Abstract
Purpose
To determine the incidence of truncated triangle appearance of anterior horn (AH) to body of medial meniscus (MM) and determine its clinical significance.
Materials and Methods
IRB approval was obtained, and informed consent waived for this study. The criteria of "pseudoradial tear" was truncated triangle appearance of the tip of AH to body of MM on one or more coronal images with adjacent fluid signal intensity at the blunted tip. Two musculoskeletal radiologists retrospectively evaluated 485 knee MR images independently for the presence and number of sections with "pseudoradial tear" of AH to body of MM using proton density-weighted coronal MR images. Inter-and intraobserver agreement was calculated using kappa coefficients. Medical records were reviewed for arthroscopic correlation.
Results
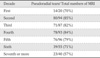
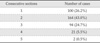
A pseudoradial tear in the AH to body of MM was present in 381 (78.6%) patients. Locations were 112 in AH (29.4%), 143 in AH to body (37.5%), and 126 in body (33.1%). Number of consecutive sections of pseudoradial tear were 1 in 100 (26.2%), 2 in 164 (43.0%), 3 in 94 (24.7%), 4 in 21 (5.5%), and 5 in 2 (0.5%). Interobserver agreement was 0.99 for presence and 0.43 for number of sections of pseudoradial tear. Arthroscopies were performed in 96 patients and none of the pseudoradial tears were proven as true radial tears on arthroscopy.
MR imaging of the knee is sensitive for the demonstration of meniscal tears, but discrepancies between MR imaging and arthroscopy still remain (1, 2, 3, 4, 5). Although high accuracy of detection of tears has been shown, normal anatomic structures of the knee may simulate meniscal tears and may be common sources of false-positive diagnosis of internal derangements (6, 7, 8). These potential pitfalls in interpretation may be caused by structures with low signal intensity; such as the transverse ligament, the meniscofemoral ligament, and the popliteus tendon; and by volumeaveraging artifact due to the concavity of the outer margin of the meniscus. These structures potentially mimic variable appearance meniscal tear (6, 7, 8); transverse ligament can stimulate oblique or vertical tear of anterior horn of meniscus, meniscofemoral ligament can stimulate vertical tear of posterior horn of lateral meniscus, while popliteus tendon can mimic oblique tear of posterior horn of lateral meniscus.
In everyday practice of reading knee MR images, we encountered a truncated triangle-like blunting of the tip of the meniscus at the anterior horn, oftentimes only on coronal images, on evaluation of knee MRIs over the years, which we frequently gave the reading of "suspicious radial tear"; these were not always seen on other sequences. However, after arthroscopy for other pathologies, the results showed that these were not true radial tears.
To our knowledge, there has been no previous report about this finding of a truncated triangle appearance "pseudoradial tear" at the anterior horn to body of the medial meniscus on coronal MR images, which could be a potential pitfall and should be differentiated from true radial tear.
Being aware of the normal variation in this region, preoperative diagnostic accuracy of radial tears may improve and false positive diagnosis of radial tears should decrease, thereby avoiding unnecessary surgery.
The purpose of this study was to determine the incidence of truncated triangle appearance of anterior horn to body of the medial meniscus and determine its clinical significance.
485 consecutive sets of MRI examinations of the knee performed between January and December 2011 at our institution were reviewed retrospectively. The age range of the 485 patients was 3-84 years (277/208 men/women; mean, 34.5 years). All patients underwent MRI of the knee in coronal, axial, and sagittal planes on a 1.5-T Intera scanner (Philips medical systems, Best, the Netherlands) and 3.0-T Achieva scanner (Philips medical systems, Best, the Netherlands) with a knee coil. Each 1.5-T study consisted of coronal and sagittal proton density-weighted (PDW) (TR/TE, 3000/20), sagittal T1-weighted (T1W) (400/10), sagittal fat saturated T2-weighted (T2W) (2300/50), and axial fat saturated PDW (2700/12) images. Each 3.0-T study consisted of coronal and sagittal turbo spin-echo (TSE) PDW (2600/10), sagittal spectral presaturation inversion recovery (SPIR) T2W (2500/60), sagittal TSE T1W (580/10), and axial SPIR PDW (3200/20) images. Imaging parameters were as follows: FOV 150-160 mm, Slice thickness 3 to 4 mm with a 10% interslice gap, ETL= 3 for T1W, 10 for PDW, 12 for all other sequences; 272×272 matrix for sagittal images, 400×384 matrix for the coronal images.
Two musculoskeletal radiologists evaluated the MR images. After consensus training session, all cases were reviewed in a blinded retrospective fashion with special attention to the appearance of the anterior horn to body of the medial meniscus for the presence of truncated triangle appearance, blinded to the clinical information. The MR imaging criteria of "pseudoradial tear" was truncated triangle appearance of the tip of anterior horn to body of the medial meniscus on one or more coronal MR images and/or adjacent fluid signal intensity at the blunted tip on proton density or T2-weighted images (Figs. 1 and 2). In case of ambiguity, T2-weighted fast spin-echo sequences were analyzed. Sagittal and axial sequences were also checked to exclude true radial tears.
