Abstract
Purpose
The origin of the vertebral artery (VA) is a frequent site of pseudostenosis on contrast-enhanced MRA (CE-MRA). The purpose of this study is to evaluate the relationship between the motion of the aortic arch and pseudostenosis at the origin of the VA.
Materials and Methods
Our study had approval of our institutional review board. 47 patients underwent CT angiography (CTA), CE-MRA, and 3D time-resolved contrast-enhanced MRA (TR-CEMRA) within 6.87±9.89 days (mean±SD). Percent stenosis using the NASCET criteria was measured on CTA and CE-MRA. CTA was used as a reference standard to classify the CE-MRA into pseudostenosis and control group. Pseudostenosis was determined as 50%-99% stenosis observed on CE-MRA but normal to less than 50% stenosis on CTA. Aortic motion (distance between the highest position and lowest position of aortic arch) was measured on TR-CEMRA. Age, route of intravenous contrast media, motion of aortic arch, and normal distal diameter of VA were compared between the two groups.
Results
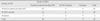
There were 17 patients and 23 vertebral arteries of pseudostenosis. Patients with pseudostenosis showed more aortic motion (3.61±1.88 vs. 2.05±1.97 mm) and older age (71.29±8.88 vs. 62.32±13.19 year-old). Route of intravenous contrast media and normal distal diameter of VA were not associated with pseudostenosis.
Figures and Tables
Fig. 1
a-f. serial images of dynamic 3D time-resolved contrast-enhanced MRA.
c. Lowest position of upper border of aortic arch are marked by red horizontal line.
d. Highest position of upper border of aortic arch. Distance between these two horizontal lines was considered as motion of aortic arch

Fig. 2
a. CTA shows no stenosis of the origin of the left vertebral artery.
b. MRA of same patient after 5 days shows pseudostenosis of the origin of the left vertebral artery (arrow).

References
1. Khan S, Rich P, Clifton A, Markus HS. Noninvasive detection of vertebral artery stenosis: a comparison of contrast-enhanced MR angiography, CT angiography, and ultrasound. Stroke. 2009. 40:3499–3503.
2. Anzidei M, Napoli A, Marincola BC, et al. Gadofosveset-enhanced mr angiography of carotid arteries: does steady-state imaging improve accuracy of firstpass imaging? comparison with selective digital subtraction angiography. Radiology. 2009. 251:457–446.
3. Wardlaw JM, Chappell FM, Best JJ, Wartolowska K, Berry E. Non-invasive imaging compared with intra-arterial angiography in the diagnosis of symptomatic carotid stenosis: a meta-analysis. Lancet. 2006. 367:1503–1512.
4. Yang CW, Carr JC, Futterer SF, et al. Contrast-enhanced MR angiography of the carotid and vertebrobasilar circulations. AJNR Am J Neuroradiol. 2005. 26:2095–2101.
5. Remonda L, Senn P, Barth A, Arnold M, Lovblad KO, Schroth G. Contrastenhanced 3d MR angiography of the carotid artery: comparison with conventional digital subtraction angiography. AJNR Am J Neuroradiol. 2002. 23:213–219.
6. Kim SH, Lee JS, Kwon OK, Han MK, Kim JH. Prevalence study of proximal vertebral artery stenosis using high-resolution contrast-enhanced magnetic resonance angiography. Acta Radiologica. 2005. 46:314–321.
7. Marquardt L, Kuker W, Chandratheva A, Geraghty O, Rothwell PM. Incidence and prognosis of > or = 50% symptomatic vertebral or basilar artery stenosis: prospective population-based study. Brain : a journal of neurology. 2009. 132:982–998.
8. Compter A, van der Worp HB, Algra A, Kappelle LJ. Prevalence and prognosis of asymptomatic vertebral artery origin stenosis in patients with clinically manifest arterial disease. Stroke. 2011. 42:2795–2800.
9. Khan S, Cloud GC, Kerry S, Markus HS. Imaging of vertebral artery stenosis: a systematic review. J Neurol Neurosurg Psychiatry. 2007. 78:1218–1225.
