Abstract
Purpose
The objective of this study was to determine the patterns of C-reactive protein (CRP) changes during the postoperative period after total knee replacement (TKR), and to determine the CRP changes associated with infection after TKR.
Materials and Methods
A retrospective analysis of the pattern of CRP changes during the first 6 postoperative months was conducted on 2,315 patients who underwent unilateral or simultaneous bilateral TKR. This data was also compared with the pattern of CRP changes which occurred in 19 patients with a deep prosthesis infection who were not enrolled in the main study.
Results
The CRP levels peaked 3 days postoperatively, and then decreased to baseline levels at 15-28 days postoperatively. Within 14 days postoperatively, the CRP levels were significantly higher in the simultaneous bilateral TKA group than in the unilateral group (p<0.01). Thereafter, no significant difference in CRP levels existed between two groups. After the 8th postoperative day, a significant difference in CRP level existed between patients with and without deep prosthesis infections.
Figures and Tables
Fig. 1
The change of average CRP levels in each perioperative interval in unilateral TKR (UTKR) group and simultaneous bilateral TKR (BTKR) group. Within 14 days postoperatively, CRP levels were significantly higher in the simultaneous bilateral TKA Group than in the unilateral group (p<0.01).

Fig. 2
The comparison of the change of average CRP levels in whole study cases and deep prosthesis joint infection (PJI) cases. After 8 days postoperatively, a significant difference was observed between patients with and without deep prosthesis infection.

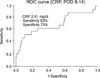
Fig. 3
ROC curve (receiver operating characteristic curve) for CRP values in postoperative 8 to 14 days shows fair discrimination (Area under the curve=0.699) in unilateral TKR group and simultaneous bilateral TKR group.
References
1. Haidar SG, Charity RM, Bassi RS, Nicolai P, Singh BK. Knee skin temperature following uncomplicated total knee replacement. Knee. 2006. 13:422–426.

2. Mehra A, Langkamer VG, Day A, Harris S, Spencer RF. C reactive protein and skin temperature post total knee replacement. Knee. 2005. 12:297–300.

3. Bernard L, Lübbeke A, Stern R, et al. Value of preoperative investigations in diagnosing prosthetic joint infection: retrospective cohort study and literature review. Scand J Infect Dis. 2004. 36:410–416.

4. Fischer CL, Gill C, Forrester MG, Nakamura R. Quantitation of "acute-phase proteins" postoperatively. Value in detection and monitoring of complications. Am J Clin Pathol. 1976. 66:840–846.

5. Greidanus NV, Masri BA, Garbuz DS, et al. Use of erythrocyte sedimentation rate and C-reactive protein level to diagnose infection before revision total knee arthroplasty. A prospective evaluation. J Bone Joint Surg Am. 2007. 89:1409–1416.
6. Peltola H, Laipio ML, Siimes MA. Quantitative C-reactive protein (CRP) determined by an immunoturbidimetric method in rapid differential diagnosis of acute bacterial and viral diseases of children. Acta Paediatr Scand. 1984. 73:273–274.

7. Lee DC, Kim SD, Jung KA, Baek SH. Changes of ESR and CRP after total knee and hip arthroplasty. J Korean Knee Society. 2001. 12:23–29.
8. Parvizi J, Ghanem E, Sharkey P, Aggarwal A, Burnett RS, Barrack RL. Diagnosis of infected total knee: findings of a multicenter database. Clin Orthop Relat Res. 2008. 466:2628–2633.

9. Mok JM, Pekmezci M, Piper SL, et al. Use of C-reactive protein after spinal surgery: comparison with erythrocyte sedimentation rate as predictor of early postoperative infectious complications. Spine. 2008. 33:415–421.
10. Osei-Bimpong A, Meek JH, Lewis SM. ESR or CRP? A comparison of their clinical utility. Hematology. 2007. 12:353–357.

11. Shih LY, Wu JJ, Yang DJ. Erythrocyte sedimentation rate and C-reactive protein values in patients with total hip arthroplasty. Clin Orthop Relat Res. 1987. 225:238–246.

13. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 2005. 340:448–454.

14. Marnell L, Mold C, Du Clos TW. C-reactive protein: ligands, receptors and role in inflammation. Clin Immunol. 2005. 117:104–111.

15. Andres BM, Taub DD, Gurkan I, Wenz JF. Postoperative fever after total knee arthroplasty: the role of cytokines. Clin Orthop Relat Res. 2003. 415:221–231.

16. Di Cesare PE, Chang E, Preston CF, Liu CJ. Serum interleukin-6 as a marker of periprosthetic infection following total hip and knee arthroplasty. J Bone Joint Surg Am. 2005. 87:1921–1927.

17. Pearle AD, Scanzello CR, George S, et al. Elevated high-sensitivity C-reactive protein levels are associated with local inflammatory findings in patients with osteoarthritis. Osteoarthritis Cartilage. 2007. 15:516–523.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download