Abstract
Purpose
To evaluate the clinical results of a unilateral balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures (VCFs).
Materials and Methods
Twenty patients, 23 cases of osteoporotic VCFs who failed to respond to nonoperative treatments and who were confirmed by a consultant radiologist, were enrolled in this study. Times between injury and operation varied from 2 weeks to 2 months. All patients except two (18 female, 2 male patients), were female, and mean patient age was 71.7 (58-82) years. Follow-ups were conducted at least 12 months (12-27, mean 18.3). All patients underwent unilateral balloon kyphoplasty. Roentgenographic assessments were perform to evaluate fractured vertebra restoration and reduction loss. A ten-point visual analogue scale was used to measure pre- and postoperative pain severity.
Results
Preoperative anterior, middle and posterior heights of vertebra bodies were 57.8%, 66.1% and 85.3% of normal at presentation and these increased to 76.2%, 80.1%, 88.7% respectively at immediately after operation and at last follow-up, heights of each portion were 74.4%, 78.6%, 87.3%. Mean preoperative kyphotic angles of 17.6° at presentation improved to 8.9° at immediately after operations and to 9.1° at last follow-ups. Loss of reduction was 1.8%, 1.5%, 1.4% and 0.2°. Mean pain scores were 8.5 before surgery, 2.5 immediately after operations and 2.7 at last follow-ups. Statistical analysis showed a significant decrease in kyphotic angle (p=0.03) but VAS scores were no different (p=0.056). Anterior, middle and posterior body height was decreased with a statistical significance between two period (p<0.001). PMMA leakage occurred in 3 cases, but they did not cause neurologic deficits.
Osteoporotic VCFs are not uncommon disease and thus, many patients may suffer from actue pain and from chronic symptoms and resultant osteoporotic spinal deformities due to these fractures. Osteoporotic VCFs restrict ambulation, reduce quality of life, and reduce lifespan. Their adverse affects on the activities of daily living are almost as great as those associated with hip fractures8). Primary treatment for osteoporotic VCFs is conservative and includes bed rest, analgesics, and early ambulation with a brace after relieving symtoms. However, some patients complain of severe pain that does not respond to these conservative treatments and even progressive collapse of vertebral bodies and kyphosis may occur with or without neurologic deficit. Even though more aggressive treatment may be needed in these cases, the majority of patients with osteoporotic VCFs are not good candidates for general anesthesia. During the past decades, vertebroplasty (VP), has been adopted as an optimal treatment of osteoporotic VCFs, and has the advantages of rapid pain relief and a long-lasting effect, but it cannot make fully restore the height of affected vertebra bodies. The introduction of a newly designed, minimally invasive technique, balloon kyphoplasty (BK), has allowed collapsed vertebral body to be restored using an inflatable bone tamp. Moreover a viscous polylmethylmethacrylate (PMMA) is then introduced to the hollow cavity produced under low pressure.
Here the authors report our experience of balloon kyphoplasty using a unilateral approach, and describe the results of our evaluation and the efficacy of unilateral BK for the treatment of osteoporotic VCFs.
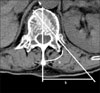
Twenty patients, 23 cases of osteoporotic VCFs who failed to respond to conservative treatment confirmed by a consultant radiologist were enrolled in this study. Times between injury and operation varied from 2 weeks to 2 months. Twenty one women and two men were enrolled in this study (mean age : 71.7 (58-82) years). The minimum follow-up period was minimum 12 months. Average bone density (T-score) using DEXA (dual energy X-ray absorptiometry) was -4.8 (-3.9 - -6.4). All patients were classified as more than grade III according to the ASA (American Society of Anesthesiology) classification. Before operations, plain anteroposterior (AP) and lateral views, radioscintigraphy, computed tomography (CT) or magnetic resonance imaging (MRI) were performed to confirm diagnosis and to exclude pathologic or metastatic disease. Whole procedures were performed under the local anesthesia. Based on peoperatively measured indexes, including angle of bone tamp and distance from the midline (Fig. 1), Balloon kyphoplasty using a unilateral approach were performed under fluoroscopic guidance. The operative indications for unilateral approach were the same as for the bilateral approach. However, unlike the bilateral approach, the bone tamp was advanced more across the midline on anteroposterior view. Also, to avoid great vessel injury, bone tamp entry was performed on the same side as great vessels. The remaining procedures were identical to those used during the bilateral approach. Postoperatively plain AP, lateral X-ray and CT were performed. Anterior, middle and posterior heights of vertebral bodies and local kyphotic angles were measured at preoperatively, immediate postoperatively and at final follow-up. Vertebral body heights were measured as follows. Anterior, middle, and posterior vertebral heights were defined as the distances between the upper and lower endplates at the anterior, posterior cortical margin and center of the fractured vertebra body. Vertebral body heights were expressed as ratio of estimated prefracture heights. Prefracture heights were defined as average value of the sum of the heights of the two adjacent vertebrae. All patients were evaluated using a ten-point Visual Analogue Scale (VAS) for pre- and postoperative pain severity. Postoperative changes in vertebral body heights and in VAS scores were analyzed using the paired Student's t-test, and the one sample t-test was used to compare the results of the present study with result using bilateral kyphoplasty reported by Berlemann et al2). P-values of <0.05 considered significant.
