Abstract
Background
Fibrin-related markers (FRM) such as fibrin monomer (FM) and D-dimer (DD) are considered useful biological markers for the diagnosis of disseminated intravascular coagulation (DIC). However, no studies on the diagnostic performance of different FRMs have been published in Korea. The aim of this study was to evaluate the diagnostic performance of FM for DIC in comparison with DD.
Methods
The reference limit of FM was determined based on plasma sample data obtained from 210 control individuals. To evaluate diagnostic performance, FM data from the plasma samples of 139 patients with DIC-associated diseases were obtained for DIC scoring. FM was measured by immunoturbidimetry using STA-LIATEST FM (Diagnostica Stago, France). Patients were classified according to the DIC score as non-DIC, non-overt DIC, or overt DIC. ROC curve analyses were performed.
Results
The reference limit in the control individuals was determined to be 7.80 µg/mL. Patients with DIC-associated diseases were categorized as non-DIC (N=43), non-overt DIC (N=80), and overt DIC (N=16). ROC curve analyses showed that the diagnostic performance of FM was comparable to DD in both non-overt DIC and overt DIC (P=0.596 and 0.553, respectively). In addition, FM had higher sensitivity, specificity, positive predictive value, and negative predictive value than DD for differentiating overt DIC from non-DIC.
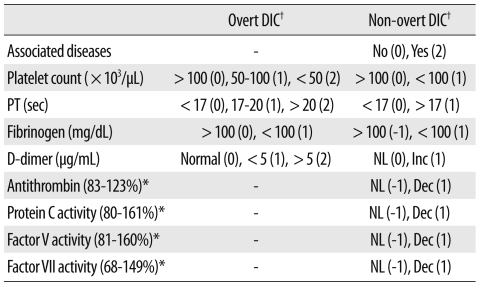
Disseminated intravascular coagulation (DIC) is a systemic thrombohemorrhagic disorder that is associated with hyperactivation of coagulation and secondary fibrinolysis [1]. It is characterized by organ failure resulting from microvascular thrombosis, and bleeding resulting from the consumption of platelets and coagulation factors. Until recently, there was no single laboratory test to confirm the diagnosis of DIC. However, a combination of tests in patients with DIC-associated disease might be helpful in the diagnosis of the disorder. A scoring system was introduced for the diagnosis of overt DIC by the International Society of Thrombosis and Hemostasis (ISTH) in 2001 [1-3]. A score of 5 or greater indicates a diagnosis of overt DIC [2, 3]. The components of the scoring system include a decreased platelet count, prolongation of prothrombin time (PT), increased fibrin-related markers (FRMs), and decreased fibrinogen [1-3].
FRMs include D-dimer (DD), fibrin degradation product (FDP), and fibrin monomer (FM). DD is produced by secondary fibrinolysis of cross-bound fibrin in the post-thrombotic state. In contrast, FM is produced by the release of fibrinopeptide A from fibrinogen by thrombin in a hypercoagulable state. Therefore, DD could be considered a post-thrombotic marker while FM could be considered an impending thrombotic marker [4, 5]. Although some studies showed advantages of FM over DD for the diagnosis or prognostication of DIC [5-8], data for evaluating the diagnostic performance of different types of FRMs is limited. In addition, there were no defined cut-offs of FRMs for the diagnosis of DIC. For this reason, the present study was performed to evaluate the diagnostic performance of FM for DIC in comparison with DD.
To establish a reference limit for FM, plasma samples from 210 control subjects were obtained. They were adult individuals who visited our institute for routine health check-ups and they had normal results in blood tests, including coagulation screening tests. Those with autoimmune diseases, chronic liver diseases, or thrombosis, and those on medication were excluded.
To evaluate the diagnostic performance of FRMs for DIC scoring, FM data from plasma samples were obtained from 139 patients with DIC-associated diseases. According to the DIC scoring system [1-3, 9] (Table 1), the patients were classified into 3 groups as follows: Group 1 without DIC (overt DIC score and non-overt DIC score was zero), Group 2 with non-overt DIC (overt DIC score range, 1-4 points and non-overt DIC score was 1 point or higher), and Group 3 with overt DIC (overt DIC score was 5 points or higher).
