Abstract
Purpose
In this study, the medication effects of Milnacipran and Pregabalin, as well known as fibromyalgia treatment medicine, in fibromyalgia syndrome patients were compared through the change of BOLD signal in pain related functional MRI.
Materials and Methods
Twenty fibromyalgia syndrome patients were enrolled in this study and they were separated into two groups according to the treatment medicine: 10 Milnacipran (MLN) treatment group and 7 Pregabalin (PGB) treatment group. For accurate diagnosis, all patients underwent several clinical tests. Pre-treated and post-treated fMRI image with block-designed pressure-pain stimulation for each group were obtained to conduct the statistical analysis of paired t-test and two sample t-test. All statistical significant level was less than 0.05.
Results
In clinical tests, the clinical scores of the two groups were not significantly different at pre-treatment stage. But, PGB treatment group had lower Widespread Pain Index (WPI) and Brief Fatigue Inventory (BFI) score than those of MLN treatment group at post-treatment stage. In functional image analysis, BOLD signal of PGB treatment group was higher BOLD signal at several regions including anterior cingulate and insula than MLN treatment group at post-treatment stage. Also, paired t-test values of the BOLD signal in MLN group decreased in several regions including insula and thalamus as known as 'pain network'. In contrast, size and number of regions in which the BOLD signal decreased in PGB treatment group were smaller than those of MLN treatment group.
Conclusion
This study showed that MLN group and PGB group have different medication effects. It is not surprising that MLN and PGB have not the same therapeutic effects since these two drugs have different medicinal mechanisms such as antidepressants and anti-seizure medication, respectively, and different detailed target of fibromyalgia syndrome treatment. Therefore, it is difficult to say which medicine will work better in this study.
Figures and Tables
Fig. 3
Comparison of Pregabalin treatment group (Black) and Milnacipran treatment group (Gray) at pre-treatment (left) and post-treatment (right).

Fig. 4
The regions where the activation area of MLN group is larger than that of PGB group: Cingulate gyrus (a). The regions where the activation area of PGB group is larger than that of MLN group: Superior temporal gyrus (b), Anterior cingulate (c), Insula (d).

Fig. 5
The regions where BOLD signal increased at PGB post-treatment stage: Anterior cingulate (a), Insula (b) and decreased BOLD signal region: Insula (c), Cingulate gyrus (d).

Fig. 6
The regions where the BOLD signal increased at MLN post-treatment stage: Superior frontal gyrus (a), Cingulate gyrus (b) and decreasing BOLD signal regions: Insula (c), Thalamus (d).

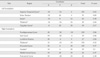
Table 2
Activation Region of MLN Treatment Group is Larger than PGB Treatment Group (p<0.005, Uncorrected for Multiple Comparison)
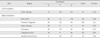
Table 3
Activation Region of PGB Treatment Group Larger than MLN Treatment Group (p<0.005, Uncorrected for Multiple Comparison)

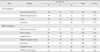
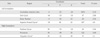
Table 4
Activation Region Increasing BOLD Signal at PGB Post-Treatment (p<0.05, Corrected for Multiple Comparison)

Table 5
Activation Region Decreasing BOLD Signal at PGB Post-treatment (p<0.05, Corrected for Multiple Comparison)
References
1. Wolfe F. Fibromyalgia. Rheum Dis Clin North Am. 1990; 16:681–698.
2. Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995; 38:19–28.
3. Mease P. Fibromyalgia syndrome: review of clinical presentation, pathogenesis, outcome measures, and treatment. J Rheumatol Suppl. 2005; 75:6–21.
4. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990; 33:160–172.
5. Geenen R, Jacobs JW. Fibromyalgia: diagnosis, pathogenesis, and treatment. Curr Opin Anaesthesiol. 2001; 14:533–539.
6. Gracely RH, Geisser ME, Giesecke T, et al. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain. 2004; 127:835–843.
7. Kuchinad A, Schweinhardt P, Seminowicz DA, Wood PB, Chizh BA, Bushnell MC. Accelerated brain gray matter loss in fibromyalgia patients: premature aging of the brain? J Neurosci. 2007; 27:4004–4007.
8. Robinson ME, Craggs JG, Price DD, Perlstein WM, Staud R. Gray matter volumes of pain-related brain areas are decreased in fibromyalgia syndrome. J Pain. 2011; 12:436–443.
9. Schmidt-Wilcke T, Leinisch E, Straube A, et al. Gray matter decrease in patients with chronic tension type headache. Neurology. 2005; 65:1483–1486.
10. D'Esposito M, Detre JA, Aguirre GK, et al. A functional MRI study of mental image generation. Neuropsychologia. 1997; 35:725–730.
11. Logothetis NK, Pauls J, Augath M, Trinath T, Oeltermann A. Neurophysiological investigation of the basis of the fMRI signal. Nature. 2001; 412:150–157.
12. Gracely RH, Petzke F, Wolf JM, Clauw DJ. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 2002; 46:1333–1343.
13. Apkarian AV, Bushnell MC, Treede RD, Zubieta JK. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005; 9:463–484.
14. Williams DA. Psychological and behavioural therapies in fibromyalgia and related syndromes. Best Pract Res Clin Rheumatol. 2003; 17:649–665.
15. Häuser W, Bernardy K, Uçeyler N, Sommer C. Treatment of fibromyalgia syndrome with antidepressants: a meta-analysis. JAMA. 2009; 301:198–209.
16. Üçeyler N, Sommer C, Walitt B, Häuser W. Anticonvulsants for fibromyalgia. Cochrane Database Syst Rev. 2013; 10:CD010782.
17. Kim SH, Lee Y, Lee S, Mun CW. Evaluation of the effectiveness of pregabalin in alleviating pain associated with fibromyalgia: using functional magnetic resonance imaging study. PLoS One. 2013; 8:e74099.
18. Gracely RH, Kwilosz DM. The Descriptor Differential Scale: applying psychophysical principles to clinical pain assessment. Pain. 1988; 35:279–288.
19. Hedberg TG, Stanton PK. Long-term potentiation and depression of synaptic transmission in rat posterior cingulate cortex. Brain Res. 1995; 670:181–196.
20. Beauregard M, Leroux JM, Bergman S, et al. The functional neuroanatomy of major depression: an fMRI study using an emotional activation paradigm. Neuroreport. 1998; 9:3253–3258.
21. Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci U S A. 2001; 98:676–682.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download