10. Choi HS, Kim DI, Kim DJ, Kim J, Kim ES, Lee SK. Accuracy of 3 t MR angioraphy in vertebral artery stenosis and coincidence with other cerebrovascular stenoses. Neuroradiology. 2010. 52:893–898.
11. Leclerc X, Martinat P, Godefroy O, et al. Contrast-enhanced three-dimensional fast imaging with steady-state precession (fisp) MR angiography of supraaortic vessels: preliminary results. AJNR Am J Neuroradiol. 1998. 19:1405–1413.
12. Randoux B, Marro B, Koskas F, Chiras J, Dormont D, Marsault C. Proximal great vessels of aortic arch: comparison of three-dimensional gadolinium-enhanced MR angiography and digital subtraction angiography. Radiology. 2003. 229:697–702.
13. Cosottini M, Calabrese R, Puglioli M, et al. Contrast-enhanced three-dimensional MR angiography of neck vessels: does dephasing effect alter diagnostic accuracy? Eur Radiol. 2003. 13:571–581.
14. Tomasian A, Salamon N, Lohan DG, Jalili M, Villablanca JP, Finn JP. Supraaortic arteries: contrast material dose reduction at 3.0-t high-spatial-resolution MR angiography--feasibility study. Radiology. 2008. 249:980–990.
15. Lohan DG, Tomasian A, Saleh RS, Singhal A, Krishnam MS, Finn JP. Ultra-low-dose, time-resolved contrast-enhanced magnetic resonance angiography of the carotid arteries at 3.0 tesla. Invest Radiol. 2009. 44:207–217.
16. Lee YJ, Laub G, Jung SL, et al. Low-dose 3d time-resolved magnetic resonance angiography (MRA) of the supraaortic arteries: correlation with high spatial resolution 3d contrast-enhanced MRA. J Magn Reson Imaging. 2011. 33:71–76.
17. Randoux B, Marro B, Koskas F, et al. Carotid artery stenosis: prospective comparison of CT, three-dimensional gadolinium-enhanced MR, and conventional angiography. Radiology. 2001. 220:179–185.
18. Vertinsky AT, Schwartz NE, Fischbein NJ, Rosenberg J, Albers GW, Zaharchuk G. Comparison of multidetector CT angiography and MR imaging of cervical artery dissection. AJNR Am J Neuroradiol. 2008. 29:1753–1760.
19. Forsting M. Cta of the ica bifurcation and intracranial vessels. Eur Radiol. 2005. 15:Suppl 4. D25–D27.
20. North american symptomatic carotid endarterectomy trial collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with highgrade carotid stenosis. N Engl J Med. 1991. 325:445–453.
21. Roos JE, Willmann JK, Weishaupt D, Lachat M, Marincek B, Hilfiker PR. Thoracic aorta: motion artifact reduction with retrospective and prospective electrocardiography-assisted multi-detector row CT. Radiology. 2002. 222:271–277.
22. Morgan-Hughes GJ, Owens PE, Marshall AJ, Roobottom CA. Thoracic aorta at multi-detector row CT: motion artifact with various reconstruction windows. Radiology. 2003. 228:583–588.
23. Lin SC, Trocciola SM, Rhee J, et al. Analysis of anatomic factors and age in patients undergoing carotid angioplasty and stenting. Ann Vasc Surg. 2005. 19:798–804.
24. Carr JC, Ma J, Desphande V, Pereles S, Laub G, Finn JP. High-resolution breath-hold contrast-enhanced MR angiography of the entire carotid circulation. AJR Am J Roentgenol. 2002. 178:543–549.
25. Takei N, Miyoshi M, Kabasawa H. Noncontrast mr angiography for supraaortic arteries using inflow enhanced inversion recovery fast spin echo imaging. J Magn Reson Imaging. 2012. 35:957–962.
26. Lummel N, Boeckh-Behrens T, Lutz J, Burke M, Linn J. Evaluation of the supraaortic arteries using non-contrast-enhanced velocity MR angiography "inhance". Neuroradiology. 2012.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download