Abstract
Purpose
Single-port laparoscopic surgery is a rapidly advancing technique in laparoscopic surgery. However, there is currently limited evidence on the learning curve for this procedure. The aim of this study was to estimate the number of single port laparoscopic cholecystectomies required until improvement in the performance of the technique ceases.
Methods
This is a descriptive, single-center study using routinely collected clinical data from 70 patients who underwent single port laparoscopic cholecystectomy between May 2009 and June 2010 at Dong-A University Medical Center in Busan, Korea. The review includes the mean operating time, conversion cases, intra-operative GB perforation, post-operative wound infection and mean hospital stay.
Results
The mean operating time of the first 30 cases (the learning period) was 91.83 minutes. After 30 operations (the experience period), it plateaued to an average of 75.25 minutes, which remained steady in the next 40 operations - a reduction of more than 16%. Reduction in the operating time was significant (P<0.001) between the learning period and the experience period. Other factors including additional ports, intraoperative gall bladder perforation, mean hospital stay, post-operative wound infection were not significantly different between the two periods.
Laparoscopic surgery has obvious benefits, such as diminished postoperative pain, improved safety, reduced length of hospital stay and enhanced esthetic result. As such, laparoscopic cholecystectomy is now accepted as the gold standard for the management of cholelithiasis and gall bladder (GB) polyps.(1,2)
Conventional laparoscopic cholecystectomy used 3 or 4 ports. The use of multiple trocars is the solution for several challenges. At first, it solved problems associated with the conventional instrument's limited degree of freedom. Second, there is a fixed working envelope surrounding each port created by fulcrum motion around the insertion point of each trocar. Third, it solved the hand-eye dissociation and the two-dimensional field-of-vision. Finally, multiple trocars overcome the deficit of experienced skill.(3-5)
On the other hand, additional ports contribute to postoperative pain, diminish cosmesis and they increase the risks of bleeding, hernia formation and organ damage.
With continued evolution of laparoscopic minimally invasive surgery, fewer incisions and trocars are being used to perform laparoscopic procedures. Since transumbilical cholecystectomy was first described in 1999, many surgeons have advanced this technique.(6) Safety and feasibility of single port laparoscopic cholecystectomy (SPLC) have been proven in many studies.(7,8) Many surgeons currently perform single port laparoscopic surgery, particularly in general surgery for appendicitis and benign gall bladder disease. We have been performing SPLC at our institution since May, 2009.(9,10)
Although SPLC are commensurate with the adoption of conventional laparoscopic cholecystectomy, it requires more subtle skill than does conventional laparoscopic cholecystectomy. Because the instruments and camera of SPLC are inserted in the same site, the advantages of multi-port are lost: it compels the instrument and camera to fight for space in the intra-abdomen and extra-abdomen. Therefore, surgeon must predict these situations and avoid them by delicate handling of the instruments and keeping accurate orientation. Some surgeons use articulating instruments developed to prevent clashes of instruments. However, movement of the instruments' extra-abdominal handle and intra-abdominal acting portion is different. That is, SPLC requires another orientation different from conventional laparoscopic cholecystectomy. Therefore, SPLC requires a different learning curve, even if the surgeon is skilled at conventional laparoscopic surgery.
The objective of this study was to investigate a surgeon's experience with SPLC and delineate the learning curve for this technically demanding procedure, using improvement in operating time as a proxy for technical skill.
All patients underwent elective SPLC by a single surgeon between May 2009 and June 2010 at the Dong-A University Medical center in Busan, Korea were included in this study.
Initially, we selected patients diagnosed with GB stone without radiological evidence of GB wall thickening (Computed tomography (CT) or abdominal ultrasonography (U/S)) who did not have classic history of abdominal pain. However, after 10 cases, patients with cholecystitis and right upper quadrant pain (RUQ) caused by GB stone (determined by the degree of GB wall thickening on CT or U/S) were included. Over time, these cases became more common.
Incidentally found GB polyp over 8 mm was another indication for SPLC. However, if the size of GB polyps were less than 10 mm, an operation was only performed when the patient wanted.
None of the patients had a prior history of upper abdominal surgery. Fifteen (n=15) patients had undergone previous surgery. The most common operative histories were appendectomy, cesarean section delivery (c/sec) and hysterectomy. In the first 20 cases, patients with body mass index (BMI) over 25 were excluded, but BMI was not an exclusion criterion thereafter. Preoperative preparation, anesthesia and preoperative antibiotics were similar to that in traditional laparoscopic technique.
