Abstract
Purpose
To retrospectively analyze the clinical presentations, radiographic findings, and surgical results of type I and II acute necrotizing fasciitis of the low extremity.
Materials and Methods
From April 1998 to March 2005, 13 patients who underwent surgery for the necrotizing fasciitis were reviewed. At the initial diagnosis, 6 patients were diagnosed with cellulitis and 3 patients were diagnosed correctly with necrotizing fasciitis. The underlying diseases, affected sites, official readings of MRI, the intervals between the onset of symptom and surgery, the duration of admission, and complications were investigated.
Results
The underlying diseases were 3 cases of diabetes, 3 cases of liver disease, 1 case of alcoholism and 1 case of cervical cancer with chemotherapy. Regarding the location of the disease, 5 cases were observed below the knees, and 8 cases were observed above the knees. Five out of 9 cases who underwent a preoperative MRI study, were diagnosed correctly as necrotizing fasciitis by the radiologist. The average period between onset of symptoms and surgery was 4.8 days. The complications were hip disarticulation in 1 case, below knee amputation in 1 case, toe amputation in 1 case, and a limited range of motion of the knee joint in 1 case. The 9 patients who healed without complications had no limitation in the range of joint motion and daily activity.
Figures and Tables
Fig. 1
The clinical photography of necrotizing fasciitis that developed on both low extremities show erythema, diffuse swelling and dusky skin color changes (arrow). The patient had rapid progression of the infection with migration of the margins of erythema and skin induration from the foot to thigh before surgery. The region of dusky skin color change (arrow) on the foot finally became necrotic and required a skin graft.

Fig. 2
Plain X-ray anteroposterior and lateral images of the left tibia show diffuse soft tissue edema with gas (arrow) lying on the fascia.

Fig. 3
T2-weighted axial and coronal MR images show diffuse edematous changes in the superficial and deep fascia and gas along the posteromedial aspect of the thigh.
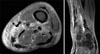
Fig. 4
A 60-year old female had a hysterectomy 2 years ago, and was hospitalized with right leg pain, edema and fever. In the MRI images, necrotizing fasciitis was suspected by the radiologist but her illeness was clinically diagnosed as a unilateral leg lymphedema after the hysterectomy. She was spontaneously restored after conservative treatment.
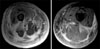
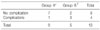
Table 1
Summary of the Associated Diseases, Initial Diagnoses and Clinical Features of the Patients on Admission

References
1. Brothers TE, Tagge DU, Stutley JE, Conway WF, Del Schutte H Jr, Byrne TK. Magnetic resonance imaging differentiates between necrotizing and non-necrotizing fasciitis of the lower extremity. J Am Coll Surg. 1998. 187:416–421.

2. Cawley MJ, Briggs M, Haith LR, et al. Intravenous immunoglobulin as adjunctive treatment for streptococcal toxic shock syndrome associated with necrotizing fasciitis: case report and review. Pharmacotherapy. 1999. 19:1094–1098.

3. Choo SK, Kim BJ, Park GW, Lee YW, Kim HS. Necrotizing fasciitis of the low extremity: A case report. J Korean Orthop Assoc. 2002. 37:822–824.

4. Ellis M. Hyperbaric oxygen can be effective in treating postpartum necrotizing fasciitis type I. J Infect. 2000. 40:292–294.

6. Hahn SB, Kang HJ, Park J. Differential diagnosis and its treatment of gas forming infections. J Korean Fracture Soc. 2002. 15:607–613.

7. Jarrett P, Rademaker M, Duffill M. The clinical spectrum of necrotising fasciitis. A review of 15 cases. Aust N Z J Med. 1997. 27:29–34.

8. Lamothe F, D'Amico P, Ghosn P, Tremblay C, Braidy J, Patenaude JV. Clinical usefulness of intravenous human immunoglobulins in invasive group A Streptococcal infections: case report and review. Clin Infect Dis. 1995. 21:1469–1470.

9. Lee ST, Lee SH, Kim KM, Lee SJ. Necrotizing fasciitis of the low extremity. J Korean Orthop Assoc. 2005. 40:772–777.

10. Loh NN, Ch'en IY, Cheung LP, Li KC. Deep fascial hyperintensity in soft-tissue abnormalities as revealed by T2-weighted MR imaging. Am J Roentgenol. 1997. 168:1301–1304.

11. McHenry CR, Piotrowski JJ, Petrinic D, Malangoni MA. Determinants of mortality for necrotizing soft-tissue infections. Ann Surg. 1995. 221:558–563.

12. McKinnon D, McDonald P. Gas gangrene--a ten-year survey from the Royal Adelaide Hospital. Med J Aust. 1973. 1:1087–1090.
13. Patel R, Rouse MS, Florez MV, et al. Lack of benefit of intravenous immune globulin in a murine model of group A streptococcal necrotizing fasciitis. J Infect Dis. 2000. 181:230–234.

14. Rahmouni A, Chosidow O, Mathieu D, et al. MR imaging in acute infectious cellulitis. Radiology. 1994. 192:493–496.

16. Riseman JA, Zamboni WA, Curtis A, Graham DR, Konrad HR, Ross DS. Hyperbaric oxygen therapy for necrotizing fasciitis reduces mortality and the need for debridements. Surgery. 1990. 108:847–850.
17. Schmid MR, Kossmann T, Duewell S. Differentiation of necrotizing fasciitis and cellulitis using MR imaging. Am J Roentgenol. 1998. 170:615–620.

18. Son GS, Choi IS, Kim KH, Jung KH, Hong YS. MRI for the early diagnosis of necrotizing fasciitis. J Korean Surg Soc. 1997. 52:766–770.
19. Stamenkovic I, Lew PD. Early recognition of potentially fatal necrotizing fasciitis. The use of frozen-section biopsy. N Engl J Med. 1984. 310:1689–1693.
20. Stephens MB. Gas gangrene: potential for hyperbaric oxygen therapy. Postgrad Med. 224. 99:217–220.
22. Tang WM, Ho PL, Fung KK, Yuen KY, Leong JC. Necrotising fasciitis of a limb. J Bone Joint Surg Br. 2001. 83:709–714.

23. VanBeek A, Zook E, Yaw P, Gardner R, Smith R, Glover JL. Proceedings: Nonclostridial gas-forming infections. A collective review and report of seven cases. Arch Surg. 1974. 108:552–557.
24. Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am. 2003. 85:1454–1460.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download