Abstract
Purpose
The diagnostic methods for examining suspicious lesions in the breast are becoming less invasive, like core-needle biopsy. Yet, the risk of invasion has been reported to be up to 47% for patients with ductal carcinoma in situ (DCIS) initially diagnosed by core-needle biopsy. The value of sentinel lymph node biopsy (SLNB) for DCIS has not been clearly proved. We searched for the factors associated with invasiveness of preoperatively diagnosed DCIS, and we determined the indications for performing SLNB for patients with preoperatively diagnosed DCIS.
Methods
Between October 1997 and December 2008, we retrospectively reviewed 135 patients with DCIS that was initially diagnosed by core-needle biopsy or other biopsy methods. We compared the invasive breast cancer group, which was finally diagnosed with the pure DCIS group in regards to clinical, radiological, and pathological factors.
Results
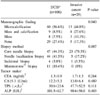
21.5% of the patients with initial diagnosis of DCIS were finally diagnosed with invasive breast cancer. On univariate analysis, the statistically meaningful factors for invasiveness were palpable lesion (P<0.0001), core-needle diagnosis (P=0.007), large tumor size (P=0.028), high nuclear grade (P=0.002), and negative estrogen receptor (P=0.005). On multivariate analysis, a palpable lesion was the only independent risk factor (odds ratio 3.9 (1.1 to 13.8); P=0.035). Axillar lymph node metastases were found in three patients in the invasive cancer group. There was no lymph node metastasis in the DCIS group.
References
1. The Consensus Conference Committee. Consensus Conference on the classification of ductal carcinoma in situ. Cancer. 1997. 80:1798–1802.
2. Schwartz GF, Solin LJ, Olivotto IA, Ernster VL, Pressman PI. Consensus conference on the treatment of in situ ductal carcinoma of the breast, April 22-25, 1999. Cancer. 2000. 88:946–954.
3. Mokbel K. Towards optimal management of ductal carcinoma in situ of the breast. Eur J Surg Oncol. 2003. 29:191–197.
4. Anderson BO. Axillary metastases with DCIS: is the glass half empty or half full? Ann Surg Oncol. 2000. 7:631–633.
5. Meijnen P, Peterse JL, Oldenburg HS, Woerdeman LA, Rutgers EJ. Changing patterns in diagnosis and treatment of ductal carcinoma in situ of the breast. Eur J Surg Oncol. 2005. 31:833–839.
6. Meunier M, Clough K. Fine needle aspiration cytology versus percutaneous biopsy of nonpalpable breast lesions. Eur J Radiol. 2002. 42:10–16.
7. Dillon MF, McDermott EW, Quinn CM, O'Doherty A, O'Higgins N, Hill AD. Predictors of invasive disease in breast cancer when core biopsy demonstrates DCIS only. J Surg Oncol. 2006. 93:559–563.
8. Jackman RJ, Burbank F, Parker SH, Evans WP 3rd, Lechner MC, Richardson TR, et al. Stereotactic breast biopsy of nonpalpable lesions: determinants of ductal carcinoma in situ underestimation rates. Radiology. 2001. 218:497–502.
9. Yen TW, Hunt KK, Ross MI, Mirza NQ, Babiera GV, Meric-Bernstam F, et al. Predictors of invasive breast cancer in patients with an initial diagnosis of ductal carcinoma in situ: a guide to selective use of sentinel lymph node biopsy in management of ductal carcinoma in situ. J Am Coll Surg. 2005. 200:516–526.
10. Goyal A, Douglas-Jones A, Monypenny I, Sweetland H, Stevens G, Mansel RE. Is there a role of sentinel lymph node biopsy in ductal carcinoma in situ?: analysis of 587 cases. Breast Cancer Res Treat. 2006. 98:311–314.
11. Meijnen P, Oldenburg HS, Loo CE, Nieweg OE, Peterse JL, Rutgers EJ. Risk of invasion and axillary lymph node metastasis in ductal carcinoma in situ diagnosed by core-needle biopsy. Br J Surg. 2007. 94:952–956.