Single port laparoscopic cholecystectomies were performed under general anesthesia and all the patients were admitted to hospital one day before the operation. After induction of anesthesia, the patient was placed in the lithotomy position. The operating surgeon stood between the patient's legs, and the assistant/camera operator was stood on the patient's left side. Monitors were placed above the patient's shoulders, and the scrub nurse was positioned on the patient's right side.
A midline transumbilical incision of 25 mm was made through the base of the umbilicus. In the early first 35 cases, an umbilical port was made using an Alexis® Wound Retractor (Applied Medical, Rancho Santa Margarita, CA, USA) and a surgical glove. After 35 cases, a commercial multi-channel port was used.
The camera was placed through the central trocar. We used 10 mm and 5 mm 30-degree laparoscope of standard length, and a flexible 10 mm 0-dgree laparoscope of standard length. Lateral trocars are used for the two dissecting instruments, a clip applier and an electrocautery dissection instrument.
Only articulating ins trument were used in the first 30 patients of the study, yet in later cases straight instruments, identical to that used in traditional laparoscopic cholecystectomy, were also used along with articulating instruments.
In all cases, the cystic duct was clipped with a 10 mm Hem-o-Lok clip® and the cystic artery was clipped with a 5 mm Hem-o-Lok clip®. After dividing the duct and artery, articulating hook electrocautery was used to dissect the gall bladder from its bed in a standard bottom-to-top fashion. In each case, the gall bladder was directly removed through the port site without a catch bag.
The parameters studied were operating time (mean, range), number of operations over 90 minutes and under 75 minutes, conversion rate, incidence of postoperative wound infection, intra-operative GB perforation and the mean hospital day. Operating time was defined as time in minutes from the first cutting of skin to final skin closure. The observed differences were subjected to statistical analysis using Student's t test and two sided Fisher's exact tests: differences were considered statistically significant if P-values<0.05.
From May, 2009 to June, 2010, 71-single-port laparoscopic cholecystectomies were performed by one general surgeon, who was in his fourth decade of life, with different assistants to control the laparoscope, at Dong-A University Medical Center, Busan, Korea.
Only one patient was excluded because stone in the cystic duct compressed the common bile duct and created a fistula between the GB and the common bile duct. Open conversion, cholecystectomy and Roux en Y hepaticojejunostomy were performed instead of SPLC.
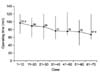
The mean operating time of the first, second and third set of 10 cases was 97.5, 90 and 88 minutes, respectively, but this fell to 77 min in the fourth set of 10 cases, and the mean operating time did not significantly vary in the last four quintiles (77, 76, 75, 67.6 minutes, respectively) (Fig. 1).
Table 1 lists the differences in operating time for the 70 operations. The operating time of the first 10 cases was 97.5 minutes, and the operating time continued to decrease. However, after the first 30 cases, the extent of decreased time dwindled. Operating time decreased with reduction in the number of long operations, and an increase in the number of short ones, and a significant cut-off again appeared to occur after 30 operations.
The demographic and preoperative data are presented in Table 2. There were no statistically significant differences between the learning and experienced periods.
Table 3 lists some of the measured parameters for the 2 groups (the learning period vs. the experienced period). The mean operating time of the first 30 cases was 91.83 minutes. After these 30 operations, the mean operation time reached a plateau of 75.25-minute, which remained steady for the next 40 operations, with a reduction of more than 16%, compared to the first thirty operations. Reduction in operating time was significant (P<0.001) between the learning period and the experienced period. But others factors such as additional ports, intra-operative GB perforation, mean hospital stay, post-operative wound infection, were not significantly different.
Seventeen (n=17) patients required conversion to multi-port laparoscopic surgery. Ten (n=10) were converted to two-port cholecystectomy: the second port was placed in the epigastric area for improved cephalad retraction and bleeding control. The other 7 conversions were made to traditional three-port cholecystectomy.
Of the patients converted to multiport laparoscopy, two (n=2) were converted because of laparoscopic instrument's malfunction, and the others were due to inadequate visualization of Calot's triangle because of severe obesity and adhesion. No conversion was performed due to complications, and no conversion resulted in complication.
There were 14 cases (20%) of bile leakage secondary to GB perforation during the operation. Among the 14 cases, there were 6 cases (8.6%) of GB polyp. Of all the GB polyp cases diagnosed on pre-operative radiologic study, none were confirmed as GB cancer by post-operative pathological study.
