antibiotics, surgical debridement, and drainage.
The effectiveness of percutaneous drainage under CT or ultrasound guidance has recently been reported good or excellent result in the treatment of pyogenic abscess in most locations in the body, including the abdomen, thorax, and retroperitoneum.9) However, valid long-term findings for use of this technique are not yet available. Because drainage alone may result in recurrence rates of up to 50%, percutaneous drainage may not be always sufficient for treatment of secondary epidural abscesses by pyogenic spondylitis.10)
Our treatment was the administration of adequate antibiotics, open surgical debridement and drainage with two tubes insertion and the intermittent continuous saline irrigation through these draingage tubes.
Although Klebsiella pneumoniae is rare organism to cause pyogenic spondylodiscitis, it could cause lumbar spondylodiscitis with epidural abscess. In the case of spinal infection, less common organism such as Klebsiella pneumonia should be also considered as pathogenic organism.
Figures and Tables
Figure 1
(A) Epidural abscess at L2-3 level on sagittal T2 weighted images, which compresses the dura of lumbar spine. Abnormal intensity of L2-3 interverteral disc space was seen. (B) Epidural abscess and the destruction of intervertebral disc at the L2-3 level and Psoas abscess at L3-4 level on axial T2 weighted images. (C) Epidural abscess and the destruction of intervertebral disc at the L2-3 level and Psoas abscess at L3-4 level on axial Gadolinium enhancement images.

References
1. Chevalier X, Marty M, Larget-Piet B. Klebsiella pneumoniae septic arthritis of a lumbar facet joint. J Rheumatol. 1992. 19:1817–1819.
2. Torda AJ, Gottlieb T, Bradbury R. Pyogenic vertebral osteomyelitis: analysis of 20 cases and review. Clin Infect Dis. 1995. 20:320–328.

3. Vorbeck F, Morscher M, Ba-Ssalamah A, Imhof H. Infectious spondylitis in adults. Radiologe. 1996. 36:795–804.

4. Kouroussis C, Georgoulias V, Souglakos J, Simvoulakis E, Karabekios S, Samonis G. Spontaneous spondylodiscitis caused by Klebsiella pneumoniae. Infection. 1999. 27:368–369.

5. Porras JA, Bayona C, Gutiérrez MC, Vidal F. Vertebral osteomyelitis due to Klebsiella pneumoniae. An Med Interna. 1994. 11:154–155.
6. Apple JS, Halvorsen RA, Chapman TM, Martinez S. Klebsiella pneumoniae arthritis of the hip in a diabetic patient. South Med J. 1984. 77:229–231.

7. DelCurling O Jr, Gower DJ, McWhorter JM. Changing concepts in spinal epidural abscess: a report of 29 cases. Neurosurgery. 1990. 27:185–192.
8. Yacoub WN, Sohn HJ, Chan S, Petrosyan M, Vermaire HM, Kelso RL, et al. Psoas abscess rarely requires surgical intervention. Am J Surg. 2008. 196:223–227.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download