Abstract
Purpose
Materials and Methods
Results
Figures and Tables
Fig. 1

Fig. 2
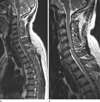
Fig. 3

Fig. 4

Table 2

Note.- CT SAG T2WIs: cervicothoracic spine sagittal T2-weighted images, SCS: spinal canal stenosis, IM-T2-HIS: intramedullary T2-high signal intensity, DH: disc herniation, CSF: cerebrospinal fluid, †Among 139 patients, 3 patients with disc herniation concurrently had block vertebrae (n = 2) and syrinx (n = 1)
Table 3

Note.- CT SAG T2WIs: cervicothoracic spine sagittal T2-weighted images, LBP: lower back pain, RP: radiating pain, SCS: spinal canal stenosis, OPLL: ossification of the posterior longitudinal ligament, OLF: ossification of the ligamentum flavum, IM-T2-HIS: intramedullary T2-high signal intensity, DH: disc herniation, ACDF: anterior cervical discectomy and fusion, TDR: total disc replacement, CSF: cerebrospinal fluid, SIH: spontaneous intracranial hypotension, Fx: fracture




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download