Abstract
We report a case of cardiac lymphoma in a 40-year-old man, who had a mediastinal mass which was diagnosed as sclerosing mediastinitis pathologically. The mediastinal mass caused right pulmonary arterial stenosis. The patient developed myocardial hypertrophy and echocardiography showed restrictive physiology and severely decreased left ventricle ejection fraction, 6 months later. MRI showed global left ventricular myocardial hypertrophy and diffuse late gadolinium hyperenhancement after administration of contrast material. Thus, non-ischemic cardiomyopathy was suspected on MRI. However, pathology confirmed the myocardial abnormality as lymphoma after myocardial biopsy. Because a basal part of the left ventricle and global subendocardial myocardium were not involved on contrast-enhanced delayed MRI, the MRI abnormalities could be differentiated from amyloidosis and other myocardial diseases. The peculiar non-mass forming diffuse hypertrophy pattern of cardiac lymphoma has not been known in the MRI literature.
Figures and Tables
Fig. 1
Transverse contrast-enhanced CT image shows a soft tissue mass (arrows) involving mid-mediastinum, encircling superior vena cava and right atrium.

Fig. 2
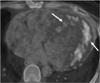
MR imaging findings.
a. 4-chamber-view cine MR image shows diffuse thickening of left ventricle myocardium, especially in apical septal segment, and small amount of pericardial effusion.
b. Short-axial plane T2-weighted image shows slightly increased signal intensity of left ventricle myocardium.
c. Gadolinium contrast-enhanced delayed myocardial images demonstrate thickened myocardium and diffuse late gadolinium enhancement (arrows) in mid-wall and epicardial layers except the basal portion of left ventricle.
d. Mitral valve flow analysis shows tall E wave with very high E/A ratio. Deceleration time measured 80.7 msec. "A" duration measured 93 msec.
e. Right pulmonary venous flow analysis shows a tall D wave and wide "AR" duration of 150 msec.

Fig. 4
Pathological findings.
a. Photomicrograph reveals small-to-medium sized atypical lymphoid cells having a high nucleus-to-cytoplasm ratio with minimal cytoplasm. The chromatins of the neoplastic cells are fine and nucleoli are either absent or inconspicuous (hematoxyline and eosine; magnification, ×400).
b. Tumor cells express the terminal deoxynucleotidyl transferase (TdT; magnification, ×400).
References
1. Rolla G, Bertero MT, Pastena G, et al. Primary lymphoma of the heart. A case report and review of the literature. Leuk Res. 2002. 26:117–120.
2. Fujisaki J, Tanaka T, Kato J, et al. Primary cardiac lymphoma presenting clinically as restrictive cardiomyopathy. Circ J. 2005. 69:249–252.
3. Lee PW, Woo KS, Chow LT, et al. Images in cardiovascular medicine. Diffuse infiltration of lymphoma of the myocardium mimicking clinical hypertrophic cardiomyopathy. Circulation. 2006. 113:e662–e664.
4. Grebenc ML, Rosado de Christenson ML, Burke AP, Green CE, Galvin JR. Primary cardiac and pericardial neoplasms: radiologic-pathologic correlation. Radiographics. 2000. 20:1073–1103. quiz 1110-1071, 1112.
5. Araoz PA, Eklund HE, Welch TJ, Breen JF. CT and MR imaging of primary cardiac malignancies. Radiographics. 1999. 19:1421–1434.
6. Karube K, Ohshima K, Tsuchiya T, et al. Non-B, non-T neoplasms with lymphoblast morphology: further clarification and classification. Am J Surg Pathol. 2003. 27:1366–1374.
7. Khuddus MA, Schmalfuss CM, Aranda JM, Pauly DF. Magnetic resonance imaging of primary cardiac lymphoma. Clin Cardiol. 2007. 30:144–145.
8. O'Donnell DH, Abbara S, Chaithiraphan V, et al. Cardiac tumors: optimal cardiac MR sequences and spectrum of imaging appearances. AJR Am J Roentgenol. 2009. 193:377–387.
9. Maron BJ, Towbin JA, Thiene G, et al. American Heart Association. Council on Clinical Cardiology, Heart Failure and Transplantation Committee. Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups. Council on Epidemiology and Prevention. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006. 113:1807–1816.
10. Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005. 26:1461–1474.
11. Flannery MT, Espino M, Altus P, Messina J, Wallach PM. Hodgkin's disease masquerading as sclerosing mediastinitis. South Med J. 1994. 87:921–923.
12. Miyata T, Takahama M, Yamamoto R, Nakajima R, Tada H. Sclerosing mediastinitis mimicking anterior mediastinal tumor. Ann Thorac Surg. 2009. 88:293–295.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download