Abstract
Purpose
This study was performed to evaluate the presence and severity of Hill-Sachs (HS) lesions on MR arthrography (MRA) of shoulder in patients with Bankart lesions following anterior dislocation and to investigate their relationship with Bankart lesions and frequency of dislocations.
Materials and Methods
86 MRA of shoulder were evaluated in patients with arthroscopic Bankart repairs following anterior dislocations. The largest surface length of HS lesion on MRA and extent of Bankart lesions on arthroscopy were measured. Relationships between length of HS lesions and extent of Bankart lesions and frequency of dislocations were assessed.
Results
HS lesions were identified on MRA in 78 patients. The largest surface length of HS lesion ranged from 9.3 mm to 29.6 mm (mean, 18.8 mm). The extent of Bankart lesion ranged from one to six o'clock extent (mean, 4.25 o'clock extent). Three patients had single dislocation and the other 75 patients had recurrent dislocations (mean 24.5 times). The largest surface length of HS lesions was positively correlated with extent of Bankart lesions (p = 0.001, r = 0.37), but not with frequency of dislocation.
The shoulder is the most mobile joint in the body. This flexibility allows the shoulder to have a wide range of motion at various positions, but also gives a particularly high chance of instability, thus making the glenohumeral joint the most common site of dislocation in the human body. The majority of shoulder dislocation occurs anteriorly. During dislocation, the humeral head is displaced anteroinferiorly and the capsuloligamentous components are stretched out, resulting in injuries to such structures.
Hill-Sachs lesion is a compression fracture on the posterolateral aspect of the humeral head, that is a typical bony abnormality after anterior dislocation. An injury on the other side of the joint, when the glenoid labrum in the anteroinferior aspect becomes detached with a tear of the inferior glenohumeral ligament, is called a classic Bankart lesion. Occasionally erosion or a defect of the anterior aspect of the glenoid bone can be present (1-4).
Hill-Sachs and Bankart lesions are commonly found when evaluating the shoulder instability (5-7). Both are produced during the anterior dislocation of the shoulder, and their relation has been reported to have a positive trend (8). However, all of the etiologies of both lesions have not been clearly established and neither is likely to be the exact counterpart of the other (9). Regarding the relationship of Hill-Sachs lesion with the frequency of the shoulder dislocation, although there have been quite a few clinical investigations, controversies still remain as some studies have proposed their contribution to the shoulder dislocation based on the higher incidence of Hill-Sachs lesions in patients with recurrent dislocations (5, 10-12), while other studies reported that there was no relationship between these lesions and the frequency of dislocation (3, 7, 8).
The purposes of this study were to evaluate the prevalence and the severity of Hill-Sachs lesion seen on MR arthrography in patients with Bankart lesion following anterior shoulder dislocations, and to investigate the relationship of Hill-Sachs lesions with Bankart lesions as well as with the frequency of shoulder dislocations.
We retrospectively analyzed eighty-six MR arthrograms of the shoulder in patients who received arthroscopic Bankart repair after antecedent anterior shoulder dislocation from 2007 to 2009. All of these patients underwent direct MR arthrography of the shoulder in order to assess instability following shoulder dislocations and then received arthroscopic Bankart repair after MR imaging was performed. The patients who had bony Bankart lesion were excluded. Seventy-three males and thirteen females ranging age from 13 to 73 years (mean age, 26.4 years) were enrolled.
Our institutional ethics committee approved this retrospective study. Informed consent was obtained from all patients after the nature of the procedure had been fully explained to them prior arthrography. Under fluoroscopic guidance, each patient was prepared in supine position for injection. After administration of lidocaine into the skin overlying the glenohumeral joint, a 22-gauge spinal needle was advanced into the joint space. Intra-articular positioning of the needle was confirmed with a test injection of less than 1 ml of iodinated contrast material (iohexol, Omnipaque; GE Healthcare, Carrington hill, Ireland). Approximately 15 - 20 ml of diluted gadopentate dimeglumine (Magnevist; Schering, Berlin, Germany) was then injected in a concentration of 1 mmol/l. To obtain this concentration, 1 ml of gadopentate dimeglumine was added to 250 ml of normal saline solution.