We excluded the first consecutive image immediately after the insertion site of following transverse ligament of anterior horn of the medial meniscus, which could cause an artifact at the meniscal tip due to partial volume (9). The following were evaluated: 1) the presence of pseudoradial tear at the anterior horn to body of the medial meniscus 2) the incidence according to age group 3) the location of blunted tip 4) the number of consecutive images on which a pseudoradial tear was present in each case. We excluded the following cases: patients with prior meniscal surgery, underlying meniscal degeneration, contusion, or tear in the anterior horn and/or anterior horn to body of the meniscus, tibial plateau fracture, difficult meniscal evaluation due to excessive large field of view (more than 200 mm) or artifacts hindering proper evaluation.
MR imaging findings were correlated with arthroscopy reports to determine the exact location and extent of any medial meniscal tears. Arthroscopies were performed by an experienced arthroscopic surgeon with full knowledge of MRI findings in 96 patients. The surgeon made note of the exact location of each meniscal tear detected using meniscal diagrams completed immediately after surgery.
Inter- and intra-observer agreements were calculated using kappa coefficients.
In the 485 consecutive MR examinations, a pseudoradial tear (Figs. 1, 2) in the anterior horn to body of the medial meniscus was present in 381 (78.6%) patients (221/160 men/women; mean age, 33.5 years). The incidence according to age group (Table 1), location (Table 2), and number of consecutive sections (Table 3) of the pseudoradial tear of the medial meniscus are listed in Tables. The incidence of truncated triangle appearance of medial meniscus was 80.1% (177/221) on 4-mm slice thickenss 1.5T MRI examination and 77.3% (204/264) on 3-mm slice thickness 3.0T MRI examination; there was no significant difference in the incidence between the two groups (P > 0.05).
Arthroscopic results were as follows: among the total 96 patients, normal medial meniscus was found in 65 cases (67.7%), medial meniscus tears in 31 cases (32.3%); 2 (6.5%) in body, 7 (22.5%) in body to posterior horn, and 22 (71%) in posterior horn. On arthroscopy, anterior horn of medial meniscus was normal in all patients and none of the pseudoradial tears were proven as true radial tears.
Interobserver agreement was almost perfect (kappa value 0.99) for the presence and moderate (kappa value 0.43) for the number of sections of pseudoradial tear. Intraobserver agreement was substantial (kappa value 0.73).
Radial tear involves the meniscal free edge and is perpendicular to the long circumferential axis of the meniscus (10, 11, 12, 13). It needs surgical debridement and/or resection, therefore the diagnosis of a radial tear is important (14). However, sometimes it is difficult to diagnose them preoperatively. Linear defect of a radial tear may not be seen when it is oriented parallel to the plane of the image. Radial tears in the body of the meniscus may be difficult to characterize in the coronal plane alone; additional use of sagittal and axial images allows more accurate characterization of radial tears (15). Small radial tears (or parrot-beak tear) affecting the free margin of the body of the meniscus are often better visualized on thin coronal cross-sections (10).
Usually the slice thickness most likely affects sensitivity in detection of radial tears; smaller section thickness decreases the effect of the volume-averaging artifact seen on thinner sections, which would theoretically result in increased sensitivity for detection of such tears. In our study, there was no perceivable difference in detection of meniscal truncated triangle appearance regarding slice thickness (3 vs. 4 mm), MR field strength (1.5 T vs. 3 T), or the addition of fat suppression to the imaging protocol. The incidence of meniscal truncated triangle appearance was 80.1% on 4-mm thickness 1.5T MRI examination and 77.3% on 3-mm thickness 3.0T MRI examination. There was no significant difference in the incidence between the two groups (P>0.05).
MR imaging criteria used for diagnosis of a radial tear were those outlined by Tuckman et al; truncation, abnormal morphology and/or lack of continuity or absence of the meniscus on one or more MR images (12). An additional criterion used was abnormal increased signal in that area on fat-saturated PD or T2W coronal and sagittal images (15). Other useful radiologic signs were described by Harper et al as follows: truncated triangle, cleft, marching cleft, and ghost meniscus signs (13). Truncation of the meniscal triangle is a useful morphologic sign of a radial tear; however, meniscal truncation is sometimes difficult to differentiate from simple fraying or fibrillation of the meniscus on MR images (1). In a study by Justice et al, false-positive interpretations of tears of the inner third of medial meniscus was found at arthroscopy to be frayed and not frankly torn; differentiation on MRI between meniscal fraying and tears sometimes is impossible (2).
