Abstract
Purpose
To evaluate late gadolinium enhancement (LGE) pattern of left ventricular (LV) myocardium and presence or absence of LGE in other regions of the heart on cardiac magnetic resonance (CMR) imaging in patients diagnosed with cardiac amyloidosis.
Materials and Methods
From 2009 to 2011, 9 patients who were suspected cardiac amyloidosis underwent CMR. We retrospectively analyzed the presence or absence of LGE and enhancement pattern in LV myocardium, and the presence or absence of LGE in other chambers as well. Also we measured interatrial septal thickness (IST), relative signal intensities of atrial septum and epicardial fat over the left atrial (LA) cavity on delayed enhanced images. MRI parameters in these patients were compared to those of control group of patients with ischemic heart disease by Wilcoxon rank sum test.
Results
Of nine patients, LGE were found in 8; subendocardial circumferential pattern in 4 and diffuse pattern in 4. LGE in right ventricle was observed in 7. IST was significantly increased in patients with cardiac amyloidosis (P = 0.02). Ratio of atrial septum to LA cavity and ratio of epicardial fat to LA cavity showed a significant difference (P = 0.0002 and P = 0.0006, respectively).
Figures and Tables
Fig. 1
Phase-sensitive inversion recovery sequence images showing subendocardial circumferential enhancement pattern in 79-year-old female with cardiac amyloidosis.
Four-chamber (a) and short-axis views (b) show global subendocardial circumferential enhancement of left ventricular wall (arrowheads) in a nonvascular distribution. Diffuse enhancement of interartrial septum and both atria was noted (arrows). Of note, diffuse epicardial strong enhancement was associated (white arrows). Ratio of atrial septum to left atrial cavity signal was 1.02 and ratio of epicardial fat signal to left atrial cavity signal was 1.06.
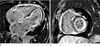
Fig. 2
Phase-sensitive inversion recovery sequence images showing diffuse transmural enhancement pattern in 51-year-old male with cardiac amyloidosis.
Four-chamber view (a) shows diffuse transmural enhancement of left ventricular wall in a nonvascular distribution. Interatrial septum (arrow) and right atrial wall (arrowheads) were thickened with enhancement. Short-axis view (b) shows diffuse enhancement and dark blood pool commonly seen in cardiac amyloidosis. Ratio of atrial septum to left atrial cavity signal and ratio of epicardial fat signal to left atrial cavity signal was 1.18 and 1.26, respectively.

Fig. 3
Phase-sensitive inversion recovery sequence images showing subendocardial infarction in 57-year-old male with ischemic heart disease.
Four-chamber (a) and short axis views (b) show subendocardial delayed enhancement in apical anterior, septal and inferior wall of left myocardium, indicating subendocardial infarction in the territory of right coronary and left anterior descending arteries (arrowheads). Blood signal was increased and interatrial septum (arrows) was relatively dark. Ratio of atrial septum to left atrial cavity signal and ratio of epicardial fat signal to left atrial cavity signal was 0.91 and 0.92, respectively.

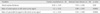
Table 1
Clinical and Histologic Characteristics of Patients with Cardiac Amyloidosis Showing Delayed Enhancement on CMR

