Abstract
Purpose
The biceps femoris tendon (BFT) and lateral collateral ligament (LCL) in the knee were formerly known to form a conjoined tendon at the fibular attachment site. However, the BFT and LCL are attached into the fibular head in various patterns. We classified insertion patterns of the BFT and LCL using MR imaging, and analyzed whether the LCL attaches to the fibular head or not.
Materials and Methods
A total of 494 consecutive knee MRIs of 470 patients taken between July 2012 and December 2012 were retrospectively reviewed. There were 224 males and 246 females, and patient age varied from 10 to 88 (mean, 48.6). The exclusion criteria were previous surgery and poor image quality. Using 3T fat-suppressed proton density-weighted axial images, the fibular insertion patterns of the BFT and LCL were classified into following types: type I (the LCL passes between the anterior arm and direct arm of the BFT's long head), type II (the LCL joins with anterior arm of the long head of the BFT), type III (the BFT and LCL join to form a conjoined tendon), type IV (the LCL passes laterally around the anterior margin of the BFT), and type V (the LCL passes posteriorly to the direct arm of the BFT's long head).
A posterolateral stability of the knee is maintained by numerous ligaments, tendons, and muscles including the biceps femoris tendon (BFT) and the lateral collateral ligament (LCL). The BFT functions as an external rotator of the tibia, and provides forceful stability to the knee. There were several previous reports on the distal insertion patterns of the BFT and LCL, and they do not agree with one another. In a radiological study which includes the fibular attachment of the BFT and LCL, these two structures have been reported to form a conjoined tendon that attaches to the fibular head (1). That is, the BFT runs downwards behind the iliotibial tract and the distal portions of the BFT and LCL attach to the fibular head as it forms a conjoined tendon. However, other cadaveric study on this part did not report any conjoined tendon of these two structures. And it reported that the BFT and LCL are attached to the fibular head independently of each other (2). A cadaveric study by Terry et al. (3) also does not report any conjoined tendon of the two structures.
Such cadaveric studies support the argument that the BFT and LCL do not form a conjoined tendon, but they form independent fibular insertions. As we show earlier from the report mentioned above, the attachment pattern of the BFT and LCL is not uniform in different patients. Such anatomic variation may cause confusion in interpreting images of the lateral ligamentous structures of the knee. More accurate understanding of these structures would allow precise radiological assessment of patients with the knee lesions and it would provide a more detailed map for surgeons who plan to do reconstructive operations or repairs in this area.
The authors classified the insertion patterns of the BFT and LCL using MR imaging. We hypothesized that the proportion of patients with conjoined the BFT and LCL would not be predominant, and that there would be additional insertion patterns of these tendons.
This retrospective study was approved by our institutional review board, which waived the need for informed consent. 516 cases of the knee MR's from 492 patients were included in the study from July 2012 to December 2012. Among the 516 cases of the knee MR images, 20 cases were excluded due to prior history of the knee related surgery, and two additional cases were excluded due to poor image quality. The study was proceeded with 494 cases of knee MR's from 470 patients. There were 224 males and 246 females, and the patient age varied from 10 to 88 (mean, 48.6).
Routine knee MR images were acquired with a 3.0-T MR system (Gyroscan Archieva 3.0 Tesla, Philips Medical System International, Best, The Netherlands) using dedicated eight-channel extremity receiver knee coils. The patients were positioned in supine position with their knee in 10° of flexion state (4). The routine MR protocol was set with a 3T proton density (PD) fat suppressed axial (TR/TE, 4036/20; section thickness, 3 mm; number of signals acquired, 1; field of view, 15×15 cm; matrix size, 332×332; echotrain length, 4), T2 TSE sagittal (TR/TE, 3900/100; section thickness, 2.5-mm; number of signals acquired, 1; field of view, 15×15 cm; matrix size, 300×300; echotrain length, 15), PD fat suppressed coronal (TR/TE, 5000/30; section thickness, 2.5-mm; number of signals acquired, 1; field of view, 15×15 cm; matrix size, 300×300; echotrain length, 6), PD TSE sagittal (TR/TE, 5000/30; section thickness, 2.5-mm; number of signals acquired, 1; field of view, 15×15 cm; matrix size, 300×300; echotrain length, 10).
Using mainly the proton density fat suppressed axial images (TR/TE, 4036/20), the distal insertion patterns of the BFT and LCL of 494 knee MR images were classified into five types by the two radiologists in consensus. In type I, the LCL passes obliquely between the anterior and direct arm of the long head of the BFT. In type II, the anterior arm of the long head of the BFT joins with the LCL. In type III, the BFT and LCL join to form a conjoined tendon. In type IV, the LCL passes laterally around the anterior margin of the BFT. In type V, the LCL passes posteriorly to the direct arm of the long head of the BFT (Fig. 1).
