Abstract
Nocardiosis is an uncommon Gram-positive bacterial infection caused by aerobic actinomycetes in the genus Nocardia. Nocardia spp. have the ability to cause localized or systemic suppurative disease in humans and animals. Nocardiosis is typically regarded as an opportunistic infection, but approximately one-third of infected patients are immunocompetent. We report a rare case of pulmonary nocardiosis and a brain abscess caused by Nocardia asteroides in an elderly woman with a history of Crohn's disease. Radiographic imaging revealed a contrast-enhancing lesion with perilesional parenchymal edema that was preoperatively thought to be a neoplasm. The patient experienced aggressive disease progression simulating a metastatic brain tumor. Early diagnosis of norcadiosis, the absence of underlying disease, and the administration of appropriate antibiotics has a positive impact on prognosis. Familiarity with the magnetic resonance and computed tomography findings associated with CNS nocardiosis, such as those presented here, is essential for making an early diagnosis.
Nocardia brain abscess is a rare central nervous system (CNS) infection that carries a high mortality rate reaching 33% which is considered the highest amongst brain abscesses caused by microorganisms (1, 2). In brain abscess, nocardiosis is a rare intracranial lesion and mostly has been reported in immunocompromised patients that presents cruel disease progression. All available literature is a single case reports or small case series. An optimal treatment option has not been established. However, early diagnosis and appropriate antimicrobial therapy are very important factors for a good outcome.
We report a rare case of pulmonary nocardiosis and a brain abscess caused by Nocardia asteroides in an elderly woman with a history of Crohn's disease. The patient experienced aggressive disease progression, simulating a metastatic brain tumor. She underwent a surgical biopsy of brain mass to differentiation of tumor and infection. After Nocardia Asteroides was seen on Gram's stain and subsequently identified by culture, appropriate antibiotic therapy was initiated.
A 77-year-old woman presented with dyspnea for 1 week and confused mental state for 2 days. She had Crohn's disease and diabetes mellitus, and had been treated with long-term mesalazine and prednisone. At admission, her temperature was 37.1℃ with 80% oxygen saturation when breathing ambient air. Physical and neurological examinations were unremarkable. Laboratory analyses yielded the following: leukocytosis (white blood cell [WBC] count, 15300/uL; 96.3% neutrophils, 2.2% lymphocytes), elevated erythrocyte sedimentation rate (75 mm/h in the first hour), and elevated C-reactive protein (CRP) level (11.0). Chest computed tomography (CT) revealed a consolidative lesion with inner necrosis and multiple nodules in the left upper lobe (LUL) of the right lung. Fluid collection in the pleural space and left lower lobe (LLL) collapse were observed, which were suggestive of obstructive pneumonitis (Fig. 1). We recommended a percutaneous transthoracic needle biopsy (PTNB) to exclude lung cancer.
An initial non-contrast-enhanced CT scan of the brain revealed low attenuation of the right frontal white matter (Fig. 2). Subsequently, a contrast-enhanced axial MR image of the brain revealed a small, ill-defined, T1-low and T2-high signal intensity lesion in the right frontal white matter; a ring-enhancing lesion of approximately 8 mm was observed within this lesion following contrast infusion (Fig. 3). The initial diagnosis was a metastatic intra-axial neoplasm and so a surgical intervention was planned.
First, CT-guided PTNB was performed targeting the localized, round, consolidative lesion in the RLL, and a pinkish fresh specimen was obtained that showed some necrosis. The initial pathology report described a necrotizing granulomatous inflammation with fibrosis and a few branching fungal organisms, which suggested invasive aspergillosis (Fig. 5a). Tests for acid-fast bacilli and Gram stains were negative. Follow-up examination revealed leukocytosis and increased CRP. The patient also reported dyspnea and headache. At that time, a follow-up contrast-enhanced chest CT scan showed aggravation of the nodular consolidation and necrosis, and an enlarged mass. The right pleural effusion was also increased despite percutaneous catheter drainage.
