Abstract
We describe a case of posterolateral capsular heterotopic ossification requiring a surgical excision after a PCL (Posterior Cruciate Ligament) reconstruction using the modified inlay method and PLCS (posterolateral corner sling) with a tibia tunnel. A 21-year-old female patient had suffered a blunt proximal tibial direct trauma 6 months earlier. She did not experience limb ischemia or a pulse deficit before she visited our out patient clinic. She had not suffered any trauma in other sites, and showed a range of motion of 0 to 30° at 4 months after surgery. There was no specific finding on the X-ray images. Arthroscopic adhesiolysis was performed and her range of motion increased to 0 to 120°. However, 6 months after the initial operation, she showed ankylosis and heterotopic ossification at the posterior aspect, which was surgically removed at 12 months postoperatively. After the second surgery, there was no recurrence and she showed a 0 to 140o range of motion at postoperative 42 months.
Heterotopic ossification (HO) is defined as the formation of mature lamellar bone in the soft tissue3,7). Ogilvie-Harris and Sekyi-Out described four cases of heterotopic ossification requiring surgical intervention after an arthroscopic anterior cruciate ligament (ACL) reconstruction, and Patton et al reported 3 cases after knee dislocations, in which the PCL was one of the structures reconstructed7). Most cases did not require a surgical excision, and were due to relatively definite causes. On the other hand, our patient had a vague cause and required a surgical excision. We report this case with a review of the relevant literature.
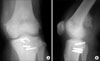
A 19-year-old woman visited the out patient clinic with right knee painful instability. She had suffered a direct pretibial trauma when she slipped down 6 months earlier. The clinical examination and MRI results were consistent with a tear of the PCL, a posterolateral corner injury showing PLRI and an incomplete peroneal nerve injury that recovered completely (Fig. 1). The clinical examination under anesthesia revealed increased posterior displacement at 90 degrees flexion with a loss of stepping, a positive reverse Povot-shift test and increased external rotation at 30 and 90° flexion. Arthroscopy revealed pseudolaxity of the anterior cruciate ligament and a drive through sign. The remnant of the PCL bundle was tensioned and anterolateral bundle of PCL was reconstructed using the modified inlay method with an ipsilateral hamstring5,6). The PLRI was restored by PLCS with a tibia tunnel using a contralateral hamstring1). The rehabilitation and follow up were performed as usual5,6). Two weeks after surgery, the patient had an active range of motion of 0 to 70° with no significant discomfort, and she was discharged with PCL brace. However, 6 weeks after surgery, the patient reported significant pain and a range of motion of only 0 to 30°, despite undergoing continued physical therapy. She had persistent pain and a range of motion 3 months after surgery, and the radiographs taken at this time showed no specific abnormality. Under general anesthesia, she showed a similar range of motion. Arthroscopic adhesiolysis and manipulation under anesthesia were performed, and a passive range of motion of 0 to 120° was gained postoperatively. However, 6 months after the initial surgery, she had a range of motion of 15 to 90° with walking difficulties. The radiographs taken at this time showed heterotopic ossification at the posterior supracondylar aspect (Fig. 2). From that time, the range of motion was not changed and a decision was made to excise the ossification fragment 12 months after surgery. Arthroscopy revealed a normally looking PCL and no specific intraarticular abnormality. The patient's position was changed and the mass was approached via the posterior aspect.
The mass was palpable, oval shaped and measured 3×5×2 cm. The range of motion improved markedly reaching 0-140° 6 months after the procedure and the patient could walk without any specific difficulty. Thirty months after the excision operation, the patient had no complaints about her knees and there were no changes observed on the radiographs (Fig. 3).
Heterotopic ossification is a common complication after a musculoskeletal injury. It is associated with central nervous system damage, burns, trauma, and a hereditary disorder known as fibrodysplasia ossificans progressiva7). Local factors including stasis, hematoma, edema, and prolonged immobilization are often cited as contributing factors9).
Although heterotopic ossification after an arthroscopic anterior cruciate ligament reconstruction has been reported, most reports of ligament injuries were of multiligament injuries, which did not require surgical removal7). However, some authors reported medial heterotopic bone requiring a surgical excision in all their patients2,4). We performed more than 150 PCL inlay reconstructions and 100 PLCS procedures but this is the only case with this complication. Our patient did not suffer a brain injury or other factors known to cause heterotopic ossification. As suggested by other authors7), it is believed that reaming for the graft tunnels particularly PLCS with a femoral tunnel contributed to the process. The link between the posterior surgical bony procedure and posterior capsular ossification has not been recognized, and our report should raise the clinical awareness of such an entity.
For diagnosis, radiographs should be obtained to exclude heterotopic ossification in any patient with pain and a loss of motion, particularly after a knee dislocation, as well as in patients with a history of heterotopic ossification in other anatomic locations. In addition, patients with pain and loss of motion should raise suspicion, even if they have suffered only minor ligament injury or a reconstruction.
The optimal protocol for a resection of heterotopic ossification with regards to the timing and adjunctive measures, such as radiation and indomethacin to prevent a recurrence, is controversial10). Most authors advocate a minimum wait of 1 year after heterotopic bone formation before the surgical excision8).
In conclusion, reaming of the graft tunnels during PLCS contributes to the process of heterotopic ossification. However, there is the possibility that a capsular injury during the PCL inlay procedure might cause such complications.
Figures and Tables
References
1. Albright JP, Brown AW. Management of chronic posterolateral rotatory instability of the knee: surgical technique for the posterolateral corner sling procedure. Instr Course Lect. 1998. 47:369–378.
2. Charnley G, Judet T, Garreau de Loubresse C, Mollaret O. Excision of heterotopic ossification around the knee following brain injury. Injury. 1996. 27:125–128.

3. Dalury DF, Jiranek WA. The incidence of heterotopic ossification after total knee arthroplasty. J Arthroplasty. 2004. 19:447–452.

4. Ippolito E, Formisano R, Farsetti P, Caterini R, Penta F. Excision for the treatment of periarticular ossification of the knee in patients who have a traumatic brain injury. J Bone Joint Surg Am. 1999. 81:783–789.

5. Jung YB, Jung HJ, Tae SK, Lee YS, Lee KH. Reconstruction of the posterior cruciate ligament with a mid-third patellar tendon graft with use of a modified tibial inlay method. J Bone Joint Surg Am. 2005. 87:Suppl 1. S247–S263.

6. Jung YB, Tae SK, Jung HJ, Lee KH. Replacement of the torn posterior cruciate ligament with a mid-third patellar tendon graft with use of a modified tibial inlay method. J Bone Joint Surg Am. 2004. 86:1878–1883.

7. Patton WC, Tew WM. Periarticular heterotopic ossification after multiple knee ligament reconstructions. A report of three cases. Am J Sports Med. 2000. 28:398–401.
8. Saito N, Horiuchi H, Takahashi H. Heterotopic ossification in the knee following encephalitis: a case report with a 10-year follow-up. Knee. 2004. 11:63–65.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download