Thus, keys to interpretation of radial tears are recognition of these signs; however, in our study truncated triangle appearance of the anterior horn to body of the medial meniscus were frequently seen on coronal MR images and mimicked true radial tears. In our study, truncated triangle appearance of the anterior horn to body of the medial meniscus was seen on coronal MR images in 381 (78.6%) patients; however, in our study, none of the truncated triangle appearance of the anterior horn to body of the medial meniscus was proven as true radial tears on arthroscopy. From the results of our study, we suggest that this relatively common and potentially confusing finding may be called a "pseudoradial tear" and may be another pitfall to be aware of and be differentiated from true radial tears.
There are several limitations to our study, first of which is the retrospective design. Secondly, arthroscopically confirmed cases were relatively small (96 cases) but there was no rationale for making patients undergo arthroscopy, if they had no definite evidence of internal derangement of the knee. Another limitation of this study was the absence of size quantification of truncated triangle appearance of the medial meniscus, i.e. we did not measure the widths of the blunted portion of the meniscal tip. However, measurement of exact width of blunted meniscal portion on coronal MR image was difficult because meniscal blunting was seen as an abrupt termination at the meniscal tip.
In conclusion, truncated triangle appearance of the tip of anterior horn to body of the medial meniscus on one or more coronal MR images and/or adjacent fluid signal intensity at the blunted tip on PD or T2W images, so called "pseudoradial tear", mimicking a true radial tear was frequently seen on coronal MR images. Awareness of this pitfall in this region should improve preoperative diagnostic accuracy of radial tears, thereby avoiding unnecessary surgery.
Figures and Tables
Fig. 1
Pseudoradial tear at the junction of anterior horn to body of the medial meniscus in a 11-year-old girl on proton densityweighted spectral presaturation inversion recovery (SPIR) coronal image (TR/TE, 2718/7.617; 3-mm section thickness) shown as blunting of the tip of the medial meniscus (arrow). Meniscus was intact at arthroscopy.

Fig. 2
Pseudoradial tear at the junction of anterior horn to body of the medial meniscus in a 39-year-old women on proton density-weighted coronal image (TR/TE, 2651/12; 4-mm section thickness) shows adjacent fluid signal intensity at the blunted tip of the medial meniscus (arrow). Meniscus was intact at arthroscopy.

Acknowledgements
This paper has been supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (NRF-2012R1A1A3010896).
References
1. Magee T, Shapiro M, Williams D. MR accuracy and arthroscopic incidence of meniscal radial tears. Skeletal Radiol. 2002; 31:686–689.
2. Justice WW, Quinn SF. Error patterns in the MR imaging evaluation of menisci of the knee. Radiology. 1995; 196:617–621.
3. De Smet AA, Tuite MJ, Norris MA, Swan JS. MR diagnosis of meniscal tears: analysis of causes of errors. AJR Am J Roentgenol. 1994; 163:1419–1423.
4. De Smet AA, Nathan DH, Graf BK, Haaland BA, Fine JP. Clinical and MRI findings assciated with false positive knee MR diagnoses of medial meniscal tears. AJR Am J Roentgenol. 2008; 191:93–99.
5. De Smet A, Graf B. Meniscal tears missed on MR imaging: relationship to meniscal tear patterns and anterior cruciate ligament tears. AJR Am J Roentgenol. 1994; 162:905–911.
6. Watanabe AT, Carter BC, Teitelbaum GP, Seeger LL, Bradley WG. Normal variations in MR imaging of the knee: appearance and frequency. AJR Am J Roentgenol. 1989; 153:341–344.
7. Vahey TN, Bennett HT, Arrington LE, Sholboumo KD, Ng J. MR imaging of the knee: pseudotear of the lateral meniscus caused by the meniscofemoral ligament. AJR Am J Roentgenol. 1990; 154:1237–1239.
8. Herman LJ, Beltran J. Pitfalls in MR Imaging of the knee. Radiology. 1988; 167:775–781.
9. Pusey E, Lufkin RB, Brown RK, et al. Magnetic resonance imaging artifacts: mechanism and clinical significance. Radiographics. 1986; 6:891–911.
10. Firooznia H, Golimbu C, Rafi M. MR imaging of the menisci. Fundamentals of anatomy and pathology. Magn Reson Imaging Clin N Am. 1994; 2:325–347.
11. Jee WH, McCauley TR, Kim JM, et al. Meniscal tear configurations: categorization with MR imaging. AJR Am J Roentgenol. 2003; 180:93–97.
12. Tuckman GA, Miller WJ, Remo JW, Fritts HM, Rozansky MI. Radial tears of the menisci: MR findings. AJR Am J Roentgenol. 1994; 163:395–400.
13. Harper KW, Helms CA, Lambert HS 3rd, Higgins LD. Radial meniscal tears: significance, incidence, and MR appearance. AJR Am J Roentgenol. 2005; 185:1429–1434.
14. Messner K, Gao J. The menisci of the knee joint: anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998; 193:161–178.
15. Magee T, Williams D. Detection of meniscal tears and marrow lesions using coronal MRI. AJR Am J Roentgenol. 2004; 183:1469–1473.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download