MR images were obtained with 1.5 T imagers (Signa; GE Medical Systems, Milwaukee, WI, USA, or Intera-NT; Philips Medical Systems, Best, The Netherlands) using a dedicated shoulder coil. Each patient was positioned with their arms at the sides of their body in a neutral position. Spin-echo T1-weighted (repetition time in ms/echo time in ms = 650/16, 760/60) MR images with fat saturation were acquired in axial, oblique coronal, and oblique sagittal planes, and fast spin-echo T2-weighted images (repetition time in ms/echo time in ms = 3300/96, 3500/90) were acquired in axial and oblique coronal planes. The imaging parameters were common to both scanners; 256×192 matrix, 2 NEX, slice thickness of 4-mm with 1-mm interslice gap, and 14×14-cm field of view. Only fat-saturated T1-weighted series were evaluated in our study.
Initially, two experienced musculoskeletal radiologists who were unaware of the patients' clinical details, reviewed fifteen MR arthrograms of the shoulder which were not included in this study, as this session was to establish a baseline consensus in the findings and severity of Hill-Sachs lesion on MR images. One radiologist then reviewed MR arthrograms included in this study.
Hill-Sachs lesion was considered to be present on MR images when an abnormal contour, i.e. notched defect or flattening, of the posterolateral aspect of the superior portion of the humeral head was observed in the axial plane and on either the oblique coronal or the oblique sagittal planes (Fig. 1). When Hill-Sachs lesion was present, its extent was further evaluated on axial images. A circular frame of reference regarding the humeral head was established on contiguous axial images showing Hill-Sachs lesion. The surface length of Hill-Sachs lesion was measured on axial images and the largest such surface length among these measurements was recorded (Fig. 2) (11).
Surgical reports of arthroscopy were reviewed in order to determine the extent of Bankart lesion. Bankart lesion was defined as detachment of the labrum and joint capsule from the anterior glenoid rim as seen at arthroscopy. The lesion extent was described on the basis of conventional clock-face description of the location of the glenoid labrum (Fig. 3). The median interval between MR imaging and surgery was 40 days (range, one to 108 days). The patients' medical records were reviewed in order to determine the number of frequency of shoulder dislocations.
The relationship between the severity of Hill-Sachs lesion seen on MR arthrography and the extent of Bankart lesion seen at arthroscopy, was evaluated using Spearman's rank test. Spearman's correlation was also used to test the relationship between the severity of Hill-Sachs lesion and the frequency of shoulder dislocations.
Spearman's correlation coefficient (r) of 1.0 indicates a perfectly positive linear correlation, and a P value less than 0.05 was considered to indicate a significant difference. The statistical Package for Social Sciences program (version 17.0, SPSS, Chicago, IL, USA) for Windows was used for the statistical data analyses.
Hill-Sachs lesions were identified in 78 patients of 86 (90.7%) patients on MR arthrograms of the shoulder, who were received arthroscopic Bankart repair following anterior shoulder dislocation. They were 67 males and 11 females, and the average age was 26.8 years (range, 15 to 73 years). The remaining eight (9.3%) patients had no evidence of a contour deformity of the humeral head indicating the presence of Hill-Sachs lesion on MR arthrography of the affected shoulder. Regarding the severity of Hill-Sachs lesion, the largest surface length of Hill-Sachs lesion measured on contiguous axial MR images ranged from 9.3 mm to 29.6 mm, and the mean±SD was 18.8±4.4 mm.
The extent of Bankart lesion according to the arthroscopic reports in 78 patients showing Hill-Sachs lesions on MR arthrograms, ranged from one to six o'clock extent according to the conventional, clock-face description, and its mean±SD was 4.25±0.9 o'clock extent.
Only three patients had a history of a single, anterior shoulder dislocation. The other 75 patients had recurrent anterior shoulder dislocations with a frequency range of two to 100 times. The mean frequency of anterior shoulder dislocations was 24.5 times and the SD was ±26 times.
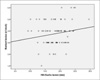
The relationship between the largest surface length of Hill-Sachs lesions on MR arthrography and the extent of Bankart lesion at arthroscopy was statistically significant and showed a positive correlation (p = 0.001, r = 0.37) (Fig. 4).