All blood samples for coagulation tests were collected into tubes containing 3.2% sodium citrate and were processed within 4 hours after collection. Aliquots of plasma samples were prepared and frozen until the determination of FM. Coagulation tests for DIC scoring were performed using the following reagents (STA-NEOPLASTINE CI PLUS for PT, STA-PTT for activated partial thromboplastin time [aPTT], STA-FIBRINOGEN for fibrinogen, STA-STACHROM AT III for antithrombin [AT], STA-STACHROM PROTEIN C for protein C [PC], STA-DEFICIENT V and VII for coagulation factor V and VII, respectively, STA-LIATEST D-DI for DD, and STA-LIATEST for FM). FDP was measured semi-quantitatively by latex agglutination (FDP PLASMA), and DD and FM were measured by immunoturbidimetric assays. All analyses were performed on a STA-R Evolution coagulation instrument (Diagnostica Stago, Asnieres, France).
To determine the reference limit of FM in the control population, we first checked for the normality of the data using the D'Agostino-Pearson test and eliminated outliers using the D/R ratio rule by Dixon. Hemostatic parameters among the 3 groups were compared by 1-way ANOVA or the Kruskal-Wallis test. The correlation between the DIC score and the levels of FRMs was analyzed, and ROC curve analysis was performed to compare the diagnostic performance. According to the cut-offs of FRMs from the ROC curve, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and the odds ratio were calculated. A P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using MedCalc software (Mariakerke, Belgium).
The plasma levels of FM in the 210 control subjects ranged from 1.64 to 9.66 µg/mL (median, 4.03 µg/mL). The data did not follow a Gaussian distribution. Therefore, the cut-off level was determined to be 7.80 µg/mL using the right-side 95th percentile.
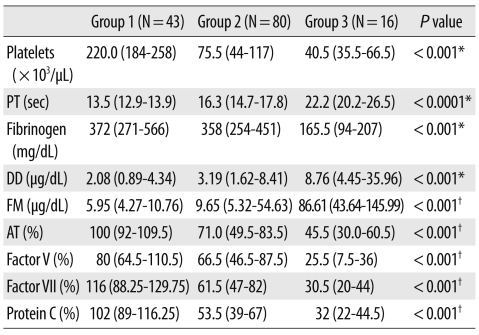
Among the 139 study patients, 43 were classified into Group 1 (without DIC), 80 into Group 2 (with non-overt DIC), and 16 patients into Group 3 (with overt DIC). Malignancies (35%), vascular diseases (29%), and infections (20%) accounted for the majority of underlying diseases in all patients. There were no differences among 3 groups in the distribution of underlying diseases. All hemostatic parameters differed significantly among the 3 groups (Table 2). The values of each parameter in Group 3 were significantly higher than in Group 2, and those in Group 2 were significantly higher than in Group 1. The median values of DD in Group 1, Group 2, and Group 3 were 2.08 µg/mL, 3.19 µg/mL, and 8.76 µg/mL, respectively (Fig. 1A; P<0.001). The median values of FM in Group 1, Group 2, and Group 3 were 5.95 µg/mL, 9.65 µg/mL, and 86.61 µg/mL, respectively (Fig. 1B; P<0.001). There was a statistically significant correlation between the levels of both FM and DD and the DIC score (r=0.3975, P<0.0001 for FM, and r=0.4280, P<0.0001 for DD). DD and FM were also significantly correlated in Group 1 and Group 2 (r=0.5556, P<0.0001 in Groups 1 and 2 combined; r=0.6487, P<0.0001 in Group 1; and r=0.5519, P<0.0001 in Group 2). However, there was no significant correlation between DD and FM in Group 3 (with overt DIC; P=0.104). Two patients in Group 3 showed extremely low levels of DD (0.56 µg/mL and 1.9 µg/mL), while they had relatively high levels of FM (10.6 µg/mL and 61.33 µg/mL, respectively).
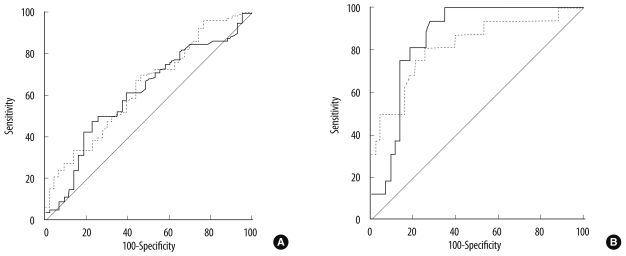
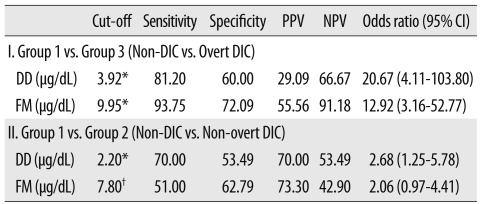
On ROC curve analyses, the diagnostic performance of FM and DD were similar in all 3 groups (Fig. 2, P=0.596 in Group 2, and P=0.553 in Group 3). To discriminate Group 3 from Group 1, the values with the largest area under the curve (AUC) were set as the cut-offs for DD and FM (3.92 µg/mL and 9.95 µg/mL, respectively). Below these cut-offs, FM had a higher sensitivity, specificity, PPV, and NPV than DD for differentiating overt DIC from non-DIC (Table 3). To discriminate Group 2 from Group 1, the cut-offs for DD and FM were 2.2 µg/mL and 7.80 µg/mL, respectively. DD had a higher sensitivity, NPV, and odds ratio than FM for differentiating non-overt DIC from non-DIC (Table 3).
Hypercoagulation and secondary fibrinolysis are the major pathologic mechanisms in DIC. Laboratory data based on the clinical condition might be critical for the diagnosis of DIC. Among the coagulation markers (PT, platelets, fibrinogen, FRM) in the DIC scoring system, FRMs such as FM and DD best reflect the underlying pathology of DIC. Because the measurement of FRMs has not been standardized, local cut-off values remain to be defined for the application of the ISTH DIC scoring system. For the diagnosis of DIC, DD was very sensitive but not specific. However, little is known about the diagnostic performance of FM in Korean patients with DIC.
