Abstract
Central nervous system (CNS) involvement in acute promyelocytic leukemia (APL) is rare, and the presence of CNS symptoms at the time of diagnosis of APL is even rarer. We report 2 cases of APL presenting with CNS involvement. A 43-yr-old woman presented with easy bruising and stuporous mentality. Her complete blood count (CBC) revealed leukocytosis with increased blasts. Bone marrow (BM) analysis was carried out, and the diagnosis of APL was confirmed. This was done by cytogenetic analysis and demonstration of PML-RARα rearrangement by reverse transcriptase PCR in the BM cells. A lumbar puncture was performed to investigate the cause of her stuporous mentality, and her cerebrospinal fluid (CSF) analysis revealed 97% leukemic promyelocytes. Despite systemic and CNS therapy, she died due to septic shock by infection and rapid disease progression only 3 days after her admission. Another patient, a 3-yr-old girl, presented with easy bruising and epistaxis, and her CBC showed pancytopenia with increased blasts. BM studies confirmed APL. Quantitative PCR for PML-RARα in the BM cells revealed a PML-RARα/ABL ratio of 0.33 and CSF analysis revealed 9.5% leukemic promyelocytes (2 of 21 cells). She received induction chemotherapy and intrathecal therapy and achieved complete remission (CR) in the BM and CNS. She has been maintained in the CR status for the past 31 months. Thus, patients with APL must be evaluated for CNS involvement if any neurological symptoms are present at the time of diagnosis.
Central nervous system (CNS) involvement is a rare complication of acute promyelocytic leukemia (APL) and is encountered more frequently at the relapse stage than at presentation. The CNS is the most commonly affected site of extramedullary relapse in APL [1, 2]. The incidence of CNS relapse ranges between 0.6% and 2% [2-4]. Furthermore, CNS involvement at the time of presentation is very rare, and only few cases have been reported in medical literature [5-9].
In this paper, we report 2 cases of APL with CNS involvement at the time of disease presentation.
A 43-yr-old woman presented with easy bruising for a month and stuporous mentality for several hours in February 2009. Initial laboratory evaluation showed a white blood cell (WBC) count of 48.6×109/L with 87% blasts, a hemoglobin count of 31 g/L, and a platelet count of 14×109/L. Prothrombin time (PT) and activated partial thromboplastin time (aPTT) at the time of admission were 14.5 sec (59% of normal) and 28.3 sec, respectively. The findings of other coagulation tests were as follows: fibrinogen level, 1.14 g/L; fibrin/fibrinogen degradation product level, 546.8 mg/L; and D-dimer level, 283,600 µg/L. These indicated disseminated intravascular coagulation. Numerous hypergranular promyelocytes (42%) and myeloblasts (41%) were visualized on bone marrow (BM) examination. Immunophenotyping of the BM revealed that leukemic cells were positive for CD13, CD33, CD117, and CD65 and negative for CD34, CD15, and CD2. HLA-DR showed dim positivity. The chromosomal analysis of BM cells showed the karyotype 46,XX,t(15;17)(q22;q21)[3]/46,XX,der(15)t(15;17)(q22;q21),ider(q10)(15;17) in 17 of the 20 metaphase cells. Reverse transcriptase PCR (RT-PCR) showed a bcr1 isoform of the PML-RARα fusion transcript in the BM specimen. For RT-PCR, total RNA was extracted from the BM cells using a High Pure RNA isolation kit (Roche Diagnostics, Mannheim, Germany), and reverse transcription was performed using Moloney murine leukemia virus transcriptase enzyme (Invitrogen, Carlsbad, CA, USA) and a hexanucleotide mixture (Roche Diagnostics). Nested PCR was performed using GeneAmp PCR System 9600 (Perkin-Elmer, Norwalk, CT, USA) [10].
A brain CT scan did not show any tumor or CNS hemorrhage. A lumbar puncture was performed to investigate the cause of her stuporous mentality; and cerebrospinal fluid (CSF) analysis revealed a WBC count of 2.2×109/L, red blood cell (RBC) count of 0.16×1012/L, and leukemic promyelocyte proportion of 97% in the bloody background (Fig. 1). Cytospins were prepared from CSF cells using a Shandon Cytospin 3 (Shandon, Astmoore, UK). The loading volume was 5 drops and centrifugation was performed at 700 rpm for 5 min. Next, Wright-Giemsa staining was carried out. The CSF specimen was not subjected to RT-PCR or FISH analysis.
Induction chemotherapy with all-trans-retinoic acid (ATRA) and idarubicin was initiated and intrathecal methotrexate (20 mg) was administered simultaneously. However, the patient's mentality and clinical condition worsened progressively and she died due to septic shock by infection and rapid disease progression only 3 days after admission.
