Abstract
The dystrophic type of neurofibromatosis is a well-known bizarre deformity of the spine. There has been little literature about spontaneous vertebral column dislocation in the thoracic spine with progressive neurological symptoms. The authors present a case of thoracic spine dislocation vertically and transversely with intact posterior elements. A 35-year-old woman had stooping and back pain for five years. She developed motor weakness of both lower extremities three months ago. Plain X-ray and three-dimensional CT scans showed dislocation between T5 and T6 vertebrae, that were which was translated transversely and vertically with severe resorption of vertebral pedicles of T5 and T6. After skeletal traction, motor weakness was improved. And we performed two-staged anterior and posterior fusion to stabilize severe kyphoscoliosis. The patient was improved neurologically with free ambulation state at 24-month follow-up. Combined anterior and posterior fusion was an effective method for the treatment spontaneous vertebral column dislocation in the thoracic spine with progressive neurological symptoms.
Scoliosis in neurofibromatosis is considered as the most common spinal manifestation, with the incidence ranging from 2% to 36%1). The dystrophic type is less common than the non-dystrophic type, difficult to manage. It is characterized by an angular curve of a short segment with bizarre deformities of the spine. There have been only several cases of vertebral column dislocation in neurofibromatosis. We present a case of neurofibromatosis which had its vertebral column dislocated vertically and transversely with intact posterior elements in the thoracic spine and progressive neurological symptoms.
A 35-year-old woman with five-year history of progression of hump in her back had sudden and progressive paraparesis which began three months ago. The patient was unable to ambulate without support. She had been diagnosed as neurofibromatosis five years ago. There was no antecedent trauma.
On the physical examination, multiple cafe-au-lait spots were all over her skin which was diagnosed as neurofibromatosis with a biopsy finally. The muscle strength during extension of the hip and knee joints were grade 2 and 3, respectively, and below the ankle joint were grade 4 for both sides. She had sensory loss of the trunk and the lower extremity. It was 20% of the normal between T6 and L2 dermatomes and 50% for below L3 dermatome. For lower-extremities, reflexes were markedly hyperactive, and the Babinski reflexes were positive. There was sustained ankle clonus bilaterally.
The segmental kyphosis involving T4 through T7 was 95 degrees on plain radiographs (Fig. 1). Three-dimensional CT scans revealed a complete dislocation of the fourth and fifth vertebrae on the sixth and seventh anterolaterally, with the body of the T4 and T5 located immediately anterior and right side to that of T6 and T7 (Fig. 2). Axial images of CT scans showed severe destruction and resorption of vertebral pedicles of T5 and T6. The left pedicle of T4 and the right pedicle of T7 showed incomplete irregular resorption (Fig. 3). MRI showed dural ectasia around the lesion (Fig. 4). The posterior structures including spinous process, lamina, and facet joints were all aligned along the smooth scoliotic curve without any subluxation or dislocation.
For the correction of kyphotic deformity, halopelvic traction was applied with gradually increased weight. Paraparesis improved at eight pounds and worsened at 15 pounds of traction. The weight was maintained at eight pounds until operation. After ten days of traction, we planned two-staged in situ posterior fusion followed by anterior fusion. The first procedure included posterior pedicle screw instrumentation and fusion from T2 to T12 vertebrae with a posterior approach. The neurological status was not aggravated postoperatively.
The second procedure was performed three weeks later, using high thoracic periscapular approach with the patient in the left lateral decubitus position. After removal of interposed fibro-osseous tissues around T4-T7 vertebral bodies, in situ fusion was performed without reduction of kyphoscoliosis. The resected fourth rib was grafted as a strut bone between T4 and T7 vertebral body and additional cancellous chip bone graft was done around the strut graft. The neurological findings remained normal after operation. The segmental kyphosis involving T4 through T7 was corrected to 48 degrees on lateral radiographs (Fig. 5).
The body jacket cast was applied postoperative for four months. The patient improved neurologically with free ambulation state at 24-months follow-up.
Neurofibromatosis is a disorder of neural crest cells involving not only neuroectoderm and mesoderm but also endoderm, caused by the defect in the gene called neurofibromin on the long arm of chromosome 173). The characteristics of dystrophic changes including enlargement of foramen, scalloping of vertebral bodies, rib deformities, and structural defect in pedicles are well known. One of the possible etiologies for this condition is regional dystrophy and dysplasia affecting both bone and meninges that have been referred to as mesodermal dysplasia2,8). Although subluxation or dislocation of spinal column in neurofibromatosis is very rare, progressive dystrophy of bony elements, dural ectasia, and laxity of ligamentous structure may cause structural instability of the vertebral column6,8,9).
In our review of literature, we found only several cases that had vertebral column dislocation8,9). Rockower, et al.6) reported two cases of spinal dislocation after minor trauma in children who had neurofibromatosis. Stone, et al. reported one case, a nine year-old boy who had dislocation of the first on the second thoracic vertebra and no neurological deficit8). Winter9) reported a case that had dislocation of the ninth on the tenth thoracic vertebra.
The mechanism of the spontaneous dislocation in neurofibromatosis is uncertain. Simpson, et al7). reported that three cases with a traumatic bilateral pedicular fracture in the thoracic spine maintained the continuity of posterior elements and the cord whereas the body was displaced. In their cases, the spinal cord was not compressed and showed normal neurological findings that might be a possible explanation for the spinal column dislocation in neurofibromatosis. After severe osseous erosion and resorption of vertebral pedicles, separation of the vertebral body may occur without disruption of posterior elements and the spinal cord in neurofibromatosis.
For the treatment of a patient who has flexible kyphotic deformities with mild neurologic deficit, preoperative halo traction could be recommended 4). In our case, vertebral bodies were severely displaced and translated and, we attempted a closed reduction of the vertebral column by halopelvic traction, which improved the neurology of the patient at eight pounds. However, neurological deficits of the patient were deteriorated with weights more than 15 pounds. Thus, we performed in situ anterior and posterior fusion after minimal skeletal traction. Although posterior fusion alone may provide stability for the patients with non-dystrophic or dystrophic curves without kyphosis, combined anterior and posterior fusion has been generally recommended to stabilize dystrophic curves in neurofibromatosis5). In a study of Parsini, et al5), the failure rate of posterior fusion was higher in the patients with kyphosis greater than 50 degrees, and the addition of planned anterior fusion decreased the failure rate more than 50%. Winter, et al10). emphasized the importance of combined anterior and posterior fusion at an early stage and explained the use of small amount of bone graft in limited area was a major reason for pseudarthrosis. In conclusion, the dystrophic kyphoscoliosis with neurofibromatosis and loss of bilateral pedicles may cause the vertebral column dislocation with progressive neurological deficit. Combined anterior and posterior fusion was an effective method for the treatment of dystrophic deformity.
Figures and Tables
Fig. 1
The anteroposterior and lateral radiograph shows a thoracic kyphoscoliosis and 95 degrees of segmental kyphosis involving T4 through T7.
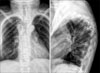
Fig. 2
Three dimensional CT scan shows a complete dislocation of the fourth and fifth vertebrae on the sixth and seventh anterolaterally, with the body of the T4 and 5 situated immediately anterior and right side to that of T6 and 7. All the posterior structures are preserved with smooth scoliotic curve.