The largest surface length of Hill-Sachs lesions was not statistically correlated with the frequency of shoulder dislocations (p = 0.4).
The stability of the glenohumeral joints is critical for establishing the essential function of the shoulders as a fulcrum for placing the upper extremities at various positions in three-dimensional space. This is provided by various bony and soft tissue structures which are divided into static and dynamic components. Static stabilizers include the bony components, cartilaginous labrum, glenohumeral ligament, particularly the inferior one, and the joint capsule. Rotator cuff muscles and the long head of the biceps tendon are considered as dynamic stabilizers with its compression concavity mechanism (4, 13).
The bony component comprising the humeral head and the glenoid is not only the basis of stability of glenohumeral joint but is also a major contributor to the inherent instability of this joint because of the discrepancy in size between the large humeral head and the small glenoid cavity (4, 13, 14). As such, injury to this foundation may cause more severe shoulder instability promoting a vicious circle (14, 15).
Hill-Sachs lesion is thought to result from impaction of a dislocated humerus against the glenoid and is seen as a notched defect or flattening of the contour of the posterolateral aspect of the humeral head (2, 5). This deformity has been evaluated using various diagnostic methods, including plain radiography of anteroposterior projection and specialized views such as internal rotation or the Stryker Notch view, as well as ultrasonography, computed tomography (CT), MR imaging, and CT or MR arthrography. MR imaging is the first imaging modality in assessing shoulder joint abnormalities with instability. MR arthrography, particularly, can be very helpful to detect subtle lesion (4, 7, 16, 17). It is considered to be the method of a choice for assessment of the labrum and glenohumeral ligaments (13, 17), although CT is excellent for detecting bony lesions and a recent study showed that CT arthrography may be a good alternative to MRI especially for evaluating labral lesions (18).
The incidence of Hill-Sachs lesion in patients with anterior shoulder dislocation has been reported to range from 31% to 93% (10, 11, 19-21). Such a wide range could considerably be attributed to the different imaging modalities used and the development of imaging equipments over time. The recent studies using CT and MR arthrography revealed that the prevalence of Hill-Sachs lesion in patients with anterior dislocation was 86% and 71%, respectively (7, 9). On MR arthrography in our series, Hill-Sachs lesion was identified in 90.7% of the patients following anterior dislocation, who had Bankart lesions confirmed on arthroscopy. This supports that Hill-Sachs lesion is closely correlated with Bankart lesion following anterior shoulder dislocation as reported previously (8).
A large Hill-Sachs lesion may lead to recurrent shoulder dislocation as it acts as a lever that promotes translation of the humeral head in external rotated arm (5, 11). To define a critical level for surgical treatment, there have been many attempts to classify the severity of Hill-Sachs lesions. Rockwood et al. classified Hill-Sachs lesions into three degrees, comprising mild defect of less than 20% deformity, moderate degree of between 20% to 45%, and severe defect of greater than 45%, according to the percentage of humeral head involved (22). Spatschil et al. divided the size of Hill-Sachs lesion on arthroscopy; non, chondral, osteochondral flat, or osteochondral deep (10). Griffith et al. estimated the overall size of Hill-Sachs deformity on serial axial CT images and classified them as absent, minimal, mild, moderate, or severe degrees (9). Cetik et al. measured the percentage and depth of Hill-Sachs lesion on CT arthrography (11). Cicak et al. calculated the volume of Hill-Sachs lesion on ultrasound using their width, length, and depth (23). For determining the severity of Hill-Sachs lesion seen on MR arthrography, we measured the largest surface length of a contour deformity of the humeral head on contiguous MR axial images. This measurement could be readily applicable and reproducible in routine clinical practice, although three-dimensional quantification of a bony defect would be helpful to more accurately evaluate the extent of Hill-Sachs lesions. In this study, the largest surface length of Hill-Sachs lesion seen on MR arthrography was in range of 9.3 to 29.6 mm, with the mean being 18.8 mm.