Two weeks after the initial brain MRI, a contrast-enhanced axial MR image of the brain revealed that the peripheral enhancing mass in the right frontal lobe had become enlarged, and a new lesion was detected in the right parietal lobe with focal diffusion restriction (Fig. 4). Under the suspicion of malignancy, we performed a right craniotomy by using a computer-assisted stereotactic neuro-navigation system. When the dural incision was made in the right frontal lobe, a mass with internal gray-green pus was found. A dissection plane was created between the lesion and the edematous brain tissue, and the abscess, including the capsule, was completely excised. Microscopic examination of the lesion revealed a thick zone of granulation tissue composed of collagen, fibroblasts, and chronic inflammatory cells surrounding a central abscess cavity (Fig. 5b). Gomori methenamine silver (GMS) and Gram staining of the abscess revealed long, branching, Gram-positive filamentous rods morphologically similar to Nocardia species (Fig. 5c). GMS staining of the pathologic slide containing the lung tissue biopsy specimen obtained during the preceding PTNB revealed the same branching, filamentous microorganisms.
An early post-operative CT scan confirmed complete removal of the lesion. Except for an erythrocyte sedimentation rate of 44 mm/h, all of the patient's other laboratory parameters were normal. Treatment with parenteral ceftriaxone and amikacin was initiated post-operatively, and was continued for 6 weeks. The patient was then discharged, asked to continue bactrim administration, and followed-up as an outpatient. At her 6-month follow-up visit, she was able to stand and walk a few steps with assistance and to speak simple words. Her higher mental functions, including memory, attention, language skills, problem solving, and emotional state, were all improving.
Nocardia asteroides was first described in animals by Nocard (1888), and its presence in a human brain abscess was reported by Eppinger (1890). Nocardia are Gram-positive, partially acid-fast, aerobic, and branching filamentous bacteria. Three species that are human pathogens have been described: Nocardia asteroides, N. brasiliensis, and N. caviae. N asteroides is the most frequently encountered (1).
A Nocardia infection involving the CNS may manifest from meningitis, diffuse cerebral infiltration without localization, granuloma with giant cells, or cerebral abscesses (2, 3).
Nocardia cerebral abscesses are rare and generally occur in immunocompromised patients. They account for only 2% of brain abscesses (2). Mamelak et al. reported that while the mortality rate among immunocompromised patients with a Nocardia cerebral abscess is 55%, it is 20% in immunocompetent patients (4). Initially, such abscesses were diagnosed as primarily neoplastic, including high-grade astrocytomas, metastasis, or lymphomas (5-7).
In our case, radiographic imaging revealed a contrast-enhancing lesion with perilesional parenchymal edema that was preoperatively diagnosed as a neoplasm such as metastasis or primary brain malignancy. Initially, the mass detected on the chest CT scan was thought to be lung cancer. The distinction between a tumor and an abscess is very important, especially with respect to a potential Nocardia infection. Our patient developed a severe CNS infection in the form of cerebritis, a brain abscess, and ventriculitis. The course of the disease was very serious, and the clinical condition of the patient deteriorated rapidly.
On the image shown, the low signal intensity rim of the lesion on the T2-weight image could be related to the presence of methemoglobin in the wall of the capsule or to the production of free radicals by macrophages (8).
The antibiotic of choice for the treatment of such infections is the synergistic combination of trimethoprim and sulfamethoxazole (4, 9). The regimen should be maintained for at least 6 weeks and should initially be administered intravenously and then orally for a long period of up to 1 year in immunocompromised patients (4).
In our patient, the initial treatment (based on the Gram staining findings) consisted of broad-spectrum antibiotics (ceftriaxone and metronidazole), and antituberculous and antifungal (fluconazole) medications. These were switched to trimethoprim/sulfamethoxazole once the final bacterial culture and sensitivity results were obtained.