Preoperative anterior, middle and posterior heights of vertebra body of 57.8%, 66.1%, 85.3% was increased to 76.2%, 80.1%, 88.7% immediately after operation and at the last follow-ups, these heights had increased to 74.4%, 78.6%, 87.3%, respectively. The mean preoperative kyphotic angle of 17.6° improved to 8.9° at immediate after operations and to 9.1° at last follow-ups. Loss of reduction was 1.8%, 1.5%, 1.4% and 0.2°. Mean VAS pain score was 8.5 before surgery, decreased to 2.5 immediately after operations and was maintained at 2.7 at last follow-ups. Changes in vertebral body heights from immediately after operations to the last follow-ups were analyzed using the Student's paired t-test. Statistical analysis showed a significant reduction in mean kyphotic angle (p=0.03) but no difference of VAS scores (p=0.056). Anterior, middle and posterior body heights decreased with statistical significance between these two times (p<0.001). The one-sample t-test was used to compare the results of the present study with the results obtaioned by Berlemann et al.2) who used bilateral balloon kyphoplasty. Preoperative kyphosis, reductions in kyphosis and percentage reductions were not statistically significant (p=0.6265, 0.5582, 0.9082). The PMMA leakage occurred in 3 cases, but it did not cause neurologic deficits. No adjacent vertebra fractures occurred.
Osteoporosis is defined as a diminished bone density of 2.5 standard deviations below the average bone density of healthy 25 year olds of the same sex. Using this criterion, 25% of postmenopausal women and 35% of women over 65 years of age in the United States suffer from osteoporosis1). The incidence of osteoporotic spine fractures in the United States is about 700,000 per year, of which more than one third are associated with chronic pain and 85% of these cases are due to primary osteoporosis3,15). Osteoporotic VCFs are an important cause of back pain and kyphotic deformity in the elderly. Osteoporotic VCFs occurs most commonly at the thoracolumbar junction, especially L111,12). Pain from acute osteoporotic vertebral compression fractures usually resolves over 6 to 8 weeks with conservative treatment, including medical and orthotic treatments. However, a few patients continue to complain of severe back pain, especially during motion of the trunk, and resultant kyphotic deformity. Such patients who are unresponsive to nonoperative treatment may be candidates for surgical treatment.
Vertebroplasty was developed during the late 1980s and Lapras first introduced this technique to treat fractured vertebra bodies10). Subsequently, it has gained wide acceptance for the treatment of osteoporotic verterbral compression fractures. In 2001, the first report on balloon kyphoplasty issued by Lieberman et al. Balloon kyphoplasty has several advantages over the vertebroplasty13,14) i.e. it offers immediate pain relief, stability and restores local kyphosis by reducing the fractured vertebrae with an inflatable bone tamp. In addition, more viscous PMMA is introduced under low pressure into the cavity made by the inflatable bone tamp, and as a result the rate of complications associated with this technique, such as, thromboembolism, and neurologic deficits due to extravertebral PMMA leakage are low. For this reason, balloon kyphoplasty has become popular. Moreover, nowadays, the indications for balloon kyphoplasty have expanded to pathologic fractures and even more revised cases6,15).
Several authors have reported the results for balloon kyphoplasty executed under general anesthesia4,5,11). However as mentioned above, all patients enrolled in the present study were debilitated (more than ASA grade III), and thus, operations were performed under local anesthesia. Also, during our earlier experiences of the technique, we treated patients using the bilateral approach under local anesthesia. However, when we tried to create access channels using the bone tamp, many patients complained of severe pain that was not controlled by local anesthetics or even parenteral sedatives and thus, we adopted unilateral approach to reduce pain. In the present study, all procedures were executed under local anesthesia.
Some authors have reported the results for the bilateral approach2,7,9). Garfin et al. reported that two balloons are usually used to provide en masse reduction7). However, on comparing results for the bilateral approach with those of present study, we found that results were similar. Several authors have reported that the clinical results of balloon kyphoplasty were not always positively correlated with the restoration of height or amount of PMMA intorduced2).
Figures and Tables
References
1. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Repport of a WHO study group. World Health Organ Tech Rep Ser. 1994. 843:1–129.
2. Berlemann U, Franz T, Orler R, Heini PF. Kyphoplasty for treatment of osteoporotic vertebral fractures: a prospective non-randomized study. Eur Spine J. 2004. 13:496–501.