A 3-yr-old girl presented with easy bruising and epistaxis for several days in August 2007. Her initial laboratory evaluation revealed pancytopenia with a WBC count of 3.8×109/L and 8% blasts, hemoglobin level of 46 g/L, and a platelet count of 27×109/L. Coagulation test results were within the normal range. The BM finding of hypergranular promyelocytes was consistent with the diagnosis of APL. Immunophenotyping of BM leukemic cells showed that they were positive for CD13, CD33, and CD117 and negative for CD34, HLA-DR, and CD2. The chromosomal analysis showed the karyotype 46,XX,t(15;17)(q22;q21) in 7 of 20 metaphase cells. RT-PCR of the BM specimen showed the bcr3 isoform of the PML-RARα fusion transcript and the ratio of PML-RARα/ABL determined by with quantitative PCR was 0.33. The patient had no neurological symptoms. However, a lumbar puncture was done for the purpose of CNS prophylaxis. CSF analysis revealed 9.5% leukemic promyelocytes (2 of 21 cells) with a WBC count of 0.002×109/L without RBCs. The CSF specimen was not subjected to RT-PCR or FISH analysis.
The patient received induction chemotherapy with ATRA, idarubicin, and cytarabine, and intrathecal cytarabine (40 mg) as per the protocol. No leukemic cells were detected during the follow-up CSF examination. She achieved remission in the BM and CNS. She was then prescribed consolidation and maintenance therapy with cytarabine and idarubicin. At present she is alive and in a CR status for 31 months.
APL is a unique disease entity associated with distinctive morphology and chromosomal abnormality, and it is often accompanied by severe coagulopathy [11]. In these cases, performing a lumbar puncture at disease presentation or induction therapy is extremely hazardous because of frequently encountered bleeding diathesis and therefore, not recommended in patients with newly diagnosed APL in general [12]. However, the presence of neurological symptoms such as headache, vertigo, nausea, vomiting, visual disturbance, seizure, and altered mental state [13, 14], necessitate a lumbar puncture both for diagnostic and therapeutic purposes [9, 12]. In our cases, the first patient presented with altered mentality, and the second patient had no neurological symptoms. However, in the hematology and oncology division of the pediatric department in our institution, all APL patients undergo prophylactic lumbar punctures irrespective of their age or presence of neurological symptoms. Chow et al. recommended lumbar puncture at the time of APL diagnosis, immediately after the resolution of coagulopathy in order to diagnose CNS involvement [4].
In Case 2, the 3-yr-old girl was unable to express the disease-related symptoms accurately. In addition, CSF analysis, showed a smaller number of leukemic cells (2 of 21 cells, WBC count, 0.002×109/L) than that in Case 1 (leukemic promyelocytes, 97%; WBC 2.2×109/L).
There have been several reports of patients with APL presenting with CNS involvement in APL at the time of initial diagnosis (Table 1). Two cases of APL with CNS involvement have been reported in Korea [13, 15], and in both of these cases, CNS was affected during relapse: one showed CNS involvement with molecular relapse in the BM, and the second showed CNS involvement with hematologic remission in the BM. To our knowledge, our report is the first to present cases of CNS involvement at the time of diagnosis of APL in Korea.
Treatment of CNS involvement in APL can be diverse and can also be case-specific. It includes local and systemic therapy. CNS therapy comprises of intrathecal chemotherapy, for example, cytarabine, methotrexate and hydrocortisone, and CNS irradiation, while systemic therapy involves the administration of ATRA in addition to chemotherapy [3, 14]. Both our patients received intrathecal methotrexate or cytarabine and systemic chemotherapy, including ATRA.
No molecular studies were performed with the CSF specimen in either of the patients, because cytological examination of CSF was considered sufficient to diagnose CNS involvement. However, this limited the comparison of our cases with a recently reported case [9], because we did not have data on the PML-RARα fusion transcript in the CSF leukemic cells.
In summary, we describe 2 cases of APL with CNS involvement at the time of presentation. Although CNS involvement is a very rare event in APL at the time of initial diagnosis, we believe that APL patients with neurological symptoms must be evaluated for CNS involvement by performing a lumbar puncture.
References
1. Evans GD, Grimwade DJ. Extramedullary disease in acute promyelocytic leukemia. Leuk Lymphoma. 1999; 33:219–229. PMID: 10221502.

