Advances in multimodality treatments, including systemic chemotherapy, have made limb salvage surgery of the distal tibia increasingly feasible7). According to previous reports, ankle arthrodesis is regarded as the best reconstructive procedure after limb salvage surgery for osteosarcoma of the distal tibia. Of the many arthrodesis options, vascularized fibular graft (VFG) is widely accepted as the most successful method. However, reconstruction using VFG is not always possible, because VFG is a highly demanding surgical procedure and is associated with high rates of morbidity at donor sites. Meanwhile, some authors have reported a novel procedure using the intrinsic potential of the periosteum to bridge massive long bone defects6,7). The authors in this study devised a novel reconstructive surgical procedure that exploits the osteogenic potential of the periosteum as an alternative to the VFG method.
CASE REPORT
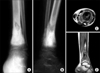
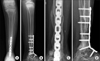
A 10-year-old female patient with painful swelling of the distal tibia was diagnosed by open biopsy as having osteosarcoma. Imaging studies (plain radiographs, MRI, chest CT, and bone scanning) revealed that the Enneking stage was IIB. Preoperative chemotherapy, according to Rosen's T-10 regimen2), consisted of weekly high dose methotrexate (12 g/m2) for 2 consecutive weeks, followed by cisplatin (100 mg/m2) and doxorubicin (30 mg/m2×2 days). After pre- operative chemotherapy (Fig. 1), wide en bloc excision and tibio-talar arthrodesis were performed. For the reconstruction of the created tibial defect, the distal segment of the ipsilateral fibula was transported. In order to preserve its periosteal blood supply, the distal one-half of the periosteum was attached to the transported fibula, while the proximal one-half of the periosteum was pealed out of its surrounding periosteum. Osteotomy was performed, and the transport-segment was moved out of its periosteal sleeve (Fig. 2). The authors hollowed out a groove on the dome of the talus, and the distal fibula of the transported segment was impacted into the groove. Two plates were applied at the proximal and distal junctions to stabilize the reconstruction. A supplementary iliac bone graft was added between the periosteal sleeve and transported fibula. Postoperatively, a long leg cast was applied for one month and was then converted to a PTB cast until achievement of solid union. According to the pathologic report, the margin of the specimen was free from tumor cells, and the degree of tumor necrosis was rated as Grade III (more than 90% necrosis). Post-operatively, the patient was treated with the same chemotherapeutic agents that had been given before surgery and was followed monthly at our outpatient clinic by chest and affected bone radiography, at two months intervals. Chest CT and radionuclide bone scans were performed every three months for two years. New bone formation along the periosteal sleeve was detected at three months post-operatively (Fig. 3A), and complete graft union between the periosteal new bone and transported fibula was achieved at twelve months. A fracture of the transported fibula shaft that developed at nine months postoperatively (Fig. 3B) was treated with an autogenous iliac bone graft and secure with internal fixation using a single plate and multiple screws. At final follow-up (36 months postoperatively), the grafted fibula and periosteal new bone had united as one unit providing stable structural support to the lower leg (Fig. 4). According to the Musculoskeletal Tumour Society scoring system4), the patient's post-operative functional score was 27 (90%). No evidence of local recurrence or distant metastasis was observed at final follow up.
DISCUSSION
Previously described surgical techniques for reconstruction include endoprosthetic replacement and allograft and/or microvascular fibular transfer by fibular transfer alone or by bone transport using distraction osteogenesis. Although ankle endoprosthetic replacement has occasionally been carried out in patients with osteosarcoma of the distal tibia, accumulated evidences have revealed many unwanted complications and high rates of failure1,8,9). Therefore, many authors agree that ankle arthrodesis is the best reconstructive procedure after wide resection of osteosarcoma of the distal tibia, although it has been associated with loss of ankle motion and frequent nonunion at the arthrodesis site3). Of the many arthrodesis options, VFG is widely accepted as the most successful method. Because the living fibula has its own vasculature, unfavorable bed condition at the tumor resection site does not matter in the host-graft union5). This point is important in tumor surgery, due to frequent lack of soft tissue coverage. Moreover, hypertrophy of the grafted fibula provides stronger support with time. Even though, non-vascularized autogenous fibular grafts hypertrophy, they are inferior to the VFG technique due to the lack of their own vasculature. Thus, recently, vascularized fibular grafts are preferred by the majority of authors. However, reconstruction using VFG is not always possible, because VFG is a complicated surgical procedure and is associated with high rates of morbidity at donor sites. Furthermore, the protracted operation time required is unacceptable for small children who have just undergone preoperative chemotherapy. Many authors have expressed the need for a novel form of surgery that is technically easy, can be performed quickly, and has low donor site morbidity. Our proposed method was based on the theory that an in situ periosteal sleeve can provide new bone formation in itself6,7), and that vascularity might be maintained by retaining the periosteal sleeve of the graft fibula. It was inconvenient not to prevent fracture of the transported fibula due to inadequate secure fixation and used of dual plates at initial operation. A wrong decision in the initial operation allowed for formation of a stress fracture and nonunion. However, our result showed that the periosteal new bone formation and the transported fibula acted as a dual strut graft providing stronger structural support relatively early in the postoperatively period. We believe our method has several advantages, namely, easier graft harvesting, provision of a dual bone graft effect preventing stress fracture, and a direct blood supply to the graft fibula through the periosteal sleeve.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download