When a patient had taken MR images on both knees, the insertion types of both knees were recorded. In total, 24 patients had MR images taken on both knees.
While classifying the insertion types of the BFT and LCL, we found some cases in which the LCL was not inserted into the fibular head. Thus we added another item to our database to record whether the LCL is inserted into the fibular or not.
In the 494 cases of the knee MR images, there were 433 (87.65%) type I cases, 21 (4.25%) type II cases, 2 (0.4%) type III cases, 16 (3.23%) type IV cases, and 22 (4.45%) type V cases. The majority was type I, and there were only two cases in which the BFT and LCL formed a conjoined tendon (Figs. 2,3,4,5,6).
Among the 24 patients who had imaged both sides of knees, 18 (75%) had the same insertion type in both knees. two patients of these 18 (2/18, 11%) were type I, 15 (15/18, 83%) were type II, and 1 (1/18, 5.5%) was type VI. Six patients among the 24 with both knee MR images (25%) had different types in each knee (two patients each with type II & III, type I & II, and type II & VI).
In 26 out of 494 cases of knee MR images (5.26%), the BFT and LCL were not attached to the fibular head (Fig. 7). Of these 26 cases, 22 were type I (22/494, 4.45%), 3 were type II (3/494, 0.006%), and 1 was type IV (0.002%).
The fibular attachment site of the BFT and LCL is not a site with a high incidence of disease or trauma, and there are no reports about the fibular insertion site and the surrounding area (5). However, the recent advancements in MR imaging with thin sections and improved image quality made it possible to observe the fibular insertion patterns of the BFT and LCL in greater detail.
It was generally known that BFT and LCL form a conjoined tendon to attach to the fibular head (1, 6). However, results from cadaveric studies on BFT and LCL insertions argue differently (2, 3, 5, 7, 8). According to Sneath et al. (2), 48 cadaveric knee dissections show that the BFT divides into multiple fibers that that attaches to the fibular head independently from the LCL. They stated that the BFT is divided into two portions. One of the portions is attached to the fibula. And the other divides once again into 4 laminae to conjoin with the LCL or attached to the tibial lateral condyle. Later, Terry et al. stated that the BFT is consists of a long head and a short head (3). They reported that the long head divides once again into a direct arm and an anterior arm, both of which attaches to the fibular head. The direct arm of the short head (lateral and posterior tendinous part) is attached to the fibular head, while the anterior arm had a tibial insertion. As stated by the studies above, the BFT does not simply form a conjoined tendon with the LCL to attach to the fibula, but it divides into multiple portions that are separated from the LCL and attaches mostly into the fibula, with some inserting into the tibia.
In a study that correlated such cadaveric studies with axial MR images, five specimens out of seven showed that the direct and anterior arms of the long head of the BFT and the direct arm of the short head of the BFT were separated as discrete components near the fibular attachment site (3). Also, in this cadaveric study, LCL was located relatively medially to the anterior arm and direct arm of the long head of the BFT. This is consistent with the MR findings shown in our study. There was no other significant MR imaging study about the fibular attachment of the BFT.
The authors tried to find out the various distal insertion patterns of the BFT and LCL using a large number of knee MR images (494). Based on previous studies(2, 3, 5, 7, 8), each arm of the BFT could be observed as separate structures in all cases. After analysis of the MR images, the insertion patterns of the LCL and the two arms of the BFT could be grouped into five different types. Type I (LCL passes between the anterior and direct arms of the long head of the BFT) was found to be the most common type, and the type in which the BFT and LCL attached to the fibular head as a conjoined tendon was observed the least frequently. Thus we can conclude that according to analysis with MR images, the insertion pattern of the BFT and LCL exists in various forms and the conjoined tendon previously known is very rarely seen.
Discovery of the five different MRI patterns described in the results would open venues for further researches for anatomical confirmation of the different patterns. If the MRI patterns are confirmed by anatomic studies, physicians in the field could find the clinical implications of each different patterns.
In 26 cases out of 494 cases of knee MR images (5.26%), the LCL was not attached to the fibular head. Instead, the LCL passed the fibular head laterally in an aponeurosis form (Fig. 7). There has not been any anatomical report yet that could describe this kind of variant of the LCL insertion (9).
Our study is limited by the following points: First, analysis was performed using only MR images and no other imaging modalities were included. Second, only images were chosen to study and no actual cadaveric study was done to confirm the findings observed in MR images. Third, this report documents only the discovery of five different patterns of the BFT and LCL tendons. Clinical differences among the five types are yet to be explored. However, future clinical studies based on this report would allow more detailed understanding of the pathophysiology in the posterolateral corner of the knee.