*Not measured
†Cut-off value of BNP : 100 pg/ml
§Abdominal fat was sampled to histopathologic study
CMR, cardiac magnetic resonance; DE, delayed enhancement; BSA, body surface area; BNP, brain natriuretic peptide; AL, amyloid light chain; TTR, transthyretin; ECG, electrocardiogram; EM, endomyocardium; BM, bone marrow
References
1. Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. 2003; 349:583–596.
2. Smith TJ, Kyle RA, Lie JT. Clinical significance of histopathologic patterns of cardiac amyloidosis. Mayo Clin Proc. 1984; 59:547–555.
3. Falk RH, Dubry SW. Amyloid heart disease. Prog Cardiovasc Dis. 2010; 52:347–361.
4. Falk RH. Diagnosis and management of the cardiac amyloidosis. Circulation. 2005; 112:2047–2060.
5. Pellikka PA, Holmes DR Jr, Edwards WD, et al. Endomyocardial biopsy in 30 patients with primary amyloidosis and suspected cardiac involvement. Arch Intern Med. 1988; 148:662–666.
6. Yilmaz A, Kindermann I, Kindermann M, et al. Comparative evaluation of left and right ventricular endomyocardial biopsy: differences in complication rate and diagnostic performance. Circulation. 2010; 122:900–909.
7. Perugini E, Rapezzi C, Piva T, et al. Non-invasive evaluation of the myocardial substrate of cardiac amyloidosis by gadolinium cardiac magnetic resonance. Heart. 2006; 92:343–349.
8. Syed IS, Glockner JF, DaLi F, et al. Role of cardiac magnetic resonance imaging in the detection of cardiac amyloidosis. JACC Cardiovasc Imaging. 2010; 3:155–164.
9. Vogelsberg H, Mahrholdt H, Deluigi CC, et al. Cardiovascular magnetic resonance in clinically suspected cardiac amyloidosis: noninvasive imaging compared to endomyocardial biopsy. J Am Coll Cardiol. 2008; 51:1022–1030.
10. Austin BA, Wilson Tang WH, Rodriguez R, et al. Delayed hyper-enhancement magnetic resonance imaging provides incremental diagnostic and prognostic utility in suspected cardiac amyloidosis. JACC Cardiovasc Imaging. 2009; 2:1369–1377.
11. Bellavia D, Pellikka PA, Abraham TP, et al. Evidence of impaired left ventricular systolic function by Doppler myocardial imaging in patients with systemic amyloidosis and no evidence of cardiac involvement by standard two-dimensional and Doppler echocardiography. Am J Cardiol. 2008; 101:1039–1045.
12. Cummings KW, Bhalla S, Javidan-Nejad C, Bierhals AJ, Gutierrez FR, Woodard PK. A pattern-based approach to assessment of delayed enhancement in nonischemic cardiomyopathy at MR Imaging. Radiographics. 2009; 29:89–103.
13. Cerqueira MD, Weissman NJ, Diilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the cardiac imaging committee of the council on clinical cardiology of the American heart association. Circulation. 2002; 105:539–542.
14. Maceira AM, Joshi J, Prasad SK, et al. Cardiovascular magnetic resonance in cardiac amyloidosis. Circulation. 2005; 111:186–193.
15. Ruberg FL, Appelhaum E, Davidoff R, et al. Diagnostic and prognostic utility of cardiovascular magnetic resonance imaging in light-chain cardiac amyloidosis. Am J Cardiol. 2009; 103:544–549.
16. Mekinian A, Lions C, Leleu X, et al. Prognosis assessment of cardiac involvement in systemic AL amyloidosis by magnetic resonance imaging. Am J Med. 2010; 123:864–868.
17. Siqueira-Filho AG, Cunha CL, Tajik AJ, Seward JB, Schattenberg TT, Giuliani ER. M-mode and two-dimensional echocardiographic features in cardiac amyloidosis. Circulation. 1981; 63:188–196.
18. Di Bella G, Minutoli F, Mazzeo A, et al. MRI of cardiac involvement in transthyretin familial amyloid polyneuropathy. AJR Am J Roentgenol. 2010; 195:W394–W399.
19. Berk JL, Keane J, Seldin DC. Persistent pleural effusions in primary systemic amyloidosis - etiology and prognosis. Chest. 2003; 124:969–977.
20. Falk RH, Plehn JF, Deering T, et al. Sensitivity and specificity of the echocardiographic features of cardiac amyloidosis. Am J Cardiol. 1987; 59:418–422.
21. Fattori R, Rocchi G, Celletti F, Bertaccini P, Rapezzi C, Gavelli G. Contribution of magnetic resonance imaging in the differential diagnosis of cardiac amyloidosis and symmetric hypertrophic cardiomyopathy. Am Heart J. 1998; 136:824–830.
22. Westermark P, Stenkvist B. A new method for the diagnosis of systemic amyloidosis. Arch Intern Med. 1973; 132:522–523.
23. Migrino RQ, Christenson R, Szabo A, Bright M, Truran S, Hari P. Prognostic implication of late gadolinium enhancement on cardiac MRI in light chain (AL) amyloidosis on long term follow up. BMC Med Phys. 2009; 9:5.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download