Three patients developed wound infection after surgery and they recovered with only simple dressing. There were no reoperations or major long-term sequelae associated with single-port cases, such as bile leakage, port site hernia, a postoperative fluid collection or bleeding.
Intuitively, we would predict the outcomes of this study: surgeons require progressively less time to perform SPLC the more they operate. Yet, we elected to investigate the exact point where operating time becomes stable. The duration and magnitude of continued improvement were not measured. As such, this report documents the actual number of cases for which improvement continues and the actual amount of improvement that is possible according to operating time.
It is very difficult to determine the exact point where the surgeon's technical skills cease to improve, because it depends on the chosen variable. For example, the range of operating time stabilized, the mean operating time plateaued and the duration of the longest or shortest operations became constant.(11) Therefore, we used cohorts of 10 patients to show a general length and shape of the learning curve, rather than calculating exact cut-off points. As for the mean operating time, there was a statistically significant difference between the first 30 operations and the subsequent 40 operations, without further statistically significant differences between the last four cohorts of 10 patients.
The overall shape of the leveling learning curve conforms to what is known about learning in other areas,(12-14) suggesting that our findings should have relevance for all surgeons. Thus, from our data, it would be reasonable to deduce that the learning curve for SPLC is in the order of 30 operations.
As shown in Table 1, the greatest contributor to shortened mean operating time is increased number of short operations (below 75 min), and decreased number of long operations (over 90 min). That is, as the operator became experienced in handling the instruments and possesses accurate orientation, the operations that previously took a long time became shortened.
Although the range of operating time did not decrease, the number of operation that took a long time (over 90min) decreased. We think that is due to an increased number of difficult cases. As the indications for single port operation increased, cholecystitis, GB empyema and biliary colic pain were included, although there was no statistically significant increase (P=0.471, 0.108). Expanding the indications can influence the longest operating time of each cohort, so, the range of operating time did not contract.
Because SPLC goes hand-in hand with performing conventional laparoscopic cholecystectomy, for surgeons who are not experienced in laparoscopic operations (that is, the surgeon who cannot proficiently use laparoscopic instruments and is not used to hand-eye dissociation or a two-dimensional field-of-view), an initial training period is usually required to become proficient in complex procedures by continuous repetition. In fact, Andrus et al.(11) and Hunter et al.(15) described that the learning curve of conventional laparoscopic cholecystectomy for surgeons who had no prior experience in laparoscopic surgery was 200 case and 83 case, respectively. Solomon et al.(16) and Kravetz et al.(17) described that the learning curve of SPLC for a surgeon who is experienced in conventional laparoscopic surgery is 10 cases and 5 cases, respectively. As seen these reports, even though SPLC requires a high degree of special resolution, dexterity, technical skill and accurate orientation, the learning curve for an experienced laparoscopic surgeon is shorter. Naturally, if SPLC is performed by a surgeon who is not experienced with conventional laparoscopic surgery, the learning curve must be longer.
Our suggestion of approximately thirty cases to become proficient in single port laparoscopic cholecystectomy is just one surgeon's initial experience and this represents a self-taught technique. The learning curve of SPLC will be shortened if there is a formal training course in SPLC, close intra-operative supervision by specialist practitioners is available and the surgeon receives assistance from other well-trained staff.(20,21)
Surgeons generally think articulating long instruments are useful for SPLS. These were developed to overcome the limitations of older instruments for adequate retraction and dissection, and to overcome poor surgical field visibility.(18,19) These instruments include Autonomy Laparo-Angle (Cambridge Endo, Framingham) and Roticulator (Covidien, Norwalk, CT, USA). But the large sized handle of articulating instruments makes surgeons uncomfortable, and large handles cause extra-abdominal clashing of instruments, and they do give enough strength to the instrument end for traction of the GB. Therefore, after about 30 cases, we used straight instrument for GB traction and articulating instrument for dissecting. As such, the most important factor that influenced operating time was not the instruments, but the surgeon's skill to prevent fighting of the instruments and the camera.
