Abstract
Actinomycosis is caused by filamentous Gram positive anaerobic bacteria from the Actinomycetaceae family, and known as a rare cause of the infection at the eyeball. We report magnetic resonance findings of a 60-year-old Korean man with cervicofacial actinomycosis, including cellulitis in the eye and central nervous system actinomycosis. On orbital magnetic resonance imaging, gadolinium-enhanced T1-weight images showed multiple abnormal enhancing lesions in head and neck including right eye, and some include low signal intensities which considered as abscesses. The lesions was diagnosed as actinomycosis by incisional biopsy, and since then was cured by using antibiotics of penicillin family.
Figures and Tables
Fig. 1
T1- (a) T2-wieghted (b), and axial Gadolinium-enhanced T1-weighted magnetic resonance imaging (c, d) scans of orbit showing inflammatory process of the right temporalis muscle (arrow), osteomyelitis of the right sphenoid bone (arrow head), slit like abscess at the right upper eyelid (open arrow) and inflammatory process of the right optic canal (open arrow head).
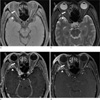
Fig. 2
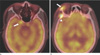
Positron emission tomography scans showing multifocal intensity hypermetabolic lesions in (a) right optic canal (arrow) (b) right upper eyelid (arrow) and right sphenoid bone (arrow head).
References
1. Acevedo F, Baudrand R, Letelier LM, Gaete P. Actinomycosis: a great pretender. Case reports of unusual presentations and a review of the literature. Int J Infect Dis. 2008; 12:358–336.
2. Wong VK, Turmezei TD, Weston VC. Actinomycosis. BMJ. 2011; 343:d6099.
3. Harvey JC, Cantrell JR, Fisher AM. Actinomycosis: its recognition and treatment. Ann Intern Med. 1957; 46:868–885.
4. Belmont MJ, Behar PM, Wax MK. Atypical presentations of actinomycosis. Head Neck. 1999; 21:264–268.
5. Weese WC, Smith IM. A study of 57 cases of actinomycosis over a 36-year period. A diagnostic 'failure' with good prognosis after treatment. Arch Intern Med. 1975; 135:1562–1156.
6. Nithyanandam S, D'Souza O, Rao SS, Battu RR, George S. Rhinoorbitocerebral actinomycosis. Ophthal Plast Reconstr Surg. 2001; 17:134–136.
7. Wallace RJ Jr, Musher DM. Actinomycosis: an update. Int J Dermatol. 1977; 16:185–187.
8. Smego RA Jr. Actinomycosis of the central nervous system. Rev Infect Dis. 1987; 9:855–865.
9. Pagliani L, Campi L, Cavallini GM. Orbital actinomycosis associated with painful ophthalmoplegia. Actinomycosis of the orbit. Ophthalmologica. 2006; 220:201–205.
10. Ho L, Seto J, Jadvar H. Actinomycosis mimicking anastomotic recurrent esophageal cancer on PET-CT. Clin Nucl Med. 2006; 31:646–647.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download