Fig. 3
Two consecutive axial CT images showing severe destruction and resorption of vertebral pedicles of T5 and 7.

References
1. Akbarnia BA, Gabriel KR, Beckman E, Chalk D. Prevalence of scoliosis in neurofibromatosis. Spine. 1992. 17:Suppl 8. S244–S248.

2. Crawford AH, Al-Sayyad MJ. Clark R, editor. Miscellaneous conditions of the cervical spine. Neurofibromatosis, juvenile rheumatoid arthritis, and Rickets. The cervical spine. 2004. 4th ed. Philadelphia: Lippincort Williams and Wilkins;481–507.
3. Goldberg NS, Collins FS. The hunt for the neurofibromatosis gene. Arch Dermatol. 1991. 127:1705–1707.

4. Kim HW, Weinstein SL. Spine update. The management of scoliosis in neurofibromatosis. Spine. 1997. 22:2770–2776.
5. Parisini P, Silvestre M, Greggi T, Paderni S, Cervellati S, Savini R. Surgical correction of dystrophic spinal curves in neurofibromatosis. Spine. 1999. 24:2247–2253.

6. Rockower S, McKay D, Nason S. Dislocation of the spine in neurofibromatosis. A report of two cases. J Bone Joint Surg Am. 1982. 64:1240–1242.

7. Simpson AH, Williamson DM, Golding SJ, Houghton GR. Thoracic spine translocation without cord injury. J Bone Joint Surg Br. 1990. 72:80–83.

8. Stone JW, Bridwell KH, Shackelford GD, Abramson CL. Dural ectasia associated with spontaneous dislocation of the upper part of the thoracic spine in neurofibromatosis. A case report and review of the literature. J Bone Joint Surg Am. 1987. 69:1079–1083.

9. Winter RB. Spontaneous dislocation of a vertebra in a patient who had neurofibromatosis. Report of a case with dural ectasia. J Bone Joint Surg Am. 1991. 73:1402–1404.

10. Winter RB, Lonstein JE, Anderson M. Neurofibromatosis hyperkyphosis: a review of 33 patients with kyphosis of 80 degrees or greater. J Spinal Disord. 1988. 1:39–49.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download