3. Cooper C, Atkinson EJ, O'Fallon WM, Melton LJ 3rd. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res. 1992. 7:221–227.

4. Coumans JV, Reinhardt MK, Lieberman IH. Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg. 2003. 99:44–50.

5. Crandall D, Slaughter D, Hankins PJ, Moore C, Jerman J. Acute versus chronic vertebral fractures treated with kyphoplasty: early results. Spine J. 2004. 4:418–424.
6. Gaitanis IN, Hadjipavlou AG, Katonis PG, Tzermiadianos MN, Pasku DS, Patwardhan AG. Balloon kyphoplasty for the treatment of pathological vertebral compressive fractures. Eur Spine J. 2005. 14:250–260.

7. Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fracture. Spine. 2001. 26:1511–1515.
8. Greendale GA, Barrett-Connor E, Ingles S, Haile R. Late physical and functional effects of osteoporotic fractures in women: the Rancho Bernado study. J Am Geriatr Soc. 1995. 43:955–961.
9. Grohs JG, Matzner M, Trieb K, Krepler P. Minimal invasive stabilization of osteoporotic vertebral fractures: a prospective nonrandomized comparison of vertebroplasty and balloon kyphoplasty. J Spinal Disord Tech. 2005. 18:238–242.
10. Lapras C, Mottolese C, Deruty R, Lapras C Jr, Remond J, Duquesnel J. Percutaneous injection of methyl-metacrylate in osteoporosis and severe vertebral osteolysis (Galibert's technic). Ann Chir. 1989. 43:371–376.
11. Ledlie JT, Renfro M. Balloon kyphoplasty: one-year outcomes in vertebral body height restoration, chronic pain and activity levels. J Neurosurg Spine. 2003. 98:36–42.

13. Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of "kyphoplasty" in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001. 26:1631–1638.

14. Na HY, Cho HW, Kim SK, Lee SY. Comparison of outcome between percutaneous vertebroplasty and kyphoplasty for osteoporotic painful vertebral compression fracture: a preliminary report. J Korean Soc Spine Surg. 2003. 10:127–136.
15. Yoon ST, Qureshi AA, Heller JG, Nordt JC 3rd. Kyphoplasty for salvage of a failed vertebroplasty in osteoporotic vertebral compression fractures: case report and surgical technique. J Spinal Disord Tech. 2005. 18:Suppl. S129–S134.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download