However, the optimal management of a Nocardia infection of the brain remains unclear. Mamelak et al. analyzed 131 patients with this condition along with their own experience of 11 patients (4). They recommended an use of sulfa drugs, empirically when clinically stable extraneural nocardial infection or an immuno-competent patient with a brain abscess less than 2 cm in diameter. If the patient's condition deteriorates or if the abscess does not decrease in size within 4 weeks, then the lesion should be aspirated to confirm the diagnosis and decompress the lesion. All abscesses > 2.5 cm in size should be aspirated regardless of the immune status of the patient. If the abscess enlarges after 2 weeks of treatment or if it remains unchanged for 4 weeks despite antibiotic therapy, then a craniotomy should be performed to remove the abscess.
Nocardiosis involving the CNS can be fatal. Early diagnosis and the administration of suitable treatments as well as the performance of appropriate surgical procedures is essential. A Nocardia brain abscess should be considered during differential diagnosis of a cerebral tumor if a contrast-enhancing brain lesion is found in immunocompromised or even immunocompetent patients. This type of abscess is often misdiagnosed as a metastasis or glioblastoma.
Figures and Tables
 | Fig. 1Contrast-enhanced axial chest computed tomography (CT) scan showing a consolidative lesion with multiple nodules and inner necrosis in the left upper lobe (LUL) of the right lung. Fluid collection was observed in the pleural space along with left lower lobe (LLL) collapse, suggesting obstructive pneumonitis. |
 | Fig. 2An initial non-contrast-enhanced CT scan of the brain showing low attenuation of the right frontal white matter. |
 | Fig. 3Axial T2WI and sagittal T1WI MR image of the brain showing a small, ill-defined T1-low and T2-high signal intensity lesion in the right frontal white matter; a ring-enhancing lesion of approximately 8 mm was observed within the lesion following contrast infusion. |
 | Fig. 4On follow up examination after two weeks, a T2WI and contrastenhanced axial MR image of the brain showing the enlarged peripheral enhancing mass with perilesional edema in the right frontal lobe and a newly developed lesion in the right parietal lobe. |
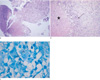 | Fig. 5
a. Percutaneous transthoracic needle biopsy of the lung revealed a necrotizing granulomatous inflammation (Hematoxylin & Eosin stain, ×100).
b. Brain specimen showing the abscess cavity (asterisk) with a surrounding rim of fibrosis (white arrow), chronic inflammatory cells, and histiocytes (black arrow) (Hematoxylin & Eosin stain, ×100).
c. GMS staining of the brain abscess revealed long, branching, Gram-positive filamentous bacilli (white arrow) (×1000).
|
References
1. Beaman BL, Beaman L. Nocardia species: host-parasite relationships. Clin Microbiol Rev. 1994; 7:213–264.
2. Lee GY, Daniel RT, Brophy BP, Reilly PL. Surgical treatment of nocardial brain abscesses. Neurosurgery. 2002; 51:668–671.
3. Beaman BL, Burnside J, Edwards B, Causey W. Nocardial infections in the United States, 1972-1974. J Infect Dis. 1976; 134:286–289.
4. Mamelak AN, Obana WG, Flaherty JF, Rosenblum ML. Nocardial brain abscess: treatment strategies and factors influencing outcome. Neurosurgery. 1994; 35:622–631.
5. Fleetwood IG, Embil JM, Ross IB. Nocardia asteroides cerebral abscess in immunocompetent hosts: report of three cases and review of surgical recommendations. Surg Neurol. 2000; 53:605–610.
6. Mogilner A, Jallo GI, Zagzag D, Kelly PJ. Nocardia abscess of the choroid plexus: clinical and pathological case report. Neurosurgery. 1998; 43:949–952.
7. Roquer J, Pou A, Herraiz J, et al. Primary cerebral abscess due to nocardia presenting as 'ghost tumor'. Clinical and pathological study. Eur Neurol. 1990; 30:254–257.
8. Lim JH, Chung TS, Kim HK, Ahn JY, Suh SH. Isolated aspergillosis of the brain in an immunocompetent patient: a case report. J Korean Soc Magn Reson Med. 2010; 14:64–68.
9. Baikie AG, Macdonald CB, Mundy GR. Systemic nocardiosis treated with trimethoprim and sulphamethoxazole. Lancet. 1970; 2:261.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download