However, the study did not demonstrate reduction in conversion rate, intra-operative GB perforations, postoperative wound complications and mean hospital stay with experience despite significant reduction in operating time. Possible explanation for this paradox is the increased number of complex and high risk cases. Similar finding were reported by Marusch et al. in a multi-center study on 1,658 patients.(22)
We suggest that the learning curve for SPLC for a surgeon with prior conventional laparoscopic cholecystectomy experience and for a self taught single port technique should be around 30 cases. If there is good training by a skilled SPLS surgeon, and development of convenient instruments, surgeons may become proficient in SPLS in less than thirty cases. On the other hand, the learning curve may become steeper in surgeons who are not experienced with conventional three-port laparoscopic cholecystectomy, or who do not possess skills in advanced laparoscopic surgery.
The limitation of this study is small number of patients included, and the operations were performed by one surgeon at one center. A study with a larger cohort across multiple centers by many surgeons should be performed to accurately determine the learning curve for SPLC.
Figures and Tables
Fig. 1
Mean operating time and Range. The mean operating time of each set of 10 cases continued to decrease. However, after the first 30 cases, the extent of the reduced time dwindled and the mean operation time reached a plateau, which remained steady for the next 40 operations. On the other hand, the range of operating time did not decrease.
References
1. Peters JH, Ellison EC, Innes JT, Liss JL, Nichols KE, Lomano JM, et al. Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann Surg. 1991. 213:3–12.
2. Yi NJ, Han HS, Kim YW, Min SK, Choi YM. The safety of a laparoscopic cholecystectomy in acute cholecystitis in high-risk patients older than sixty with stratification based on ASA score. Minim Invasive Ther Allied Technol. 2006. 15:159–164.
3. Leung KF, Lee KW, Cheung TY, Leung LC, Lau KW. Laparoscopic cholecystectomy: two-port technique. Endoscopy. 1996. 28:505–507.
4. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997. 84:695.
5. Ramachandran CS, Arora V. Two-port laparoscopic cholecystectomy: an innovative new method for gallbladder removal. J Laparoendosc Adv Surg Tech A. 1998. 8:303–308.
6. Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the "critical view of safety" technique. J Gastrointest Surg. 2009. 13:498–503.
7. Edwards C, Bradshaw A, Ahearne P, Dematos P, Humble T, Johnson R, et al. Single-incision laparoscopic cholecystectomy is feasible: initial experience with 80 cases. Surg Endosc. 2010. 24:2241–2247.
8. Erbella J Jr, Bunch GM. Single-incision laparoscopic cholecystectomy: the first 100 outpatients. Surg Endosc. 2010. 24:1958–1961.
9. Hong TH, Kim HL, Lee YS, Kim JJ, Lee KH, You YK, et al. Transumbilical single-port laparoscopic appendectomy (TUSPLA): scarless intracorporeal appendectomy. J Laparoendosc Adv Surg Tech A. 2009. 19:75–78.
10. Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009. 23:1393–1397.
11. Voitk AJ, Tsao SG, Ignatius S. The tail of the learning curve for laparoscopic cholecystectomy. Am J Surg. 2001. 182:250–253.
12. Teplitz CJ. The Learning Curve Deskbook: A Reference Guide to Theory, Calculations and Applications. 1991. New York: Quorum Books.
13. Mishne JM. The Learning Curve: Elevating Children's Academic and Social Competence. 1996. Dunmore, Penn: Jason Aronson.
14. Birren JE, Schaie KW. Handbook of the Psychology of Aging. 1990. San Diego: Academic Press.
15. Hunter JG, Sackier JM, Berci G. Training in laparoscopic cholecystectomy Quantifying the learning curve. Surg Endosc. 1994. 8:28–31.
16. Solomon D, Bell RL, Duffy AJ, Roberts KE. Single-port cholecystectomy: small scar, short learning curve. Surg Endosc. 2010. 24:2954–2957.
17. Kravetz AJ, Iddings D, Basson MD, Kia MA. The learning curve with single-port cholecystectomy. JSLS. 2009. 13:332–336.
18. Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009. 23:1419–1427.
19. Podolsky ER, Rottman SJ, Poblete H, King SA, Curcillo PG. Single port access (SPA) cholecystectomy: a completely transumbilical approach. J Laparoendosc Adv Surg Tech A. 2009. 19:219–222.
20. Hasan A, Pozzi M, Hamilton JR. New surgical procedures: can we minimise the learning curve? BMJ. 2000. 320:171–173.
21. Tekkis PP, Senagore AJ, Delaney CP, Fazio VW. Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg. 2005. 242:83–91.
22. Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, et al. Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc. 2001. 15:116–120.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download