Widjaja et al. suggested that there is a strong correlation between Hill-Sachs lesions and Bankart lesions on MRI, however, they only evaluated the incidence of both lesions, and not the severity of these lesions (8). In addition, their result was also not statistically significant because of the small number of the study patients. The study by Griffith et al. revealed that glenoid bone loss in patients with anterior dislocation on CT was positively correlated with the severity of Hill-Sachs deformity, although they did not evaluate the glenoid labral lesion (9). In order to determine the relationship of the severity between both lesions in our study, the measurement of the largest surface length of each Hill-Sachs lesion was compared with the extent of each Bankart lesion confirmed on arthroscopy. The extent of Hill-Sachs lesion was positively correlated with the extent of each Bankart lesion (r = 0.37), thus indicating that Hill-Sachs lesions tend to be larger in patients having more severe Bankart lesion.
Several studies have been shown that the incidence of Hill-Sachs lesion in patients with recurrent shoulder dislocation was higher than in those with a single dislocation (5, 10-12). However, the relationship between the extent of Hill-Sachs lesion and frequency of shoulder dislocation were assessed in only a few studies. In the study by Griffith et al., the deformity of humeral head was more severe in patients with recurrent dislocations (12). Cetik et al. reported that the extent of Hill-Sachs lesion was positively correlated with the frequency of anterior shoulder dislocation (11). However, our results showed no significant correlation between the length of Hill-Sachs lesion and the frequency of the shoulder dislocations. We suggested that it is not possible to accurately predict the severity of Hill-Sachs lesion solely on the basis of the frequency of dislocations.
There are some limitations to our study. First, the presence and extent of Hill-Sachs lesions we evaluated on MR arthrography were not precisely correlated with the surgical findings, although all of our study patients had undergone the arthroscopic surgery. However, MR arthrography has been proposed as more accurate than arthroscopy for evaluating Hill-Sachs lesions (5, 23). In addition, the largest surface length of lesions was evaluated, without using its volume. Second, as the median time lag between MR arthrography and arthroscopy in surgery was 40 days, with a wide range from one day to 108 days, this may have influenced the severity of Bankart lesions. This study is retrospective in nature and with the frequency of dislocation also established retrospectively. Therefore, resulting frequency of dislocations cited by patients with frequent dislocations may not be entirely accurate. Also, regarding the relation to the frequency of shoulder dislocation, the difference of the extent of Hill-Sachs lesion or of Bankart lesion between single dislocation and recurrent dislocations could not be evaluated because of small number of patients.
Hill-Sachs lesions were very common in patients with Bankart lesion confirmed on arthroscopy, in as many as 90.6% of these patients, following anterior shoulder dislocation. Regarding the severity of Hill-Sachs lesion when identified on MR arthrography, the largest surface length of Hill-Sachs lesions was positively correlated with the extent of Bankart lesions observed on arthroscopy. This supports the close relationship between Hill-Sachs and Bankart lesions regarding both their incidence and severity and, therefore, suggests that if one of these lesions is detected, there is a high probability that the other will also be identified and that the larger Hill-Sachs lesion, the more severe Bankart lesion will be seen when evaluating MR images of the shoulder in patients with a history of anterior shoulder dislocation.
Figures and Tables
Fig. 1
Hill-Sachs lesion on MR arthrogram in a patient with antecedent anterior shoulder dislocation.
A fat-saturated T1-weighted axial MR image at the level of the coracoid process shows a notched defect (arrow) (a) and flattening (arrow) (b) on posterolateral aspect of humeral head indicating Hill-Sachs lesion.
Fig. 2
Measurement of the largest surface length of Hill-Sachs lesion on MR arthrogram.
On three contiguous fat-saturated T1-weighted axial MR images, the surface lengths of bony defect on posterolateral aspect of humeral head (dotted lines) are measured (a-c). Among them, the largest surface length of Hill-Sachs lesion (b) is recorded as the extent of Hill-Sachs lesion.

Fig. 3
Description of conventional clock-face in glenoid.
A fat-saturated T1-weighted oblique coronal image shows a detachment of anteroinferior aspect of glenoid labrum (dotted line with arrow tips), indicating Bankart lesion. Bankart lesion is located at 2 to 6 o'clock direction on the basis of conventional clock-face description of the location of the glenoid labrum, the extent of Bankart lesion is 4 o'clock extent. Arrows indicates 12, 3, 6, 9 o'clock direction starting from the superior point with counterclockwise direction.