The present study established a reference limit for FM in healthy individuals and evaluated the diagnostic performance of FM in patients with DIC-associated diseases. We established the cut-off for FM in 210 healthy individuals as 7.80 µg/mL. The measurement of FM is based on immunoturbidimetry, which might be affected by interference from hemolysis, bilirubinemia, and lipidemia. We excluded samples with abnormal routine laboratory findings. Okajima et al. [10] reported that the level of FM in 116 healthy volunteers was less than 6.6 µg/mL using an ELISA method. Hamano et al. [11] defined 6.1 µg/mL of FM as the clinical baseline using a latex immunoturbidimetric assay.
In our study, a comparison of the ROC curves of FM and DD showed that FM was comparable to DD as a marker for the diagnosis of both non-overt DIC and overt DIC. Previous studies showed some controversial data [6, 12]. According to Dempfle et al. [6], FM was better indicator than DD for the early diagnosis of DIC and its prognosis. In contrast, large prospective studies by multiple institutions showed that FM was not a useful marker for the differentiation of "pre-DIC" from "not-DIC" [12]. By the ISTH, "pre-DIC" was defined as the state within a week before the onset of DIC, while "non-overt DIC" was defined as the state with hemostatic dysfunction that is compensated [3]. We hypothesized that FM might be a more useful marker for detection of the early phase of non-overt DIC with compensation. The level of FM in Group 2 with non-overt DIC was significantly higher than that in Group 1 without DIC, and was lower than that in Group 3 with overt DIC. Differences in DD were also observed among the 3 Groups. However, comparison of ROC curves for FM and DD in the diagnosis of non-overt DIC showed that FM was not a better indicator than DD. Theoretically, FM would be produced earlier than DD in a hypercoagulable state, while DD would be produced after thrombosis and fibrinolysis. Therefore, increased levels of FM without an increase in DD might enhance the diagnostic power of FM. In the present study, there were 2 cases showing an increase in FM with no increase in DD despite the diagnosis of overt DIC. This suggested that for the diagnosis of overt DIC, FM is more sensitive than DD; however, there was no difference between the ROC curves of DD and FM. Assuming that the presence of heparin might influence thrombin, which in turn might influence the formation of FM, we investigated the history of anticoagulation, and did not find any differences among the 3 Groups.
In the present study, we defined cut-offs for the FRMs based on the values with the largest AUC in ROC curves and the reference limit in the control population. Using the suggested cut-offs, FM showed lower sensitivity than DD in patients with non-overt DIC, and higher sensitivity in patients with overt DIC. DD might be obtained from both intravascular coagulation and extravascular sources such as trauma and local inflammation, while FM might result from only intravascular sources [6]. Therefore, FM might have higher sensitivity for the diagnosis of overt DIC.
The present study had some limitations. First, the number of the patients was very small, especially the number of patients with overt DIC. The magnitude of FM elevation might be influenced by other factors such as medications or the nature of underlying diseases. Therefore, some patients with non-overt DIC had levels of FM that were more elevated than in patients with overt-DIC. Second, we could not investigate the levels of FM at the state of pre-DIC in the present study. By definition, pre-DIC might reflect the early phase of DIC more than non-overt DIC. Lastly, we would like discuss the clinical utility of AT, PC, and factor V and factor VII for non-overt DIC included in this study. The clinical utility of these biomarkers in non-overt DIC is still under investigation [2, 3, 9, 13, 14]. In addition, these tests are typically not available as stat tests, as is the case at the authors' institution, which also limits their clinical utility.
In summary, we investigated the reference limit of FM in healthy adults and evaluated the diagnostic performance of FM in terms of the sensitivity, specificity, PPV, NPV, and AUC for the diagnosis of DIC. FM had performance comparable to DD for the diagnosis of DIC.
Acknowledgement
Reagents for the measurement of FM were provided free of charge by the manufacturers.
References
1. Levi M, Toh CH, Thachil J, Watson HG. British Committee for Standards in Haematology. Guidelines for the diagnosis and management of disseminated intravascular coagulation. Br J Haematol. 2009; 145:24–33. PMID: 19222477.