12. Wilkie C, White L, Dupont E, Cantor A, Cox CE. An update of sentinel lymph node mapping in patients with ductal carcinoma in situ. Am J Surg. 2005. 190:563–566.
13. Bae JS, Song BJ, Kim DC, Suh YJ, Park WC, Kim JS, et al. Predictive factors of residual invasive breast cancer after core biopsy for ductal carcinoma in situ. J Breast Cancer. 2008. 11:36–39.
14. Moran CJ, Kell MR, Flanagan FL, Kennedy M, Gorey TF, Kerin MJ. Role of sentinel lymph node biopsy in high-risk ductal carcinoma in situ patients. Am J Surg. 2007. 194:172–175.
15. Mittendorf EA, Arciero CA, Gutchell V, Hooke J, Shriver CD. Core biopsy diagnosis of ductal carcinoma in situ: an indication for sentinel lymph node biopsy. Curr Surg. 2005. 62:253–257.
16. Hoorntje LE, Schipper ME, Peeters PH, Bellot F, Storm RK, Borel Rinkes IH. The finding of invasive cancer after a preoperative diagnosis of ductal carcinoma-in-situ: causes of ductal carcinoma in-situ underestimates with stereotactic 14-gauge needle biopsy. Ann Surg Oncol. 2003. 10:748–753.
17. Renshaw AA. Predicting invasion in the excision specimen from breast core needle biopsy specimens with only ductal carcinoma in situ. Arch Pathol Lab Med. 2002. 126:39–41.
18. Cox CE, Nguyen K, Gray RJ, Salud C, Ku NN, Dupont E, et al. Importance of lymphatic mapping in ductal carcinoma in situ (DCIS): why map DCIS. Am Surg. 2001. 67:513–519.
19. Lee CH, Carter D, Philpotts LE, Couce ME, Horvath LJ, Lange RC, et al. Ductal carcinoma in situ diagnosed with stereotactic core needle biopsy: can invasion be predicted. Radiology. 2000. 217:466–470.
20. Silverstein MJ, Poller DN, Waisman JR, Colburn WJ, Barth A, Gierson ED, et al. Prognostic classification of breast ductal carcinoma-in-situ. Lancet. 1995. 345:1154–1157.
21. Pendas S, Dauway E, Giuliano R, Ku N, Cox CE, Reintgen DS. Sentinel node biopsy in ductal carcinoma in situ patients. Ann Surg Oncol. 2000. 7:15–20.
22. Farkas EA, Stolier AJ, Teng SC, Bolton JS, Fuhrman GM. An argument against routine sentinel node mapping for DCIS. Am Surg. 2004. 70:13–17.
23. Veronesi P, Intra M, Vento AR, Naninato P, Caldarella P, Paganelli G, et al. Sentinel lymph node biopsy for localised ductal carcinoma in situ? Breast. 2005. 14:520–522.
24. Klauber-DeMore N, Tan LK, Liberman L, Kaptain S, Fey J, Borgen P, et al. Sentinel lymph node biopsy: is it indicated in patients with high-risk ductal carcinoma-in-situ and ductal carcinoma-in-situ with microinvasion? Ann Surg Oncol. 2000. 7:636–642.
25. Katz A, Gage I, Evans S, Shaffer M, Fleury T, Smith FP, et al. Sentinel lymph node positivity of patients with ductal carcinoma in situ or microinvasive breast cancer. Am J Surg. 2006. 191:761–766.
26. Lara JF, Young SM, Velilla RE, Santoro EJ, Templeton SF. The relevance of occult axillary micrometastasis in ductal carcinoma in situ: a clinicopathologic study with long-term follow-up. Cancer. 2003. 98:2105–2113.
27. Ansari B, Ogston SA, Purdie CA, Adamson DJ, Brown DC, Thompson AM. Meta-analysis of sentinel node biopsy in ductal carcinoma in situ of the breast. Br J Surg. 2008. 95:547–554.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download