Abstract
Dermatofibrosarcoma protuberans is a rare tumor that occurs in the dermis or subcutaneous tissue of the trunk or extremities in relatively young adults. There are few reports of Dermatofibrosarcoma protuberans associated with pregnancy. We experienced a 28-year-old pregnant female patient with an abdominal wall mass, which grew rapidly during pregnancy. Excisional biopsy was performed and the pathologic diagnosis was fibrosarcoma transformed from Dermatofibrosarcoma protuberans. Dermatofibrosarcoma protuberans showed a positive CD34 immunostaining while fibrosarcoma showed a negative CD34. There was no recurrence or metastasis with the follow up period of 2 years. We report here a rare case of Dermatofibrosarcoma protuberans aggravated during pregnancy with a review of the literature.
Figures and Tables
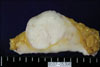 | Fig. 1Gross appearance of dermatofibrosarcoma protuberans.Two nodules abut each other and the total lesion is 5.0×4.5×3.5 cm in three dimensions. The upper right portion involving the skin dermis and subcutis has firm consistency, and shows a pale-gray homogeneous and solid cut surface. In the lower left portion of the lesion, an ovoid smooth solid and rubbery nodule is exhibited and the tumor size is 3.5× 2.4 cm in surface dimension. |
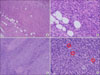 | Fig. 2Microscopic findings of dermatofibrosarcoma protuberans. Dermatofibrosarcoma portion composed of slender spindle cells is arranged in a storiform pattern. This portion intricately interdigitates with normal fat. H&E staining, ×100 (A). A high power view shows a uniform population of slender fibroblasts, an inconspicuous vasculature and interdigitating normal fat cells. H&E staining, ×400 (B). Fibrosarcoma area shows increased cellularity with a long fascicle pattern. H&E staining, ×100 (C). A high power view shows frequent mitotic figures (red circles). H&E staining, ×400 (D). |
 | Fig. 3Microscopic findings of the transitional zone. Dermatofibrosarcoma protuberans (upper right portion) showing the transition to fibrosarcoma (lower left corner). H&E staining, ×40 (A). Dermatofibrosarcoma protuberans (upper right) shows positive CD34 immunostain result while fibrosarcoma (lower left) shows negative CD34 immunoreactivity ×40 (B). |
References
1. Parlette LE, Smith CK, Germain LM, Rolfe CA, Skelton H. Accelerated growth of dermatofibrosarcoma protuberans during pregnancy. J Am Acad Dermatol. 1999. 41:778–783.
2. Fiore M, Miceli R, Mussi C, Lo Vullo S, Mariani L, Lozza L, et al. Dermatofibrosarcoma protuberans treated at a single institution: a surgical disease with a high cure rate. J Clin Oncol. 2005. 23:7669–7675.
3. Gloster HM Jr. Dermatofibrosarcoma protuberans. J Am Acad Dermatol. 1996. 35:355–374.
4. Hoffman E. Ueber alas knollentribende fibrosarkam der haut (dermatofibrosarcoma protuberans). Dermatol Z. 1925. 43:1–28.
5. Kim SH, Chang MC, Lee WA, Oh SK. Dermatofibrosarcoma protuberans in breast. J Korean Surg Soc. 2007. 72:63–65.
6. Haycox CL, Odland PB, Olbricht SM, Piepkorn M. Immunohistochemical characterization of dermatofibrosarcoma protuberans with practical applications for diagnosis and treatment. J Am Acad Dermatol. 1997. 37:438–444.
7. Handolias D, McArthur GA. Imatinib as effective therapy for dermatofibrosarcoma protuberans: proof of concept of the autocrine hypothesis for cancer. Future Oncol. 2008. 4:211–217.
8. Morrison AE, Lang PG. Case of rapidly enlarging dermatofibrosarcoma protuberans during pregnancy followed by metastasis in the absence of local recurrence. Dermatol Surg. 2006. 32:125–127.
9. Bigby SM, Oei P, Lambie NK, Symmans PJ. Dermatofibrosarcoma protuberans: report of a case with a variant ring chromosome and metastases following pregnancy. J Cutan Pathol. 2006. 33:383–388.
10. Abbott JJ, Oliveira AM, Nascimento AG. The prognostic significance of fibrosarcomatous transformation in dermatofibrosarcoma protuberans. Am J Surg Pathol. 2006. 30:436–443.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download