In conclusion, the previously known conjoined tendon at the fibular attachment of the BFT and LCL was actually very rare to exist. Fibular attachment pattern of the BFT and LCL shows various types in MR imaging. Understanding of such anatomic variations will be useful when evaluating anatomic structures in this area.
Figures and Tables
Fig. 1
Fibular insertion of the BFT and LCL, alB: anterior arm of the BFT's long head, dlB: direct arm of the BFT's long head, dsB: direct arm of the BFT's short head.
(a) Type I, the LCL passes between the anterior arm and direct arm of the BFT's long head.
(b) Type II, LCL joins with the anterior arm of the BFT's long head.
(c) Type III, the BFT and LCL join to form a conjoined tendon.
(d) Type IV, the LCL passes laterally around the anterior margin of the BFT.
(e) Type V, the LCL passes posteriorly to the direct arm of the BFT's long head.

Fig. 2
28-years-old female, type I.
3T proton density fat suppressed axial image (TR/TE, 4036/20). LCL (arrowhead) passes between the anterior arm (open arrow) and direct arm (solid arrow) of the BFT's long head.
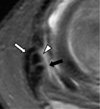
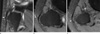
Fig. 3
12-years-old male, type II.
(a, b) 3T proton density fat suppressed axial image (TR/TE, 4036/20). The anterior arm (open arrow) of the BFT's long head joins with LCL (arrowhead). The solid arrow indicates the direct arm of the BFT's long head.
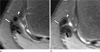
Fig. 4
52-years-old male, type III.
(a) 3T proton density fat suppressed axial image (TR/TE, 4036/20). BFT (open arrow) is not divided into separate arms, and forms a fused mass. The arrowhead indicates the LCL. (b) In a lower level, BFT and LCL joins and forms a conjoined tendon (stripe arrow).
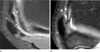
Fig. 5
61-years-old male, type IV.
3T proton density fat suppressed axial image (TR/TE, 4036/20). LCL (arrowhead) passes laterally to the anterior arm (open arrow) of BFT. The solid arrow indicates the direct arm of long head of BFT. Stripe arrow indicates fibula.
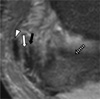
Fig. 6
64-years-old female, type V.
3T proton density fat suppressed axial image (TR/TE, 4036/20). LCL (arrowhead) passes posteriorly to the direct arm (solid arrow) of long head of BFT. Stripe arrow indicates tibia.
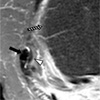
Fig. 7
28-years-old male patient without fibular insertion of the LCL.
(a) Proton density (PD) fat suppressed coronal image (TR/TE, 5000/30) and (b) axial image show LCL (arrowhead) passing the fibular head without attachment. (c) In a lower level, axial image show LCL (arrowhead) passing the fibular head laterally in an aponeurosis form.
References
1. Recondo JA, Salvador E, Villanúa JA, Barrera MC, Gervás C, Alústiza JM. Lateral stabilizing structures of the knee: functional anatomy and injuries assessed with MR imaging. Radiographics. 2000; 20:S91–S102.
2. Sneath RS. The insertion of the biceps femoris. J Anat. 1955; 89:550–553.
3. Terry GC, LaPrade RF. The biceps femoris muscle complex at the knee. Its anatomy and injury patterns associated with acute anterolateral-anteromedial rotatory instability. Am J Sports Med. 1996; 24:2–8.
4. Pereira ER, Ryu KN, Ahn JM, Kayser F, Bielecki D, Resnick D. Evaluation of the anterior cruciate ligament of the knee: comparison between partial flexion true sagittal and extension sagittal oblique positions during MR imaging. Clin Radiol. 1998; 53:574–578.
5. Munshi M, Pretterklieber ML, Kwak S, Antonio GE, Trudell DJ, Resnick D. MR imaging, MR arthrography, and specimen correlation of the posterolateral corner of the knee: an anatomic study. AJR Am J Roentgenol. 2003; 180:1095–1110.
6. DeLee JC, Riley MB, Rockwood CA Jr. Acute posterolateral rotatory instability of the knee. Am J Sports Med. 1983; 11:199–207.
7. Tubbs RS, Caycedo FJ, Oakes WJ, Salter EG. Descriptive anatomy of the insertion of the biceps femoris muscle. Clin Anat. 2006; 19:517–521.
8. Espregueira-Mendes , da Silva MV. Anatomy of the lateral collateral ligament: a cadaver and histological study. Knee Surg Sports Traumatol Arthrosc. 2006; 14:221–228.
9. Solomon LB, Stevenson AW. Tibial insertion of the biceps femoris tendon: anatomical and radiological description of an anatomical variant. Clin Anat. 2008; 21:802–804.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download