2. de Botton S, Sanz MA, Chevret S, Dombret H, Martin G, Thomas X, et al. Extramedullary relapse in acute promyelocytic leukemia treated with all-trans retinoic acid and chemotherapy. Leukemia. 2006; 20:35–41. PMID: 16307026.

3. Montesinos P, Díaz-Mediavilla J, Debén G, Prates V, Tormo M, Rubio V, et al. Central nervous system involvement at first relapse in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline monochemotherapy without intrathecal prophylaxis. Haematologica. 2009; 94:1242–1249. PMID: 19608685.

4. Chow J, Feusner J. Isolated central nervous system recurrence of acute promyelocytic leukemia in children. Pediatr Blood Cancer. 2009; 52:11–13. PMID: 18816805.

5. Kanakura Y, Yonezawa T, Hamaguchi Y, Otsuka A, Matayoshi Y, Kondoh H, et al. Acute promyelocytic leukemia with an intracerebral mass and meningeal involvement after treatment of non-Hodgkin's lymphoma. Cancer. 1987; 59:94–98. PMID: 3466663.

6. Pogliani EM, Fowst C, Marozzi A, Salvatore M, Polli EE. Cerebral parenchymal involvement in acute promyelocytic leukemia. A case report. Haematologica. 1988; 73:71–73. PMID: 3131209.
7. Hara T, Tsurumi H, Yamada T, Sawada M, Moriwaki H. Detection of acute promyelocytic leukemia (APL) cells intermediately differentiated by all-trans retinoic acid in the cerebrospinal fluid: central nervous system involvement in APL. Leuk Lymphoma. 2000; 39:213–215. PMID: 10975402.

8. Classen CF, Debatin KM, Friedrich W, Schulz AS. Long-term remission of APL with a second allogeneic BMT after CNS relapse following HLA-identical allogeneic BMT. Bone Marrow Transplant. 2003; 32:843–846. PMID: 14520432.

9. Collins C, Knoderer H. Central nervous system involvement at the time of presentation in acute promyelocytic leukemia. Pediatr Blood Cancer. 2010; 54:603–605. PMID: 19998465.

10. Gallagher RE, Li YP, Rao S, Paietta E, Andersen J, Etkind P, et al. Characterization of acute promyelocytic leukemia cases with PML-RAR alpha break/fusion sites in PML exon 6: identification of a subgroup with decreased in vitro responsiveness to all-trans retinoic acid. Blood. 1995; 86:1540–1547. PMID: 7632962.

11. Parmar S, Tallman MS. Acute promyelocytic leukaemia:a review. Expert Opin Pharmacother. 2003; 4:1379–1392. PMID: 12877645.

12. Sanz MA, Grimwade D, Tallman MS, Lowenberg B, Fenaux P, Estey EH, et al. Management of acute promyelocytic leukemia: recommendations from an expert panel on behalf of the European LeukemiaNet. Blood. 2009; 113:1875–1891. PMID: 18812465.

13. Bae SH, Ryoo HM, Cho HS, Lee JL, Lee KH, Hyun MS. Meningeal relapse in a patient with acute promyelocytic leukemia: a case report and review of the literature. J Korean Med Sci. 2004; 19:311–314. PMID: 15082912.

14. Vega-Ruiz A, Faderl S, Estrov Z, Pierce S, Cortes J, Kantarjian H, et al. Incidence of extramedullary disease in patients with acute promyelocytic leukemia: a single-institution experience. Int J Hematol. 2009; 89:489–496. PMID: 19340529.

15. Lee HY, Kim KM, Kang MH, Kang JH, Kang KM, Lee GW. Concurrent craniospinal radiotherapy and intrathecal chemotherapy in patient with acute promyelocytic leukemia second relapsed in central nervous system (CNS) following allogeneic stem cell transplantation. J Neurooncol. 2006; 79:73–75. PMID: 16718520.

Fig. 1
Cytospin preparation of the cerebrospinal fluid of Case 1 showing promyelocytes with Auer rods in the cytoplasm. Numerous red blood cells are seen in the background (Wright-Giemsa stain, ×1,000).
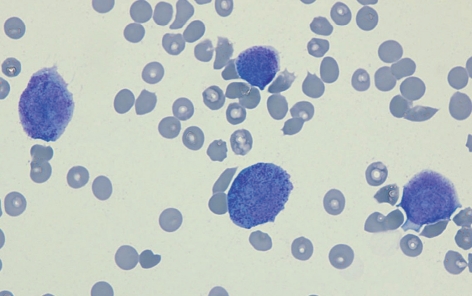
Table 1
Reported cases of acute promyelocytic leukemia with central nervous system involvement at the time of initial diagnosis
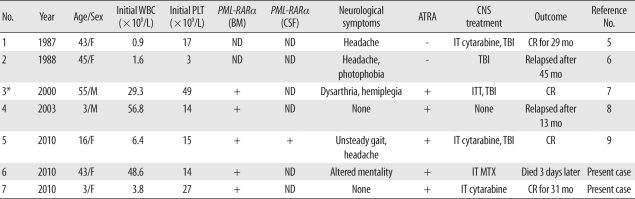
*Probable case: Although lumbar puncture was not performed at diagnosis, follow-up lumbar puncture after complete remission showed numerous immature myelocytes and promyelocytes.
Abbreviations: WBC, white blood cell; PLT, platelet; PML-RARα, promyelocytic leukemia/retinoic acid receptor alpha; BM, bone marrow; CSF, cerebrospinal fluid; ATRA, all-trans-retinoic acid; CNS, central nervous system; ND, not done; IT, intrathecal; TBI, total brain irradiation; CR, complete remission; ITT, intrathecal triple (methotrexate, cytarabine, and prednisolone); MTX, methotrexate.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download