Fig. 4
Scatterplot graph about relationship between the largest surface length of Hill-Sachs lesions and the extent of Bankart lesions.
Graph shows a positive correlation between the largest surface length of Hill-Sachs lesions on MR arthrograms (x-axis) and the extent of Bankart lesions at arthroscopy (y-axis). The Spearman's correlation coefficient is 0.37, p = 0.001.
References
1. Bankart A. The pathology and treatment of recurrent anterior dislocation of the shoulder joint. Br J Surg. 1938; 26:23–29.
2. Hill H, Sachs M. The grooved defect of the humeral head. A frequently unrecognized complication of dislocations of the sholuder. Radiology. 1940; 35:690–700.
3. Calandra JJ, Baker CL, Uribe J. The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. Arthroscopy. 1989; 5:254–257.
4. Beltran J, Rosenberg ZS, Chandnani VP, Cuomo F, Beltran S, Rokito A. Glenohumeral instability: evaluation with MR arthrography. Radiographics. 1997; 17:657–673.
5. Workman TL, Burkhard TK, Resnick D, et al. Hill-Sachs lesion: comparison of detection with MR imaging, radiography, and arthroscopy. Radiology. 1992; 185:847–852.
6. Griffith JF, Antonio GE, Tong CW, Ming CK. Anterior shoulder dislocation: quantification of glenoid bone loss with CT. AJR Am J Roentgenol. 2003; 180:1423–1430.
7. Antonio GE, Griffith JF, Yu AB, Yung PS, Chan KM, Ahuja AT. First-time shoulder dislocation: high prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging. 2007; 26:983–991.
8. Widjaja AB, Tran A, Bailey M, Proper S. Correlation between Bankart and Hill-Sachs lesions in anterior shoulder dislocation. ANZ J Surg. 2006; 76:436–438.
9. Griffith JF, Antonio GE, Yung PS, et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol. 2008; 190:1247–1254.
10. Spatschil A, Landsiedl F, Anderl W, et al. Posttraumatic anterior-inferior instability of the shoulder: arthroscopic findings and clinical correlations. Arch Orthop Trauma Surg. 2006; 126:217–222.
11. Cetik O, Uslu M, Ozsar BK. The relationship between Hill-Sachs lesion and recurrent anterior shoulder dislocation. Acta Orthop Belg. 2007; 73:175–178.
12. Griffith JF, Yung PS, Antonio GE, Tsang PH, Ahuja AT, Chan KM. CT compared with arthroscopy in quantifying glenoid bone loss. AJR Am J Roentgenol. 2007; 189:1490–1493.
13. Cicak N, Bilić R, Delimar D. Hill-Sachs lesion in recurrent shoulder dislocation: sonographic detection. J Ultrasound Med. 1998; 17:557–560.
14. Omoumi P, Teixeira P, Lecouvet F, Chung CB. Glenohumeral joint instability. J Magn Reson Imaging. 2011; 33:2–16.
15. Bushnell BD, Creighton RA, Herring MM. Bony instability of the shoulder. Arthroscopy. 2008; 24:1061–1073.
16. Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res. 2002; 400:32–39.
17. Sanders TG, Morrison WB, Miller MD. Imaging techniques for the evaluation of glenohumeral instability. Am J Sports Med. 2000; 28:414–434.
18. Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology. 2005; 237:578–583.
19. Oh JH, Kim JY, Choi JA, Kim WS. Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: comparison with magnetic resonance imaging with arthroscopic correlation. J Shoulder Elbow Surg. 2010; 19:14–20.
20. Singson RD, Feldman F, Bigliani L. CT arthrographic patterns in recurrent glenohumeral instability. AJR Am J Roentgenol. 1987; 149:749–753.
21. Cook JV, Tayar R. Double-contrast computed tomographic arthrography of the shoulder joint. Br J Radiol. 1989; 62:1043–1049.
22. Ito H, Takayama A, Shirai Y. Radiographic evaluation of the Hill-Sachs lesion in patients with recurrent anterior shoulder instability. J Shoulder Elbow Surg. 2000; 9:495–497.
23. Bigliani L, Flatow E, Pollock R. Rockwood and Green's fractures in adults. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2005.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download