2. Toh CH, Hoots WK. The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost. 2007; 5:604–606. PMID: 17096704.

3. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001; 86:1327–1330. PMID: 11816725.

4. Wada H, Sakuragawa N. Are fibrin-related markers useful for the diagnosis of thrombosis? Semin Thromb Hemost. 2008; 34:33–38. PMID: 18393141.

5. Wada H, Sase T, Matsumoto T, Kushiya F, Sakakura M, Mori Y, et al. Increased soluble fibrin in plasma of patients with disseminated intravascular coagulation. Clin Appl Thromb Hemost. 2003; 9:233–240. PMID: 14507112.

6. Dempfle CE, Wurst M, Smolinski M, Lorenz S, Osika A, Olenik D, et al. Use of soluble fibrin antigen instead of D-dimer as fibrin-related marker may enhance the prognostic power of the ISTH overt DIC score. Thromb Haemost. 2004; 91:812–818. PMID: 15045145.

7. Ieko M, Nakabayashi T, Tarumi T, Naito S, Yoshida M, Kanazawa K, et al. Soluble fibrin monomer degradation products as a potentially useful marker for hypercoagulable states with accelerated fibrinolysis. Clin Chim Acta. 2007; 386:38–45. PMID: 17803984.

8. Wada H, Wakita Y, Nakase T, Shimura M, Hiyoyama K, Nagaya S, et al. Increased plasma-soluble fibrin monomer levels in patients with disseminated intravascular coagulation. Am J Hematol. 1996; 51:255–260. PMID: 8602623.

9. Toh CH, Downey C. Performance and prognostic importance of a new clinical and laboratory scoring system for identifying non-overt disseminated intravascular coagulation. Blood Coagul Fibrinolysis. 2005; 16:69–74. PMID: 15650549.

10. Okajima K, Uchiba M, Murakami K, Okabe H, Takatsuki K. Determination of plasma soluble fibrin using a new ELISA method in patients with disseminated intravascular coagulation. Am J Hematol. 1996; 51:186–191. PMID: 8619398.

11. Hamano A, Umeda M, Ueno Y, Tanaka S, Mimuro J, Sakata Y. Latex immunoturbidimetric assay for soluble fibrin complex. Clin Chem. 2005; 51:183–188. PMID: 15514091.

12. Okamoto K, Wada H, Hatada T, Uchiyama T, Kawasugi K, Mayumi T, et al. Frequency and hemostatic abnormalities in pre-DIC patients. Thromb Res. 2010; 126:74–78. PMID: 20452653.

13. Egi M, Morimatsu H, Wiedermann CJ, Tani M, Kanazawa T, Suzuki S, et al. Non-overt disseminated intravascular coagulation scoring for critically ill patients: the impact of antithrombin levels. Thromb Haemost. 2009; 101:696–705. PMID: 19350114.

14. Oh D, Jang MJ, Lee SJ, Chong SY, Kang MS, Wada H. Evaluation of modified non-overt DIC criteria on the prediction of poor outcome in patients with sepsis. Thromb Res. 2010; 126:18–23. PMID: 20079919.

Fig. 1
Box plots of the plasma concentration of D-dimer (DD) (A) and fibrin monomer (FM) (B) in the 3 Groups. Data are expressed as median ±2SD. The statistical significance between the 2 groups was determined by 1-way analysis of variance.
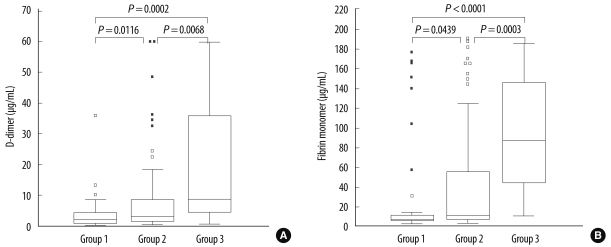
Fig. 2
ROC curves of D-dimer (DD) and fibrin monomer (FM) for the diagnosis of disseminated intravascular coagulation (DIC); (A) In Group 2 (non-overt DIC), the area under the curve (AUC) of DD and FM were 0.638 and 0.610, respectively (P=0.596). (B) In Group 3 (overt DIC), the AUC of DD and FM were 0.819 and 0.858, respectively (P=0.553).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download