Synovial osteochondroid metaplasia is a tumorous condition in which synovial cells undergoes metaplasia and produce a bony and cartilaginous mass. Although synovial osteochondromatosis of the elbow joint has been frequently reported as multiple lesions1,3,4,6,8-10), synovial osteochondroid metaplasia presenting as a solitary mass lesion has not been frequently reported in the literature. While the multiple lesions in synovial osteochondromatosis help us to avoid the mis-diagnosis of a fracture, a solitary bony fragment in a patient with synovial osteochondroid metaplasia can cause the incorrect diagnosis of an acute bony injury. We present here a case of synovial osteochondroid metaplasia of the elbow joint that mimicked a fracture in a military recruit who had undergone minor direct trauma to the joint. The lesion was initially mistaken for an acute fracture.
CASE REPORT
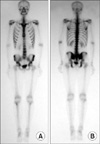
A twenty-one-year-old man presented with acute pain in his left elbow after minor direct trauma to the joint. He was a military recruit and was injured during a military drill. He complained of tenderness at the lateral side of his elbow. On clinical examination there was no skin bruise or scratch around the elbow. Although any swelling of the joint was not detected, the range-of-motion was limited due to pain. There was no neurovascular deficit. The simple radiographs showed a radio-opaque density around the radio-capitellar joint, and computed tomography (CT) scans revealed a small bony fragment on the posterolateral side of the elbow joint (Fig. 1). The clinical diagnosis was fracture either of the capitellum or the radial head. To avoid entanglement due to the loose body and to confirm the diagnosis, an operation was performed on the 7th day after presentation. Repositioning of the fractured fragment and internal fixation, or excision of the fragment was planned. The posterolateral approach to the elbow between the anconeus and extensor carpi ulnaris was chosen. There was no soft tissue hematoma, swelling of the joint or any evidence of intra-articular bleeding. The fragment was a 1.5 by 1.3 by 0.5 cm sized mass embedded in the synovium. The lack of evidence for an acute injury led us to simply excise the fragment en bloc (Fig. 2). Postoperatively, the bone scintigraphy performed 3 days later revealed no evidence of bony injury (Fig. 3). The findings of the histopathological slides were osteocartilagenous tissue buried in the fibromuscular tissue, which was compatible with osteochondroid metaplasia (Fig. 4). The final diagnosis of osteochondroid metaplasia of the elbow joint was made. At postoperative 1 year, he had no difficulty in the activities of daily living, and no evidence of recurrence could be documented.
DISCUSSION
Loose bodies of the elbow joint may originate from osteoarthritis, trauma and osteochondritis dissecans, or they may exist as idiopathic lesion1,3). The common presentations are pain or mechanical symptoms such as catching or locking, none of which is specific6,7). Incidentally detected single loose bodies of the elbow joint that are without pain or mechanical symptoms has received little attention by clinicians. If a bony fragment is seen on a radiograph of an acutely injured person, the clinician is liable to reach the diagnosis of a fracture as the first impression. Synovial osteochondroid metaplasia, which has similar radiologic features to a fracture fragment should be included in the differential diagnosis of an acutely injured joint.
The main phenomenal difference between synovial osteochondromatosis and synovial osteochondroid metaplasia is the multiplicity, although the histopathological findings are similar. The clinical manifestation may be related to the mass effect of the lesion. While synovial osteochondromatosis is rarely mistaken for a fracture, synovial osteochondroid metaplasia is liable to be misdiagnosed. The pain in synovial osteochondromatosis may accompany not only exertion, but it may be due to effusion, locking, nerve compression or secondary osteoarthritic changes1,7). The extra-articular manifestations may be bursitis around the elbow joint7) or peripheral nerve compression, including ulnar nerve entrapment neuropathy2,10) and entrapment of both the median nerve at the wrist and the posterior interosseous nerve at the elbow5). Operative excision with debridement and synovectomy has often been performed to treat the mechanical symptoms6,8,10). Synovial osteochondromatosis is rarely associated with malignant transformation and distant metastasis9), recurrence 6,8) or osteoarthritic change6,8).
The pain of a current case might originate from the contused soft tissue or exacerbation of the vague pain associated with a tumor. However, even though we included the correct diagnosis in preoperative differential diagnosis, the management plan might not have been different. The operative excision of the lesion might be justified in that the surgical wound was small and the functional impairment associated with the operation itself was minimal. It is, however, important to consider all the possible morbid conditions preoperatively, and to include synovial osteochondroid metaplasia in the differential diagnosis. Omitting this disease from the differential diagnosis might bring about medicolegal conflict in certain situations such as military recruits, industrial workers, etc.
The dearth of definitive preoperative diagnostic methods for synovial osteochondroid metaplasia accentuates the importance of having a clinical suspicion for this disease. None of the diagnostic test, including simple radiography, CT scans or bone scintigraphy, can provided a definite positive result for the synovial osteochondroid metaplasia or synovial osteochondromatosis. The morphological features on radiographs or CT scans sometimes fall between acute injury and a tumorous condition. Although preoperative bone scintigraphy may be helpful to discriminate acute bony lesion, it cannot exactly discern a tumorous lesion from a fracture. Milgram described 3 histopathological phases in the growth of synovial osteochondromatosis, and they consist of intrasynovial involvement, intrasynovial involvement and free bodies (transitional), and multiple free bodies due to synovial osteochondromatosis9); the activity of the lesion is variable according to the phases. The discrimination between acute bony injury and osteochondrogenic tumor might not be clear on hot uptakes, while a tumorous entity cannot be excluded by an absence of hot uptake. Hence, the final diagnosis should be made histopathologically, and a diagnostic suspicion by the physician for this malady is mandatory.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download